Trapeziometacarpal osteoarthritis
Trapeziometacarpal osteoarthritis, also known as osteoarthritis at the base of the thumb or as rhizarthrosis, is a reparitive joint disease affecting the first carpometacarpal joint (CMC1).[1] This joint is formed by the trapezium bone of the wrist and the first metacarpal bone of the thumb. Because of its relative instability, this joint is a frequent site for osteoarthritis.[2] Carpometacarpal osteoarthritis (CMC OA) of the thumb occurs when the cushioning cartilage of the joint surfaces wears away, resulting in damage of the joint.[1][3]
| Trapeziometacarpal osteoarthritis | |
|---|---|
| Other names | Carpometacarpal (CMC) osteoarthritis (OA) of the thumb, osteoarthritis at the base of the thumb |
 | |
| Osteoarthritis of the first carpometacarpal joint | |
| Specialty | Plastic surgery |
The main complaint of patients is pain.[4][5] Pain at the base of the thumb occurs when moving the thumb and might eventually persist at rest.[4][5] Other symptoms include stiffness, swelling and loss of strength of the thumb.[4][5] Treatment options include conservative and surgical therapies.[6]
Signs and symptoms
The primary and most common symptom in patients with CMC OA of the thumb is pain.[5] Pain at the base of the thumb is mainly experienced when moving the thumb or when applying pressure with the thumb. However, in advanced stages of CMC OA, pain might persist at rest. Another prominent symptom is loss of strength of the thumb.[5] Patients struggle to grab or hold an object due to weakening of the thumb. For example, tying a knot or holding a saucepan becomes increasingly difficult.
If patients present themselves with similar symptoms, physicians should also consider De Quervain syndrome, rheumatoid arthritis or flexor carpi radialis and flexor pollicis longus tendinopathy as a possible cause.[7]
Typical signs of CMC OA can be observed from the outside of the hand.[5] For example, the area near the base of the thumb can be swollen and could appear inflamed. Advanced stages of CMC OA can eventually lead to deformity of the thumb. This deformity, also called a ‘zigzag’ deformity, is characterized by a deviation of the thenar eminence towards the middle of the hand, whilst the thumb phalanges overextend.[8] Also a grinding sound, known as crepitus, can be heard when the CMC1 joint is moved.[6]
Causes
CMC OA of the thumb is a degenerative joint disease.[1] Although the exact cause remains unclear, there is a general consensus among researchers about some of the mechanisms leading to CMC OA of the thumb.[9]
It is believed that laxity of the ligaments surrounding the CMC1 joint is the main cause of CMC OA.[10] Especially laxity of the most significant ligament, the palmar beak ligament, will lead to joint instability.[10] This instability causes misalignment of the joint bones, which will then rub against each other. As a consequence, the cushioning cartilage, which covers the surfaces of the joint bones, wears down.[1] The synovial membranes get irritated and synovitis occurs. Eventually, the bare surfaces of the joint bones are exposed to each other. The gap between the joint bones decreases, as there is hardly any cartilage left.
In reaction of this process the joint bones thicken at the surface, resulting in subchondral sclerosis. Also bony outgrowths, called osteophytes, are formed at the joint margins.[11]
In advanced stages of CMC OA, misalignment of the joint bones causes the tendons attached to thumb to force the base of the thumb into radial deviation and extension and the thumb phalanges in hyperextension. As a consequence the ‘zigzag’ deformity becomes visible.[8]
The large forces, which the CMC1 joint has to withstand, are considered to be another cause of CMC OA.[12] During daily manual activities, such as grabbing and pinching, the thumb is constantly being used. The forces generated by these movements have an enlarged impact on the CMC1 joint because of the leverage within the thumb. This makes the joint even more sensitive to wear and tear.[12]

Risk factors
Several risk factors of CMC OA of the thumb are known. Each of these risk factors does not cause CMC OA by itself, but acts as a predisposing factor influencing the process of OA in some way. Risk factors include: female gender,[2] suffering from obesity,[13] repetitive heavy manual labor,[14] familial predisposition and hormonal changes, such as menopause.[15]
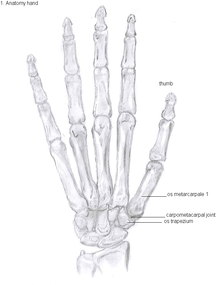
Anatomy
The CMC1 joint is a synovial joint between the trapezium bone of the wrist and the metacarpal bone at the base of the thumb. This joint is a so-called saddle joint (articulatio sellaris), unlike the CMC joints of the other four fingers which are ellipsoid joints.[16] This means that the surfaces of the CMC1 joint are both concave and convex.
