Targeted immunization strategies
Targeted immunization strategies are approaches designed to increase the immunization level of populations and decrease the chances of epidemic outbreaks.[1][2] Though often in regards to use in healthcare practices and the administration of vaccines to prevent biological epidemic outbreaks,[3] these strategies refer in general to immunization schemes in complex networks, biological, social or artificial in nature.[1] Identification of at-risk groups and individuals with higher odds of spreading the disease often plays an important role in these strategies.[1][2][4]
| Network science | ||||
|---|---|---|---|---|
| ||||
|
||||
| Network types | ||||
|
||||
| Graphs | ||||
|
||||
| ||||
|
||||
| Models | ||||
|
||||
| ||||
|
||||
Background
The success of vaccines and anti-virus software in preventing major outbreaks relies on the mechanism of herd immunity, also known as community immunity, where the immunization of individuals provides protection for not only the individuals, but also the community at large.[5] In cases of biological contagions such as influenza, measles, and chicken pox, immunizing a critical community size can provide protection against the disease for members who cannot be vaccinated themselves (infants, pregnant women, and immunocompromised individuals). Often however these vaccine programmes require the immunization of a large majority of the population to provide herd immunity.[6] A few successful vaccine programmes have led to the eradication of infectious diseases like small pox[7] and rinderpest, and the near eradication of polio,[8] which plagued the world before the second half of the 20th century.[9][10]
Network-based strategies
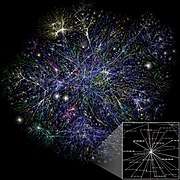
More recently researchers have looked at exploiting network connectivity properties to better understand and design immunization strategies to prevent major epidemic outbreaks.[11][12] Many real networks like the Internet, world wide web, and even sexual contact networks[13] have been shown to be scale-free networks and as such exhibit a power-law distribution for the degree distribution. In large networks this results in the vast majority of nodes (individuals in social networks) having few connections or low degree k, while a few "hubs" have many more connections than the average <k>.[14] This wide variability (heterogeneity) in degree offers immunization strategies based on targeting members of the network according to their connectivity rather than random immunization of the network. In epidemic modeling on scale-free networks, targeted immunization schemes can considerably lower the vulnerability of a network to epidemic outbreaks over random immunization schemes. Typically these strategies result in the need for far fewer nodes to be immunized in order to provide the same level of protection to the entire network as in random immunization.[1][2][15] In circumstances then where vaccines are scarce, efficient immunization strategies become necessary to preventing infectious outbreaks.[16]
Examples
A common approach for targeted immunization studies in scale-free networks focuses on targeting the highest degree nodes for immunization. These nodes are the most highly connected in the network, making them more likely to spread the contagion if infected. Immunizing this segment of the network can drastically reduce the impact of the disease on the network and requires the immunization of far fewer nodes compared to randomly selecting nodes.[1] However, this strategy relies on knowing the global structure of the network, which may not always be practical.[2]
Another strategy, acquaintance immunization,[2][17] tries to target all of the most highly connected nodes for immunization by going through their neighbors without knowing the full network topology. In this approach a random group of nodes are chosen and then a random set of their neighbors are selected for immunization. The most highly connected nodes are far more likely to be in this group of neighbors so immunizing this group results in targeting the most highly connected but requiring far less information about the network.[2][18][19] Another variant of this strategy again calls for the random selection of nodes but instead asks for one of their neighbors with a higher degree, or at least more than a given threshold degree and immunizes them.[12] These degree based strategies consistently require fewer nodes to be immunized and as such improve a network's chances against epidemic attacks.[2][17]
A recent centrality measure, Percolation Centrality, introduced by Piraveenan et al.[20] is particularly useful in identifying nodes for vaccination based on the network topology. Unlike node degree which depends on topology alone, however, percolation centrality takes into account the topological importance of a node as well as its distance from infected nodes in deciding its overall importance. Piraveenan et al.[20] has shown that percolation centrality-based vaccination is particularly effective when the proportion of people already infected is on the same order of magnitude as the number of people who could be vaccinated before the disease spreads much further. If infection spread is at its infancy, then ring-vaccination surrounding the source of infection is most effective, whereas if the proportion of people already infected is much higher than the number of people that could be vaccinated quickly, then vaccination will only help those who are vaccinated and herd immunity cannot be achieved.[6] Percolation centrality-based vaccination is most effective in the critical scenario where the infection has already spread too far to be completely surrounded by ring-vaccination, yet not spread wide enough so that it cannot be contained by strategic vaccination. Nevertheless, Percolation Centrality also needs full network topology to be computed, and thus is more useful in higher levels of abstraction (for example, networks of townships rather than social networks of individuals), where the corresponding network topology can more readily be obtained.
Increasing immunization coverage
Millions of children worldwide do not receive all of the routine vaccinations as per their national schedule. As immunization is a powerful public health strategy for improving child survival, it is important to determine what strategies work best to increase coverage. A Cochrane review assessed the effectiveness of intervention strategies to boost and sustain high childhood immunization coverage in low- and middle income countries.[21] Fourteen trials were included but most of the evidence was of low quality. Providing parents and other community members with information on immunization, health education at facilities in combination with redesigned immunization reminder cards, regular immunization outreach with and without household incentives, home visits, and integration of immunization with other services may improve childhood immunization coverage in low-and middle income countries.
