Tuberculosis in India
In India, each year, approx. 220,000 deaths are reported due to Tuberculosis. Between 2006 and 2014, the disease cost Indian economy USD 340 billion. This public health problem is the world's largest tuberculosis epidemic.[1] India bears a disproportionately large burden of the world's tuberculosis rates, as it continues to be the biggest health problem in India. It remains one of the largest on India's health and wellness scale. India is the highest TB burden country with World Health Organization (WHO) statistics for 2011 giving an estimated incidence figure of 2.2 million cases of TB for India out of a global incidence of 9.6 million cases.[2] Compare India to Canada, where there are about 1,600 new cases of TB every year.[3] Citing studies of TB-drug sales, the government now suggests the total went from being 2.2 million to 2.6 million people nationwide.[4] On March 24, 2019, TB Day, the Ministry of Health & Family Welfare of India notified that 2.15 million new tuberculosis patients has discovered only in 2018. [5]
Tuberculosis is India's biggest health issue, but what makes this issue worse is the recently discovered phenomenon of TDR-TB - Totally Drug-Resistant Tuberculosis. This issue of drug-resistant TB began with MDR-TB, and moved on to XDR-TB. Gradually, the most dangerous form has situated itself in India as TDR-TB.
"Within India, the Journal—using government data obtained through the Right to Information Act has reported that India's drug-resistance rate is likely much higher than the 2% to 3% of TB cases reported to the WHO"[4]
In India, TB is responsible for the death of every third AIDS patient. moreover, India accounts for about a quarter of the Global TB Burden.[5] The ministry reiterated their commitment to eliminating TB in the country by 2025.[5]
Epidemiology
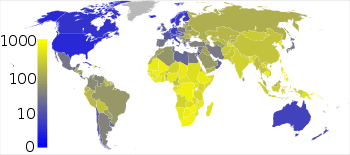
Tuberculosis is one of India's major public health problems. According to WHO estimates, India has the world's largest tuberculosis epidemic.[7] Many research studies have shown the effects and concerns revolving around TDR-TB, especially in India; where social and economic positions are still in progression. In Zarir Udwadia’s report originated from the Hinduja Hospital in Mumbai, India explicitly discusses the drug-resistant effects and results.[8] An experiment was conducted in January, 2012 on four patients to test how accurate the “new category” of TDR-TB is. These patients were given all the first-line drugs and second-line drugs that usually are prescribed to treat TB, and as a result, were resistant to all. As a response, the government of India had stayed in denial, but WHO took it as a more serious matter and decided that although the patterns of drug-resistance were evident, they cannot rely on just that to create a new category of TDR-TB.
"Paul Nunn, coordinator of WHO's STOP TB department in Geneva, described the cases as “a wake up call for countries to accelerate provision of proper care, particularly for multi drug-resistant patients”.[9]
Symptoms
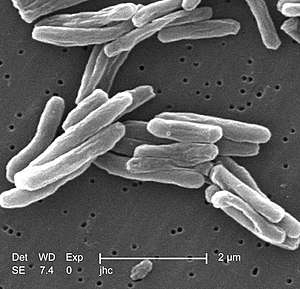
The bacterium that causes TB is called Mycobacterium tuberculosis. Inactive tuberculosis means that one can even unconsciously and unknowingly acquire the bacteria for tuberculosis within them but not even know about it because it is inactive. Whereas, active tuberculosis is the start of the bacteria developing, and the signs and symptoms begin to be visible. This is when tuberculosis is active within you, and is a serious issue leading to even more serious results. Although the TB bacteria can infect any organ (e.g., kidney, lymph nodes, bones, joints) in the body, the disease commonly occurs in the lungs.[3] Around 80% of all TB cases are related to pulmonary or lung.
Common symptoms include: coughing (that lasts longer than 3 weeks with green, yellow, or bloody sputum), weight loss, fatigue, fever, night sweats, chills, chest pain, shortness of breath, and loss of appetite.