Because of its specific shape, the CMC1 joint allows a wide range of motion of the thumb. Movements possible in this CMC1 joint are:[17]
- Flexion
- Extension
- Abduction
- Adduction
- Opposition
- Reposition
- Circumduction
This high mobility is due to the little intrinsic osseous stability of the joint. This causes the CMC1 joint to be more unstable compared to the CMC joints of the other fingers.[18] Because of this instability, the joint is more susceptible to be damaged.[12] To remain stable the CMC1 joint has to rely on the surrounding ligaments for support. These ligaments provide the ability to subject high pressure loads, particularly during pinch and grasp manoeuvres.[19]
16 ligaments surrounding the CMC1 joint are identified, which give strength and stability to the joint. Of these ligaments, the deep anterior oblique ligament, also known as the palmar beak ligament, is considered to be the most important stabilizing ligament.[20]
Diagnosis
CMC OA is diagnosed based on clinical findings and radiologic imaging.[5]
Classification
CMC OA can be divided into different stages which show the progression of the disease. The most commonly used classification is the radiological staging protocol according to Eaton and Littler. Four different stages are distinguished on radiological evidence of synovitis, joint space and capsular laxity.[15][21]
Stage 1:
- "synovitis phase"
- slight widening of the joint space
- articular contours are normal
- < 1/3 subluxation of the joint (in any projection)
Stage 2:
- There is a significant capsular laxity
- 1/3 subluxation of the joint
- Osteophytes, < 2 mm in diameter, are present. (usually adjacent to the volar or dorsal facets of the trapezium)
Stage 3:
- > 1/3 subluxation of the joint
- Osteophytes, > 2 mm in diameter, are present (usually adjacent to the volar and dorsal facets of the trapezium)
- Slight joint space narrowing

Stage 4:
- Major subluxation of the joint.
- Very narrow joint space
- Cystic and sclerotic subchondral bone changes are present
- Significant erosion of the scaphotrapezial joint.
Treatment
Conservative
There is moderate quality evidence that manual therapy and therapeutic exercise improves pain in patients with thumb CMC OA at both short- and intermediate-term follow-up, and low to moderate quality evidence that magneto therapy improves pain and function at short-term follow-up. There is moderate evidence that orthoses (splints) can improve hand function at long-term follow-up. There is very low to low-quality evidence that other conservative interventions provide no significant improvement in pain and in function at short- and long-term follow-up. Some of the commonly performed conservative interventions performed in therapy have evidence to support their use to improve hand function and decrease hand pain in patients with CMC OA. [22] Patients with CMC OA of the thumb should initially be treated conservatively. Conservative treatment is equal to any non-surgical treatment and includes splinting, manual therapy, therapeutic exercises, magneto therapy, laser, NSAID medication and injections with corticosteroids.[23]
Manual therapy
Manual therapy is another commonly used treatment modality in which the joints or muscles of patients are manipulated with the intention of restoring the range of motion of the joint or increasing the flexibility of the muscles around the joint. Intervention techniques:
Kaltenborn mobilization technique
The specific Kaltenborn mobilization of posterior-anterior gliding with distraction in grade 3 of the CMC joint; the Convex/Concave Rule was applied in each case. In brief, Kaltenborn described these mechanics in terms of the convex-concave rule; the direction of decreased joint gliding in a hypomobile joint and, thus, the appropriate treatment can be deduced by this rule. With movement of a concave joint partner, the glide occurs in the same direction. The form of the joint surface has been considered to induce its gliding/sliding movement; a female (concave) joint surface glides in the same direction as the bone movement, whereas a male (convex) surface glides in the opposite direction of the bone movement. Traction is the technique that distracts 1 articular surface perpendicular to the other, and the glide technique describes the translational gliding of 1 articular surface parallel to the other. Traction in grade 3 has been defined as an additional force, which is applied in the parallel axis. This results in surrounding soft tissues and joint stretching, separating the joint surfaces.[24][29]
