Virotherapy
Virotherapy is a treatment using biotechnology to convert viruses into therapeutic agents by reprogramming viruses to treat diseases. There are three main branches of virotherapy: anti-cancer oncolytic viruses, viral vectors for gene therapy and viral immunotherapy. These branches utilize three different types of treatment methods: gene overexpression, gene knockout, and suicide gene delivery. Gene overexpression adds genetic sequences that compensate for low to zero levels of needed gene expression. Gene knockout utilizes RNA methods to silence or reduce expression of disease-causing genes. Suicide gene delivery introduces genetic sequences that induce an apoptotic response in cells, usually to kill cancerous growths.[1] In a slightly different context, virotherapy can also refer more broadly to the use of viruses to treat certain medical conditions by killing pathogens.
| Virotherapy | |
|---|---|
| Specialty | virology |
Oncolytic virotherapy
Oncolytic virotherapy is not a new idea – as early as the mid 1950s doctors were noticing that cancer patients who suffered a non-related viral infection, or who had been vaccinated recently, showed signs of improvement;[2] this has been largely attributed to the production of interferon and tumour necrosis factors in response to viral infection, but oncolytic viruses are being designed that selectively target and lyse only cancerous cells.
In the 1940s and 1950s, studies were conducted in animal models to evaluate the use of viruses in the treatment of tumours.[3] In the 1940s–1950s some of the earliest human clinical trials with oncolytic viruses were started.[4][5]
In 2015 the FDA approved the marketing of talimogene laherparepvec, a genetically engineered herpes virus, to treat melanoma lesions that cannot be operated on; it is injected directly into the lesion.[6] As of 2016 there was no evidence that it extends the life of people with melanoma, or that it prevents metastasis.[7] Two genes were removed from the virus – one that shuts down an individual cell's defenses, and another that helps the virus evade the immune system – and a gene for human GM-CSF was added. The drug works by replicating in cancer cells, causing them to burst; it was also designed to stimulate an immune response but as of 2016, there was no evidence of this.[8][6] The drug was created and initially developed by BioVex, Inc. and was continued by Amgen, which acquired BioVex in 2011.[9] It was the first oncolytic virus approved in the West.[8]
Viral gene therapy
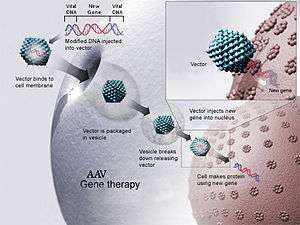
Viral gene therapy uses genetically engineered viral vectors to deliver therapeutic genes to cells with genetic malfunctions[10]. Typically, the virus is administered to patients intravenously or by direct injection into target tissues[10]. The molecular mechanisms of gene delivery and/or integration into cells vary based on the viral vector that is used[10].
There are many targets of viral gene therapy. While some therapies target the missing or mutated genes of inherited genetic disorders, others seek to deliver new genes to cancer cells in order to destroy tumors[11][12].
Currently, immune responses to viral gene therapies pose a challenge to successful treatment[13]. However, responses to viral vectors at immune privileged sites such as the eye may be reduced compared to other sites of the body[13][14].
Viral immunotherapy
Unlike traditional vaccines, in which attenuated or killed virus/bacteria is used to generate an immune response, viral immunotherapy uses genetically engineered viruses to present a specific antigen to the immune system. That antigen could be from any species of virus/bacteria or even human disease antigens, for example cancer antigens.
Vaccines are another method of virotherapy that use attenuated or inactivated viruses to develop immunity to disease. An attenuated virus is a weakened virus that incites a natural immune response in the host that is often undetectable. The host also develops potentially life-long immunity due to the attenuated virus’s similarity to the actual virus. Inactivated viruses are killed viruses that present a form of the antigen to the host. However, long-term immune response is limited.[15]
There are two general approaches to develop these viruses using applied evolutionary techniques: Jennerian and Pastorian. The Jennerian method involves selecting similar viruses from non-human organisms to protect against a human virus while Pastorian methods use serial passage. This Pastorian method is very similar to directive evolution of oncolytic viruses. Selected viruses that target humans are passed through multiple non-human organisms for multiple generations. Over time the viruses adapt to the foreign environments of their new hosts. These now maladapted viruses have minimal capacity for harming humans and are used as attenuated viruses for clinical use.[16] An important consideration is to not reduce the replicative ability of the virus beyond the point where the immune system response will be compromised. A secondary immune response would therefore be insufficient to provide protection against the live virus should it be reintroduced to the host.