Causes
There is a specific bacterium that evolves inside the body to result in tuberculosis, known as mycobacterium tuberculosis. This bacterium is only spread throughout the body when a person has an active TB infection. One of many causes of acquiring TB is living a life with a weak immune system; everything becomes fragile, and an easy target. That is why babies, children, and senior adults have a higher risk of adapting TB.[3] The bacterium spreads in the air sacs, and passes off into the lungs, resulting in an infected immune system.
In addition, coughing, sneezing, and even talking to someone can release the mycobacterium into the air, consequently affecting the people breathing this air. It has been stated that your chances of becoming infected are higher if you come from – or travel to – certain countries where TB is common, and where there is a big proportion of homeless people.[3] India, having the most TB cases of any country[10] falls under this cause because it stands recognized as consuming a higher chance of gaining TB.
Socioeconomic Dimensions of TB
Those listed are all the bodily and personal causes of acquiring TB, but decreases in tuberculosis in India incidence are correlated with improvements in social and economic determinants of health moreso than with access to quality treatment.[11] In India, TB occurs at high rates because of the pollution dispersed throughout the country. Pollution causes many effects in the air the people breathe there, and since TB can be gained through air, the chances of TB remain high and in a consistent movement going uphill for India.
Another major cause for the growth of TB in India has to do with it currently still standing as a developing country. Because its economy is still developing, the citizens are still fighting for their rights, and the structure of the country lies in poor evidence that it is not fit as other countries still. A study of Delhi slums has correlated higher scores on the Human Development Index and high proportions of one-room dwellings tended to incur TB at higher rates.[12] Poor built environments, including hazards in the workplace, poor ventilation, and overcrowded homes have also been found to increase exposure to TB [11]
TB rises high in India because of the majority of patients are not able to afford the treatment drugs prescribed. “At present, only the 1.5 million patients already under the Indian government's care get free treatments for regular TB. That leaves patients who seek treatment in India's growing private sector to buy drugs for themselves, and most struggle to do that, government officials say.”[4] Although the latest phase of state-run tuberculosis eradication program, the Revised National Tuberculosis Control Program, has focused on increasing access to TB care for poor people[10], the majority of poor people still cannot access TB care financially.[13]
Consequently, high priced treatment drugs and the struggles of “poor patients” also brawl through the poor treatment they receive in response to acquiring TB. “It is estimated that just 16% of patients with drug-resistant TB are receiving appropriate treatment”.[14] To combat this huge problem, India has instated a new program to try to provide free drugs to all those infected in the country.[4]
While RNTCP has created schemes to offer free or subsidized, high quality TB care, less than 1% of private practitioners have taken up these practices.[13] Lastly, as high pricing is linked to the economic standings of India, which is linked to poor treatment, it all underlines the lack of education and background information practitioners and professionals hold for prescribing drugs, or those private therapy sessions. A study conducted in Mumbai by Udwadia, Amale, Ajbani, and Rodrigues, showed that only 5 of 106 private practitioners practicing in a crowded area called Dharavi could prescribe a correct prescription for a hypothetical patient with MDR tuberculosis.[15] Because the majority of TB cases are addressed by private providers, and because the majority of poor people access informal (private) providers, the RNTCP's goals for universal access to TB care have not been met.[13]
Poverty and lacking financial resources are also associated with malnutrition, poor housing conditions, substance use, and HIV/AIDS incidence. These factors often cause immunosuppression, and are accordingly correlated with higher susceptibility to TB;[11] they also tend to have greater impacts on people from high incidence countries such as India than lower incidence countries.[16] Indeed, addressing these factors may have a stronger correlation with decreased TB incidence than the decreasing financial burdens associated with care.[11]. Yet, the RNTCP's treatment protocols do not address these social determinants of health.[11]
Disempowerment and stigma are often felt by TB patients as they are disproportionately impoverished or socially marginalized.[17] The DOTS treatment regimen of the RNTCP is thought to deepen this sentiment,[18] as its close monitoring of patients can decrease patient autonomy. To counteract disempowerment, some countries have engaged patients in the process of implementing the DOTS and in creating other treatment regimens that adhere to their nonclinical needs. Their knowledge can inform valuable complements[19] the clinical care provided by the DOTS. Pro-poor strategies, including wage compensation for time lost to treatment, working with civil society organizations to link low income patients to social services, nutritional support, and offering local NGOs and committees a platform for engagement with the work done by private providers may reduce the burden of TB[20] and leads to greater patient autonomy.