Neural mobilization technique
Nerve mobilization aims to glide a nerve by alternating moving at least two joints to increase in nerve strain due to nerve bed elongation at one joint (e.g., wrist extension) is simultaneously counterbalanced by a decrease in nerve bed length at an adjacent joint (e.g., elbow flexion).[30] The nerve mobilization technique for the median nerve consists of alternating the combination of elbow extension (which increases tension on the median nerve) and wrist flexion (which decreases tension on the median nerve) movement with the combination of elbow flexion (decreasing tension) and wrist extension (increasing tension) movement.[30] The radial nerve mobilization involves alternating the following 2 movements: shoulder depression applied simultaneously with elbow flexion and wrist flexion and ulnar deviation wrist extension; and shoulder elevation simultaneously with elbow extension, wrist extension. These movements can be alternated at a rate of approximately 2 seconds per cycle (1 second into extension and 1 second into flexion). Speed and amplitude of movement is adjusted to ensure that no pain was produced. At each session, the technique can be applied 3 times for 3 min separated by 1-min rest periods.[28]
Surgery
If conservative treatment does not reduce the complaints of patients, surgical treatment is indicated.[8] This might be the case when pain persists or when functional disability remains present after conservative treatment.
There are several surgical options to treat CMC OA of the thumb.[31] The aim of the treatment is not to cure the disease but to minimize the complaints and symptoms of patients.
Because many different expert opinions about the surgical treatment exist, there are many varieties of surgery, even within one type of surgery. However, there are four types of surgical techniques that are most commonly used.[31] These techniques can be categorized as follows:
- Trapeziectomy
- Arthrodesis
- Joint replacement
- Metacarpal osteotomy
Throughout the years many clinical trials have been carried out, investigating which surgical technique is superior. The levels of evidence of these studies vary from case reports up to randomized controlled trials and systematic reviews. Most studies focused on levels of pain, strength of the thumb, thumb mobility, satisfaction and complications.
No significant evidence has been found to claim that one of the four treatments is superior to one of the others in both short- and long-term effect.[31] Further investigation is needed, but until new evidence is found, investigators advice to carry out the most simple treatment with the least amount of complications. This means that the trapeziectomy is the most recommended surgical procedure for now.[31]

Types of trapeziectomy
The principle of this procedure is the removal of the trapezium bone. It was originally described by Gervis in 1949 [24]. Because half of the carpometacarpal joint is removed, the complaints of patients caused by OA are usually gone.
Four main varieties within this procedure are performed:[32]
- Trapeziectomy
- Trapeziectomy with tendon interposition (TI)
- Trapeziectomy with ligament reconstruction (LR)
- Trapeziectomy with a combination of ligament reconstruction and tendon interposition (LRTI)
Claims have been made that one of these procedures is superior to the others, but there is no scientific evidence to support these statements.[33]
When pain, grip strength and key and tip pinch strengths were examined, investigators could not find a significant difference between the different procedures.[33]
Investigators suggest that the trapeziectomy without any interposition or reconstruction is preferred. It is a simpler procedure then the trapeziectomy with TI or LR and it tends to have fewer complications than the trapeziectomy with LRTI.[31][33]
Trapeziectomy is considered a good surgical option to treat stage II to IV of CMC OA of the thumb.[33]
Trapeziectomy
The most simple form out of the four variations is the trapeziectomy alone, also referred as the simple trapeziectomy.[32] During this procedure, the trapezium bone is removed without any further surgical adjustments.
The trapezium bone will be removed through an approximately three centimeter long incision along the lateral side of the thumb. To preserve surrounding structures, the trapezium bone will be removed through fragmentation of the bone (the bone will therefore be broken into pieces).