See also
- Influenza vaccine
- Immunization
- Vaccine-preventable diseases
- smallpox eradication
- Poliomyelitis eradication
- Infectious diseases
- ILOVEYOU (computer worm epidemic in 2000)
- Epidemiology
- Epidemic model
- Network Science
- Critical community size
- Scale-free network
- Complex network
References
- Pastor-Satorras R, Vespignani A (March 2002). "Immunization of complex networks". Physical Review E. 65 (3 Pt 2A): 036104. arXiv:cond-mat/0107066. Bibcode:2002PhRvE..65c6104P. doi:10.1103/PhysRevE.65.036104. PMID 11909162.
- Cohen R, Havlin S, Ben-Avraham D (December 2003). "Efficient immunization strategies for computer networks and populations". Physical Review Letters. 91 (24): 247901. arXiv:cond-mat/0207387. Bibcode:2003PhRvL..91x7901C. doi:10.1103/PhysRevLett.91.247901. PMID 14683159.
- "Vaccines and immunization". www.cdc.gov/vaccines/. Center for Disease Control and Prevention. Retrieved 17 November 2014.
- Piddle S (October 14, 2014). "VNA nurses bring shots to school". Clinton Herald. Retrieved 15 November 2014.
- John TJ, Samuel R (2000-07-01). "Herd immunity and herd effect: new insights and definitions". European Journal of Epidemiology. 16 (7): 601–6. doi:10.1023/A:1007626510002. PMID 11078115.
- "Community Immunity ("Herd" Immunity)". National Institute of Allergy and Infectious Diseases. Retrieved 7 April 2014.
- Bazin H (2000). The Eradication of Small Pox. London: Academic Press. ISBN 978-0-12-083475-4.
- "Updates on CDC's Polio Eradication Efforts". www.cdc.gov/polio. Center for Disease Control and Prevention. Retrieved 17 November 2014.
- Lewis T (October 28, 2014). "Polio Vaccine: How the US' Most Feared Disease Was Eradicated". LiveScience. Purch. Retrieved 15 November 2014.
- McNeil Jr DG (May 5, 2014). "Polio's Return After Near Eradication Prompts a Global Health Warning". The New York Times. Retrieved 18 November 2014.
- Campbell E, Salathé M (May 28, 2013). "Complex social contagion makes networks more vulnerable to disease outbreaks". Scientific Reports. 3: 1905. arXiv:1211.0518. Bibcode:2013NatSR...3E1905C. doi:10.1038/srep01905. PMC 3664906. PMID 23712758.
- Gallos LK, Liljeros F, Argyrakis P, Bunde A, Havlin S (April 2007). "Improving immunization strategies". Physical Review E. 75 (4 Pt 2): 045104. arXiv:0704.1589. Bibcode:2007PhRvE..75d5104G. doi:10.1103/PhysRevE.75.045104. PMID 17500948.
- Liljeros F, Edling CR, Amaral LA, Stanley HE, Aberg Y (June 2001). "The web of human sexual contacts". Nature. 411 (6840): 907–8. arXiv:cond-mat/0106507. Bibcode:2001Natur.411..907L. doi:10.1038/35082140. PMID 11418846.
- Barabasi AL, Albert R (October 1999). "Emergence of scaling in random networks". Science. 286 (5439): 509–12. arXiv:cond-mat/9910332. Bibcode:1999Sci...286..509B. doi:10.1126/science.286.5439.509. PMID 10521342.
- Tanaka G, Urabe C, Aihara K (July 2014). "Random and targeted interventions for epidemic control in metapopulation models". Scientific Reports. 4 (5522): 5522. Bibcode:2014NatSR...4E5522T. doi:10.1038/srep05522. PMC 4099978. PMID 25026972.
- Glasser J, Taneri D, Feng Z, Chuang JH, Tüll P, Thompson W, Mason McCauley M, Alexander J (September 2010). "Evaluation of targeted influenza vaccination strategies via population modeling". PLOS ONE. 5 (9): e12777. Bibcode:2010PLoSO...512777G. doi:10.1371/journal.pone.0012777. PMC 2941445. PMID 20862297.
- Madar N, Kalisky T, Cohen R, Ben-avraham D, Havlin S (May 14, 2004). "Immunization and epidemic dynamics in complex networks". The European Physical Journal B. 38 (2): 269–276. Bibcode:2004EPJB...38..269M. CiteSeerX 10.1.1.2.8758. doi:10.1140/epjb/e2004-00119-8.
- Christakis NA, Fowler JH (September 2010). "Social network sensors for early detection of contagious outbreaks". PLOS ONE. 5 (9): e12948. arXiv:1004.4792. Bibcode:2010PLoSO...512948C. doi:10.1371/journal.pone.0012948. PMC 2939797. PMID 20856792.
- Krieger K. "Vaccinate Thy Neighbor" (12). American Physical Society. Physical Review Focus. Retrieved 18 November 2014.
- Piraveenan M, Prokopenko M, Hossain L (2013-01-22). "Percolation centrality: quantifying graph-theoretic impact of nodes during percolation in networks". PLOS ONE. 8 (1): e53095. Bibcode:2013PLoSO...853095P. doi:10.1371/journal.pone.0053095. PMC 3551907. PMID 23349699.
- Oyo-Ita A, Wiysonge CS, Oringanje C, Nwachukwu CE, Oduwole O, Meremikwu MM (July 2016). "Interventions for improving coverage of childhood immunisation in low- and middle-income countries". The Cochrane Database of Systematic Reviews. 7: CD008145. doi:10.1002/14651858.CD008145.pub3. PMC 4981642. PMID 27394698.