Diagnosis
Testing for pulmonary TB
Any person who has signs and symptoms suggestive of TB including a cough for more than 2 weeks, significant weight loss, haemoptysis (coughing blood), etc. and any abnormality in a chest radiograph should be evaluated to find out if they have TB.
Children with a persistent fever and/or cough for more than two weeks, children who have a loss of weight or no weight gain, and/or children who are household contacts of people who have already been diagnosed as having pulmonary TB must be evaluated for TB.
Screening for TB
People living with HIV (PLHIV), people who are malnourished, who have diabetes or cancer, and people on steroid therapy should be regularly screened for signs and symptoms suggestive of TB. Enhanced case finding should be undertaken in certain “high risk” populations such as healthcare workers, prisoners, slum dwellers. There should also be enhanced case finding in certain occupational groups such as mineworkers, as in some countries such as South Africa, there is known to be a high level of TB among miners. Enhanced case finding means having a high level of suspicion for TB in all encounters. Then excluding TB (or indeed identifying TB) using a combination of clinical queries, radiographic and microbiologic testing.
There are a number of diagnostic TB tests currently available.
Microbiological confirmation on sputum
All patients who have presumptive (that is are presumed to have) TB and who are capable of producing sputum, should undergo a sputum test for rapid microbiological diagnosis of TB. These are two type of test 1) by LJ (solid) Method 2) MGIT (liquid) Method
Chest X-ray as a screening tool
Where available chest X-ray should be used as a screening tool.
Cartridge Based Nucleic Acid Amplification Test (CB NAAT)
The CB NAAT is known as the GeneXpert in most countries other than India. This is the preferred first diagnostic test in children and people with TB and HIV co-infection.
Sputum samples
Sputum tests are very important in diagnosing TB, so paying attention to the detail of collecting a good sputum sample is very important. A number of studies have looked at this, and the general view is that two samples are almost as good as three samples.
Binocular microscopes are used for testing TB samples and the diagnosis of TB in India
Methods of testing using sputum samples include sputum smear microscopy (both conventional and fluorescent), culture (on solid or liquid media) commercial line probe assay (LPA) or CB-NAAT. With the advent of CB_NAAT the sensitivity and specificity of rapid diagnosis from sputum, has increased to approximately the levels seen in solid-media sputum culture, but of course the time scales, at just a few hours, are very much shorter with CB-NAAT.
RNTCP Laboratory Network
The Revised National Tuberculosis Control Program (RNTCP) has established a network of laboratories where TB tests can be done to diagnose people who have TB. There are also tests that can be done to determine whether a person has drug-resistant TB.