An empty gap is left by the trapeziectomy and the wound is closed with sutures. Despite this gap, no significant changes in function of the thumb are reported.[31] After the surgery, the thumb will be immobilized with a cast.
Trapeziectomy with TI
Some physicians still believe that it is better to fill the gap left by the trapeziectomy. They assume that filling the gap with a part of a tendon is preferable in terms of function, stability and position of the thumb. They are afraid that leaving a gap might result in complications such as shortening or subluxation of the thumb.
During trapeziectomy with TI, a tendon interposition is performed.[34] A longitudinal strip of the palmaris longus tendon is separated. If this tendon is absent (which is the case in 13% of the population), half of the flexor carpi radialis tendon (FCR) can be used.
The tendon is then formed into a circular shape and placed in the gap, where it will be stabilized by sutures.[8]
Trapeziectomy with LR
Another technique used to assumable restore stability of the thumb, is a ligament reconstruction after a trapeziectomy is performed. The thought is that ligament reconstruction provides more stability to the thumb after removal of the trapezium bone.[35]
During this procedure the anterior oblique ligament is reconstructed using the FCR tendon. There is a wide variety in techniques to perform this LR, but they all have a similar goal.

Trapeziectomy with LRTI
Some physicians suppose that combining LR with TI results in an even better stabilised thumb.
Like the name already suggests, this procedure includes a combination of a trapeziectomy with a LR as well as a TI.[36]
Arthrodesis
Arthrodesis of the CMC1 joint is a surgical procedure in which the trapezium bone and the metacarpal bone of the thumb are secured together. Because the joint is fixed, and therefore can not be moved, the complaints of the patient are mainly gone.
During the surgery the two bones will be fixated using K-wires. The use of plates and screws has also been described. The thumb will be positioned in a way it can still perform a pinch grip. Because of the fixation, the two bones will fuse together. This will occur usually within four to six weeks.
However, this technique has some disadvantages.[31] The palm of the hand is unable to be flattened, making it difficult to wear gloves or put your hand in a pocket. Because the stress on the CMC1 joint is now divided over the other joints, those joints are more likely to be damaged.[37]
Nevertheless, this procedure can be used in patients with stage II and III CMC OA as well as in young people with posttraumatic OA.[31]
Joint Replacement
There are several prostheses available for use although they have not been widely successful. The goal is to create a stable artificial joint by replacing the old affected joint with new material. Newer prostheses tend to have better results than older ones.[31] Prostheses come in many varieties, such as spacers or resurfacing prostheses.
The total CMC1 joint replacement is a newer arthroplasty which has developed into a cemented and a non-cemented design. The cement acts as a binding factor for fixation of the prosthesis to the host bone. The non-cemented procedure is a good option to treat stage II and III OA and could be better on short-term than the trapeziectomy with LRTI. However, on the longer term, literature indicates the contrary.[31]
Overall, joint replacements are related to long-term complications such as subluxation, fractures, synovitis (due to the material used) and nerve damaging.[38] In many cases revision surgery is needed to either remove or repair the prosthesis. Also note that usage of a joint replacement is heavy in costs.
The quality of the prostheses is improving and there is reason to believe this will have a positive effect on outcome in the years to follow.[31]

Metacarpal osteotomy
The aim of this procedure is to change the pressure distribution on the CMC1 joint, so it can function without further damaging the joint. That is why a successful osteotomy requires a CMC1 joint of reasonable condition. Therefore, the metacarpal osteotomy should be limited to patients with a stage I-II CMC OA.[39]
An osteotomy is a surgical procedure wherein bone fragments are modified by cutting the bone.
During this procedure an abduction osteotomy of the proximal end of the first metacarpal bone is performed. An incision is made over the radial border of the first metacarpal bone. A wedged shape bone fragment is removed, causing the distal part of the metacarpal bone to tilt towards its desired position.[40] Postoperative, the thumb of the patient is immobilized using a thumb-cast.