Specific projects and products
Oncolytic viruses
RIGVIR is a virotherapy drug that was approved by the State Agency of Medicines of the Republic of Latvia in 2004.[17] It is wild type ECHO-7, a member of echovirus family.[18] The potential use of echovirus as an oncolytic virus to treat cancer was discovered by Latvian scientist Aina Muceniece in the 1960s and 1970s.[18] The data used to register the drug in Latvia is not sufficient to obtain approval to use it in the US, Europe, or Japan.[18][19] As of 2017 there was no good evidence that RIGVIR is an effective cancer treatment.[20][21] On March 19th, 2019, the manufacturer of ECHO-7, SIA LATIMA, announced the drug's removal from sale in Latvia, quoting financial and strategic reasons and insufficient profitability.[22] However, several days later an investigative TV show revealed that State Agency of Medicines had run laboratory tests on the vials, and found that the amount of ECHO-7 virus is of a much smaller amount than claimed by the manufacturer. According to agency's lab director, "It's like buying what you think is lemon juice, but finding that what you have is lemon-flavored water". In March 2019, the distribution of ECHO-7 in Latvia has been stopped. [23]
Viral gene therapy
Currently, there are many viral gene therapy products in clinical trial phases. Listed below are the products that are (or were) approved for marketing in the US and/or European Union.
- In 2012 the European Commission approved Glybera, an AAV vector-based gene therapy product for the treatment of lipoprotein lipase deficiency in adults.[24] It was the first gene therapy approved in the EU.[25] The drug never received FDA approval in the US, and was discontinued by its manufacturer uniQure in 2017 due to profitability concerns.[26] As of 2019 it is no longer authorized for use in the EU.[24]
- In 2017, the FDA approved Spark Therapeutics' Luxturna, an AAV vector-based gene therapy product for the treatment of RPE65 mutation-associated retinal dystrophy in adults.[27][28] Luxturna is the first gene therapy approved in the US for the treatment of a monogenetic disorder.[27][29] It has been authorized for use in the EU since 2018.[30]
- In 2019, the FDA approved Zolgensma, an AAV vector-based gene therapy product for the treatment of spinal muscular atrophy in children under the age of two.[31]. As of August 2019, it is the world's most expensive treatment, at a cost of over two million USD.[32] Novartis is still seeking marketing approval for the drug in the EU as of 2019.[32]
Protozoal virotherapy
Viruses have been explored as a means to treat infections caused by protozoa.[33][34] One such protozoa that potential virotherapy treatments have explored is Naegleria fowleri which causes primary amebic meningoencephalitis (PAM). With a mortality rate of 95%, this disease-causing eukaryote has one of the highest pathogenic fatalities known. Chemotherapeutic agents that target this amoeba for treating PAM have difficulty crossing blood-brain barriers. However, the driven evolution of virulent viruses of protozoal pathogens (VVPPs) may be able to develop viral therapies that can more easily access this eukaryotic disease by crossing the blood-brain barrier in a process analogous to bacteriophages. These VVPPs would also be self-replicating and therefore require infrequent administration with lower doses, thus potentially reducing toxicity. [35] While these treatment methods for protozoal disease may show great promise in a manner similar to bacteriophage viral therapy, a notable hazard is the evolutionary consequence of using viruses capable of eukaryotic pathogenicity. VVPPs will have evolved mechanisms of DNA insertion and replication that manipulate eukaryotic surface proteins and DNA editing proteins. VVPP engineering must therefore control for viruses that may be able to mutate and thereby bind to surface proteins and manipulate the DNA of the infected host.
History
Chester M. Southam, a researcher at Memorial Sloan Kettering Cancer Center, pioneered the study of viruses as potential agents to treat cancer.[36]
See also
- Cancer
- Gene therapy
- Oncolytic virus
- Vector
- Virosome, using modified viruses for drug delivery
References
- Stephen, Sam. "How Science Is Using Viruses To Make You Better - CPI". CPI. Retrieved 31 October 2018.
- Kelly, E; Russell, SJ (April 2007). "History of oncolytic viruses: genesis to genetic engineering". Molecular Therapy. 15 (4): 651–9. doi:10.1038/sj.mt.6300108. PMID 17299401.
- Moore, AE (May 1949). "The destructive effect of the virus of Russian Far East encephalitis on the transplantable mouse sarcoma 180". Cancer. 2 (3): 525–34. doi:10.1002/1097-0142(194905)2:3<525::AID-CNCR2820020317>3.0.CO;2-O. PMID 18131412.
- "Clinical virotherapy: four historically significant clinical trials".
- Huebner, RJ; Rowe, WP; Schatten, WE; Smith, RR; Thomas, LB (Nov–Dec 1956). "Studies on the use of viruses in the treatment of carcinoma of the cervix". Cancer. 9 (6): 1211–8. doi:10.1002/1097-0142(195611/12)9:6<1211::AID-CNCR2820090624>3.0.CO;2-7. PMID 13383455.
- Fukuhara, H; Ino, Y; Todo, T (3 August 2016). "Oncolytic virus therapy: A new era of cancer treatment at dawn". Cancer Science. 107 (10): 1373–1379. doi:10.1111/cas.13027. PMC 5084676. PMID 27486853.
- "Imlygic label" (PDF). FDA. October 2015. Retrieved 16 October 2016. For label updates see FDA index page for BLA 125518
- Bilsland, AE; Spiliopoulou, P; Evans, TR (2016). "Virotherapy: cancer gene therapy at last?". F1000Research. 5: 2105. doi:10.12688/f1000research.8211.1. PMC 5007754. PMID 27635234.