The laboratory system comprises National Reference Laboratories (NRLs), state level Intermediate Reference Laboratories (IRLs), Culture & Drug Susceptibility Testing (C & DST) laboratories and Designated Microscopy Centres (DMCs). Some of Private lab also Accredited for Culture & Drug Susceptibility Testing for M.tuberculosis (i.e Microcare Laboratory & tuberculosis Research Centre, Surat)
Treatment
India has a large burden of the world's TB, one that this developing country can ill afford, with an estimated economic loss of US $43 billion and 100 million lost annually directly due to this disease.[21] Treatment in India is on the rise just as the disease itself is on the rise. To prevent spreading TB, it's important to get treatment quickly and to follow it through to completion by your doctor. This can stop transmission of the bacteria and the appearance of antibiotic-resistant strains. It is a known fact that bacterial infections require antibiotics for treatment and prevention, thus, commonly you will see that patients diagnosed with tuberculosis have certain pills and antibiotics carried around with them. The antibiotics most commonly used include isoniazid, rifampin, pyrazinamide, and ethambutol. It is crucial to take your medication as instructed by your doctor, and for the full course of the treatment (months or years). This helps to ward off types of TB bacteria that are antibiotic-resistant, which take longer and are more difficult to treat.[3] In India’s case, the particular type of TB infections are majority resistant to regular antibiotic treatment (MDR-TB, XDR-TB, TDR-TB), therefore, not one or two medications will help, rather a combination of different medications must be taken for over a course of 18–24 months, depending on how deep the infection is. Since the 1960s, two drugs — isoniazid and rifampicin — have been the standard TB treatment.[14] In addition to antibiotics, a vaccine is available to limit the spread of bacteria after TB infection. The vaccine is generally used in countries or communities where the risk of TB infection is greater than 1% each year,[3] thus, the country of India; whose TB infection rate is at a peak (world’s third highest TB infected country), and is consistently growing, and giving 20% of the world’s diagnosed patients a home.[14] At present the anti TB treatment offered in public and private sector in India is not satisfactory and needs to be improved.[22] Today India's TB control program needs to update itself with the international TB guidelines as well as provide an optimal anti TB treatment to the patients enrolled under it or it will land up being another factor in the genesis of drug-resistant tuberculosis.[23]
The Indian government’s Revised National TB Control Programme (RNTCP) started in India during 1997. The program uses the WHO-recommended Directly Observed Treatment Short Course (DOTS) strategy to develop ideas and data on TB treatment. This group’s initial objective is to achieve and maintain a TB treatment success rate of at least 85% in India among new patients.[24] “In 2010 the RNTCP made a major policy decision that it would change focus and adopt the concept of Universal Access to quality diagnosis and TB treatment for all TB patients”.[9] By doing so, they extend out a helping hand to all people diagnosed with TB, and in addition, provide better quality services and improve on therapy for these patients.
Treatment recommendations from Udwadia, et al. suggest that patients with TDR-TB only be treated “within the confines of government-sanctioned DOTS-Plus Programs to prevent the emergence of this untreatable form of tuberculosis”.[14] As this confirming result of hypothesis is at a conclusion by Udawadai, et al., it is given that the new Indian government program will insist on providing drugs free of charge to TB patients of India, for the first time ever.[4]
Tuberculosis Association of India
The Tuberculosis Association of India is a voluntary organization. It was set up in February 1939. It is also affiliated to the Govt. of India & is working with TB Delhi center.[25]
See also
India-related
- Public health system in India
- Pharmaceutical industry in India
Tuberculosis-related
- 2007 tuberculosis scare
- Abreugraphy
- ATC code J04 Drugs for treatment of TB
- Buruli ulcer and leprosy: other diseases caused by mycobacteria
- Latent tuberculosis
- List of tuberculosis victims
- Mycobacterium Tuberculosis Structural Genomics Consortium
- National Center for HIV, STD, and TB Prevention
- Nontuberculous mycobacteria
- Overcrowding
- Philip D'Arcy Hart
- Tuberculosis in history and art
- UNITAID
- Nosocomial infection
- Isaac Santra
References
- World Health Organization (2009). "Epidemiology" (PDF). Global tuberculosis control: epidemiology, strategy, financing. pp. 6–33. ISBN 978-92-4-156380-2. Retrieved 12 November 2009.
- TB Statistics for India. (2012). TB Facts. Retrieved April 3, 2013, from http://www.tbfacts.org/tb-statistics-india.html
- Tuberculosis - Causes, Symptoms, Treatment, Diagnosis. (2013). C-Health. Retrieved April 3, 2103, from http://chealth.canoe.ca/channel_condition_info_details.asp?disease_id=231&channel_id=1020&relation_id=71085
- Anand, G., & McKay, B. (2012). Awakening to Crisis, India Plans New Push Against TB. The Wall Street Journal. Retrieved April 3, 2013, from http://online.wsj.com/article/SB10001424127887324461604578193611711666432.html
- "India records 2.15m new TB patients in 2018". The Nation. 2019-03-26. Retrieved 2019-03-27.