Possible complications are non-union of the bone, persistent pain related to unrecognized CMC or pantrapezial disease and radial sensory nerve injury.[39]
Complications
The most common complication after surgery is pain persisting in the thumb. Over long term, there is pain relief, but on short term, patients experience pain from the surgery itself. The main complaint is a burning sensation or hypersensitivity over the incision. Some patients develop a complex regional pain syndrome. This is a syndrome of chronic pain with changes of temperature and colour of the skin.
Other general complications include radial nerve damage and postoperative wound infection.
After arthrodesis, non-union, in which fusion of the trapezium bone with the metacarpal bone fails, occurs in 8% to 21% of the cases.[31]
Subluxation of a prosthesis is a complication where the prosthesis is mobile and is partially dislocated. When the prosthesis is fully dislocated it is called a luxation. Both are painful and need revision surgery so the prosthesis can be repaired or removed.[41] When using a prosthesis over a longer period of time, there is a chance of breaking the prosthesis itself. This is due to mechanical wear.
Prostheses might also cause a reaction of the body against the artificial material they are made of, resulting in local inflammation.
Epidemiology
CMC OA is the most common form of OA affecting the hand.[2] Dahaghin et al. showed that about 15% of women and 7% of men between 50 and 60 years of age suffer from CMC OA of the thumb.[42] However, in about 65% of people older than 55 years, radiologic evidence of OA was present without any symptoms.[42] Armstrong et al. reported a prevalence of 33% in postmenopausal women, of which one third was symptomatic, compared to 11% in men older than 55 years.[2] This shows CMC OA of the thumb is significantly more prevalent in women, especially in postmenopausal women, compared to men.
References
- Pelligrini VD (November 1991). "Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. II. Articular wear patterns in the osteoarthritic joint". J Hand Surg Am. 16 (6): 975–82. doi:10.1016/S0363-5023(10)80055-3. PMID 1748768.
- Armstrong AL, Hunter JB, Davis TRC (1994). "The prevalence of reparative arthritis of the base of the thumb in post-menopausal women". J Hand Surg. 19B (3): 340–341. doi:10.1016/0266-7681(94)90085-X. PMID 8077824.
- Kihara H (April 1992). "[Anatomical study of the normal and degenerative articular surfaces on the first carpometacarpal joint]". Nippon Seikeigeka Gakkai Zasshi (in Japanese). 66 (4): 228–39. PMID 1593195.
- Burton R. I. "Basal joint arthrosis of the thumb". Orthop. Clin. North Am. 4 (347): 1973.
- Glickel SZ (May 2001). "Clinical assessment of the thumb trapeziometacarpal joint". Hand Clin. 17 (2): 185–95. PMID 11478041.
- Carr M. M., Freiberg A. "Osteoarthritis of the thumb: Clinical aspects and management". Am. Fam. Physician. 50 (995): 1994.
- Orthopedie, second edition, Bohn Stafleu van Loghum, ISBN 9031348619.
- Ghavami A, Oishi SN (May 2006). "Thumb trapeziometacarpal arthritis: treatment with ligament reconstruction tendon interposition arthroplasty". Plast. Reconstr. Surg. 117 (6): 116e–128e. doi:10.1097/01.prs.0000214652.31293.23. PMID 16651933.
- Pellegrini VD (May 2001). "Pathomechanics of the thumb trapeziometacarpal joint". Hand Clin. 17 (2): 175–84, vii–viii. PMID 11478040.
- Doerschuk SH, Hicks DG, Chinchilli VM, Pellegrini VD (May 1999). "Histopathology of the palmar beak ligament in trapeziometacarpal osteoarthritis". J Hand Surg Am. 24 (3): 496–504. doi:10.1053/jhsu.1999.0496. PMID 10357527.
- North ER, Eaton RG (March 1983). "Degenerative joint disease of the trapezium: a comparative radiographic and anatomic study". J Hand Surg Am. 8 (2): 160–6. doi:10.1016/s0363-5023(83)80008-2. PMID 6833724.
- Cooney WP, Chao EY (January 1977). "Biomechanical analysis of static forces in the thumb during hand function". J Bone Joint Surg Am. 59 (1): 27–36. doi:10.2106/00004623-197759010-00004. PMID 833171.