- "Amgen to Buy BioVex, Maker of Cancer Drugs". Bloomberg News via The New York Times. 24 January 2011.
- "How does gene therapy work?". U.S. National Library of Medicine: Genetics Home Reference. Retrieved 2019-12-05.
- "Gene therapy - Mayo Clinic". www.mayoclinic.org. Retrieved 2019-12-05.
- Cross, Deanna; Burmester, James K. (2006). "Gene Therapy for Cancer Treatment: Past, Present and Future". Clinical Medicine and Research. 4 (3): 218–227. ISSN 1539-4182. PMC 1570487. PMID 16988102.
- Bessis, N.; GarciaCozar, F. J.; Boissier, M.-C. (2004). "Immune responses to gene therapy vectors: influence on vector function and effector mechanisms". Gene Therapy. 11 (1): S10–S17. doi:10.1038/sj.gt.3302364. ISSN 1476-5462.
- Zhou, Ru; Caspi, Rachel R (2010-01-18). "Ocular immune privilege". F1000 Biology Reports. 2. doi:10.3410/B2-3. ISSN 1757-594X. PMC 2948372. PMID 20948803.
- Services, U.S. Department of Health and Human. "Vaccines.gov". www.vaccines.gov.
- Hanley, KA (December 2011). "The double-edged sword: How evolution can make or break a live-attenuated virus vaccine". Evolution. 4 (4): 635–643. doi:10.1007/s12052-011-0365-y. PMC 3314307. PMID 22468165.
- "Latvijas Zāļu reģistrs". www.zva.gov.lv. Retrieved 2017-12-17.
- Babiker, HM; Riaz, IB; Husnain, M; Borad, MJ (2017). "Oncolytic virotherapy including Rigvir and standard therapies in malignant melanoma". Oncolytic Virotherapy. 6: 11–18. doi:10.2147/OV.S100072. PMC 5308590. PMID 28224120.
- "Feasibility study for registration of medicine RIGVIR with the European Medicine Agency". European Commission. 2016-01-08. Archived from the original on 2016-11-02. Retrieved 2016-11-02.
However, further use and commercialisation in the EU is prevented as EU regulations require cancer medicines to be registered centrally through the European Medicine Agency (EMA). National registrations are not considered.
- Gorski D (18 September 2017). "Rigvir: Another unproven and dubious cancer therapy to be avoided". Science-Based Medicine.
- Gorski, David (25 September 2017). "Ty Bollinger's "The Truth About Cancer" and the unethical marketing of the unproven cancer virotherapy Rigvir". Science-Based Medicine.
- "Rigvir medication distribution in Latvia halted temporarily".
- "Rigvir cancer treatment at center of fresh controversy".
- "Glybera: EPAR - Summary for the public" (PDF). European Medicines Agency. Retrieved 2019-11-25.
- Gallagher, James (2012-11-02). "Gene therapy: Glybera approved by European Commission". BBC News. Retrieved 2019-11-25.
- "uniQure Announces It Will Not Seek Marketing Authorization Renewal for Glybera in Europe" (PDF). uniQure. Retrieved 2019-11-25.
- "FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss". U.S. Food & Drug Administration. 2017-12-18. Retrieved 2019-11-25.
- "Package Insert - LUXTURNA (voretigene neparvovec-rzyl)" (PDF). U.S. Food & Drug Administration. Retrieved 2019-11-25.
- Stein, Rob (2017-12-19). "First Gene Therapy For Inherited Disease Gets FDA Approval". NPR.org. Retrieved 2019-11-26.
- "Luxturna : EPAR - Medicine overview" (PDF). European Medicines Agency. Retrieved 2019-11-25.
- "Package Insert - ZOLGENSMA" (PDF). U.S. Food & Drug Administration. Retrieved 2019-11-25.
- Erman, Michael (2019-08-07). "Novartis says it knew of Zolgensma data problems before U.S. approval". Reuters. Retrieved 2019-11-26.
- Keen, E. C. (2013). "Beyond phage therapy: Virotherapy of protozoal diseases". Future Microbiology. 8 (7): 821–823. doi:10.2217/FMB.13.48. PMID 23841627.
- Hyman, P.; Atterbury, R.; Barrow, P. (2013). "Fleas and smaller fleas: Virotherapy for parasite infections". Trends in Microbiology. 21 (5): 215–220. doi:10.1016/j.tim.2013.02.006. PMID 23540830.
- Keen, Eric C (July 2013). "Beyond phage therapy: virotherapy of protozoal diseases". Future Microbiology. 8 (7): 821–823. doi:10.2217/fmb.13.48.
- Sepkowitz, Kent (24 August 2009). "West Nile Made Its U.S. Debut in the 1950s, in a Doctor's Syringe". The New York Times. p. D5.
Further reading
- Ring, Christopher J. A.; Blair, Edward D. (2000). Genetically engineered viruses: development and applications. Oxford: Bios. ISBN 978-1859961032. OCLC 45828140.