- "The Stop TB Strategy, case reports, treatment outcomes and estimates of TB burden". Global tuberculosis control: epidemiology, strategy, financing. World Health Organization. 2009. pp. 187–300. ISBN 978-92-4-156380-2. Archived from the original on 2009-11-19. Retrieved 2009-11-14.
- WHO. Global tuberculosis control. WHO report. WHO/HTM/TB/2006.362. Geneva: World Health Organization, 2006.
- Udwadia, Zarir; Vendoti, Deepesh (2013). "Totally drug-resistant tuberculosis (TDR-TB) in India: Every dark cloud has a silver lining". Journal of Epidemiology and Community Health. 67 (6): 471–472. doi:10.1136/jech-2012-201640. PMID 23155059.
- https://m.facebook.com/story.php?story_fbid=1680306518662783&id=100000503523412%5B%5D%5B%5D%5B%5D
- Sachdeva, Kuldeep Singh et al. “New vision for Revised National Tuberculosis Control Programme (RNTCP): Universal access - "reaching the un-reached".” The Indian journal of medical research vol. 135,5 (2012): 690-4.
- Hargreaves, James R et al. “The social determinants of tuberculosis: from evidence to action.” American journal of public health vol. 101,4 (2011): 654-62. doi:10.2105/AJPH.2010.199505
- Chandra, Shivani. “Resurrecting Social Infrastructure as a Determinant of Urban Tuberculosis Control in Delhi, India.” Health Research Policy and Systems, vol. 12, no. 3, 2014, health-policy-systems.biomedcentral.com/track/pdf/10.1186/1478-4505-12-3.
- Verma, Ramesh (2013). [www.ncbi.nlm.nih.gov/pmc/articles/PMC3570899/ "Revised National Tuberculosis Control Program in India: The Need to Strengthen"] Check
|url=value (help). International Journal of Preventive Medicine. 4: 1–5 – via NCBI. - Rowland, Katherine (2012). "Totally drug-resistant TB emerges in India". Nature. doi:10.1038/nature.2012.9797.
- Udwadia, Z. F; Amale, R. A; Ajbani, K. K; Rodrigues, C (2011). "Totally Drug-Resistant Tuberculosis in India". Clinical Infectious Diseases. 54 (4): 579–581. doi:10.1093/cid/cir889. PMID 22190562.
- Dye, Christopher, et al. “Nutrition, Diabetes and Tuberculosis in the Epidemiological Transition.” PLoS ONE, vol. 6, no. 6, June 2011, pp. 1–7., journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0021161&type=printable.
- Daftary A, Frick M, Venkatesan N, et al. Fighting TB stigma: we need to apply lessons learnt from HIV activism. BMJ Glob Health 2017;2:e000515.doi:10.1136/ bmjgh-2017-000515
- Achmat, Z. “Science and Social Justice: the Lessons of HIV/AIDS Activism in the Struggle to Eradicate Tuberculosis.” Int J Tuberc Lung Dis, vol. 10, no. 12, 2006, pp. 1312–1317.
- Corburn, J. “Street Science: Characterizing Local Knowledge.” Street Science: Community Knowledge and Environmental Health Justice, MIT Press, 2005, pp. 47–77.
- Kamineni, Vishnu Vardhan et al. “Addressing poverty through disease control programmes: examples from Tuberculosis control in India.” International journal for equity in health vol. 11 17. 26 Mar. 2012, doi:10.1186/1475-9276-11-17
- Udwadia, Zarir F (2012). "MDR, XDR, TDR tuberculosis: Ominous progression". Thorax. 67 (4): 286–288. doi:10.1136/thoraxjnl-2012-201663. PMID 22427352.