- Dahaghin S, Bierma-Zeinstra SM, Koes BW, Hazes JM, Pols HA (July 2007). "Do metabolic factors add to the effect of overweight on hand osteoarthritis? The Rotterdam Study". Ann. Rheum. Dis. 66 (7): 916–20. doi:10.1136/ard.2005.045724. PMC 1955104. PMID 17314121.
- Jensen JC, Sherson D (September 2007). "Work-related bilateral osteoarthritis of the first carpometacarpal joints". Occup Med (Lond). 57 (6): 456–60. doi:10.1093/occmed/kqm029. PMID 17698839.
- Tomaino, M. M. Thumb basal joint arthritis. In D. P. Green et al. (Eds.), Green’s Operative Hand Surgery, 5th Ed. New York: Churchill Livingstone, 2005. Pp. 461–485.
- Sobotta Anatomy, 14th ed., Elsevier, ISBN 9780702034831
- Gray’s Anatomy for Students, second edition, Elsevier, ISBN 9780443069529
- Pomerance JF (May 1995). "Painful basal joint arthritis of the thumb. Part I: Anatomy, pathophysiology, and diagnosis". Am. J. Orthop. 24 (5): 401–8. PMID 7620862.
- Bettinger PC, Linscheid RL, Berger RA, Cooney WP, Kai-Nan A (1999). "An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint". J Hand Surg [Am]. 24 (4): 786–798. doi:10.1053/jhsu.1999.0786. PMID 10447171.
- Pellegrini VD, Olcott CW, Hollenberg G (March 1993). "Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament". J Hand Surg Am. 18 (2): 238–44. doi:10.1016/0363-5023(93)90354-6. PMID 8463587.
- Eaton RG, Glickel SZ (November 1987). "Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment". Hand Clin. 3 (4): 455–71. PMID 3693416.
- Bertozzi, L; Valdes, K; Vanti, C; Negrini, S; Pillastrini, P; Villafañe, JH (5 January 2015). "Investigation of the effect of conservative interventions in thumb carpometacarpal osteoarthritis: systematic review and meta-analysis". Disability and Rehabilitation. 37 (22): 2025–2043. doi:10.3109/09638288.2014.996299. PMID 25559974.
- Valdes, Kristin; Marik, Tambra (October 2010). "A Systematic Review of Conservative Interventions for Osteoarthritis of the Hand". Journal of Hand Therapy. 23 (4): 334–351. doi:10.1016/j.jht.2010.05.001. PMID 20615662.
- Villafañe JH, Silva GB, Diaz-Parreño SA, Fernandez-Carnero J (October 2011). "Hypoalgesic and motor effects of kaltenborn mobilization on elderly patients with secondary thumb carpometacarpal osteoarthritis: a randomized controlled trial". J Manipulative Physiol Ther. 34 (8): 547–56. doi:10.1016/j.jmpt.2011.08.005. PMID 21899891.
- Villafañe JH, Silva GB, Fernandez-Carnero J (February 2012). "Effect of thumb joint mobilization on pressure pain threshold in elderly patients with thumb carpometacarpal osteoarthritis". J Manipulative Physiol Ther. 35 (2): 110–20. doi:10.1016/j.jmpt.2011.12.002. PMID 22257943.
- Villafañe JH, Bishop MD, Fernández-de-Las-Peñas C, Langford D (March 2013). "Radial nerve mobilisation had bilateral sensory effects in people with thumb carpometacarpal osteoarthritis: a randomised trial". J Physiother. 59 (1): 25–30. doi:10.1016/S1836-9553(13)70143-7. PMID 23419912.
- Villafañe JH, Silva GB, Fernandez-Carnero J (September 2011). "Short-term effects of neurodynamic mobilization in 15 patients with secondary thumb carpometacarpal osteoarthritis". J Manipulative Physiol Ther. 34 (7): 449–56. doi:10.1016/j.jmpt.2011.05.016. PMID 21875519.
- Villafañe JH, Silva GB, Bishop MD, Fernandez-Carnero J (March 2012). "Radial nerve mobilization decreases pain sensitivity and improves motor performance in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial". Arch Phys Med Rehabil. 93 (3): 396–403. doi:10.1016/j.apmr.2011.08.045. PMID 22218138.
- Villafañe JH, Fernandez de-Las-Peñas C, Silva GB, Negrini S (June 2014). "Contralateral sensory and motor effects of unilateral kaltenborn mobilization in patients with thumb carpometacarpal osteoarthritis: a secondary analysis". J Phys Ther Sci. 26 (6): 807–12. doi:10.1589/jpts.26.807. PMC 4085197. PMID 25013272.
- Coppieters MW, Alshami AM (Jul 2007). "Longitudinal excursion and strain in the median nerve during novel nerve gliding exercises for carpal tunnel syndrome" (PDF). J Orthop Res. 25 (7): 972–80. doi:10.1002/jor.20310. PMID 17415752.
- Vermeulen, Guus M.; Slijper, Harm; Feitz, Reinier; Hovius, Steven E.R.; Moojen, Thybout M.; Selles, Ruud W. (2011). "Surgical Management of Primary Thumb Carpometacarpal Osteoarthritis: A Systematic Review". The Journal of Hand Surgery. 36 (1): 157–169. doi:10.1016/j.jhsa.2010.10.028. ISSN 0363-5023. PMID 21193136.
- Gervis W.H. (1949). "Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint". J Bone Joint Surg. 31B (4): 537–539. doi:10.1302/0301-620X.31B4.537.
- Gangopadhyay S, McKenna H, Burke FD, Davis TR (March 2012). "Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition". J Hand Surg Am. 37 (3): 411–7. doi:10.1016/j.jhsa.2011.11.027. PMID 22305824.
- Weilby A (1988). "Tendon interposition arthroplasty of the first carpo-metacarpal joint". J Hand Surg [Br]. 13 (4): 421–425. doi:10.1016/0266-7681(88)90171-4.
- Blank J, Feldon P (1997). "Thumb metacarpophalangeal joint stabilization during carpometacarpal joint surgery". Atlas Hand Clin. 2: 217–225.
- Burton RI, Pellegrini VD (May 1986). "Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty". J Hand Surg Am. 11 (3): 324–32. doi:10.1016/s0363-5023(86)80137-x. PMID 3711604.
- Mureau MA, Rademaker RP, Verhaar JA, Hovius SE (September 2001). "Tendon interposition arthroplasty versus arthrodesis for the treatment of trapeziometacarpal arthritis: a retrospective comparative follow-up study". J Hand Surg Am. 26 (5): 869–76. doi:10.1053/jhsu.2001.26659. PMID 11561240.
- Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L (February 2015). "Surgery for thumb (trapeziometacarpal joint) osteoarthritis". Cochrane Database Syst Rev (2): CD004631. doi:10.1002/14651858.CD004631.pub4. PMC 6464627. PMID 25702783. (Retracted, see doi:10.1002/14651858.cd004631.pub5. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - Atroshi I, Axelsson G, Nilsson EL (June 1998). "Osteotomy versus tendon arthroplasty in trapeziometacarpal arthrosis: 17 patients followed for 1 year". Acta Orthop Scand. 69 (3): 287–90. doi:10.3109/17453679809000932. PMID 9703405.
- Hobby JL, Lyall HA, Meggitt BF (May 1998). "First metacarpal osteotomy for trapeziometacarpal osteoarthritis". J Bone Joint Surg Br. 80 (3): 508–12. doi:10.1302/0301-620x.80b3.8199. PMID 9619947.
- Weilby A, Søndorf J (March 1978). "Results following removal of silicone trapezium metacarpal implants". J Hand Surg Am. 3 (2): 154–6. doi:10.1016/s0363-5023(78)80064-1. PMID 632545.
- Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, Pols HA, Hazes JM, Koes BW (May 2005). "Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study)". Ann. Rheum. Dis. 64 (5): 682–7. doi:10.1136/ard.2004.023564. PMC 1755481. PMID 15374852.
External links
| Wikimedia Commons has media related to Carpometacarpal osteoarthritis. |