- Mishra G, Mulani J. Tuberculosis Prescription Practices In Private And Public Sector In India. NJIRM. 2013; 4(2): 71-78.Available online at http://www.scopemed.org/?mno=36915. Accessed on 6/5/2013.
- Mishra, Gyanshankar; Ghorpade, S. V; Mulani, J (2014). "XDR-TB: An outcome of programmatic management of TB in India". Indian Journal of Medical Ethics. 11 (1): 47–52. doi:10.20529/IJME.2014.013. PMID 24509111.
- http://www.scidev.net/tb/facts%5B%5D%5B%5D%5B%5D
- http://tbassnindia.org/home.html
Further reading
General and applied
- Sharma SK, Liu JJ (2006). "Progress of DOTS in global tuberculosis control". Lancet. 367 (9514): 951–2. doi:10.1016/S0140-6736(06)68391-8. PMID 16546549.
- China Tuberculosis Control Collaboration (2004). "The effect of tuberculosis control in China". Lancet. 364 (9432): 417–22. doi:10.1016/S0140-6736(04)16764-0. PMID 15288739..
- Dye C, Fengzeng Z, Scheele S, Williams B (2000). "Evaluating the impact of tuberculosis control: number of deaths prevented by short-course chemotherapy in China". International Journal of Epidemiology. 29 (3): 558–64. doi:10.1093/ije/29.3.558. PMID 10869331.
- Squire SB, Tang S (2004). "How much of China's success in tuberculosis control is really due to DOTS?". Lancet. 364 (9432): 391–2. doi:10.1016/S0140-6736(04)16777-9. PMID 15288717.
- Xianyi C, Fengzeng Z, Hongjin D, et al. (2002). "The DOTS strategy in China: results and lessons after 10 years". Bull. World Health Organ. 80 (6): 430–6. PMC 2567538. PMID 12131998.
- World Health Organization. In: An expanded DOTS framework for effective tuberculosis control: stop TB communicable diseases. Geneva: WHO, 2002: 1-20WHO Document WHO/CDS/TB/2002·297.
- China Tuberculosis Control Collaboration (1996). "Results of directly observed short-course chemotherapy in 112,842 Chinese patients with smear-positive tuberculosis. China Tuberculosis Control Collaboration". Lancet. 347 (8998): 358–62. doi:10.1016/S0140-6736(96)90537-1. PMID 8598701.
- Tang S, Wang L, Wang X, Squire SB (2002). "Does rapid economic growth reduce TB prevalence in the absence of effective TB control". Int J TB Lung Dis. 6. (suppl 1): S149.
- Zignol M, Hosseini MS, Wright A, et al. (2006). "Global incidence of multidrug-resistant tuberculosis". J. Infect. Dis. 194 (4): 479–85. doi:10.1086/505877. PMID 16845631.
- Blumberg HM, Leonard MK, Jasmer RM (2005). "Update on the treatment of tuberculosis and latent tuberculosis infection". JAMA. 293 (22): 2776–84. doi:10.1001/jama.293.22.2776. PMID 15941808.
- Dormandy, Thomas (2000). The White Death. New York: New York University Press. ISBN 978-0-8147-1927-5.
- Joint Tuberculosis Committee of the British Thoracic Society (2000). "Control and prevention of tuberculosis in the United Kingdom: code of practice 2000". Thorax. 55 (11): 887–901. doi:10.1136/thorax.55.11.887. PMC 1745632. PMID 11050256.
- Kidder, Tracy (2004). Mountains beyond Mountains. New York: Random House Trade Paperbacks. ISBN 978-0-8129-7301-3. A nonfiction account of treating TB in Haiti, Peru, and elsewhere.
- Lawlor, Clark (2007). Consumption and Literature. Basingstoke: Palgrave Macmillan. ISBN 978-0-230-02003-0.
- Nemery B, Yew WW, Albert R, et al. (2005). "Tuberculosis, nontuberculous lung infection, pleural disorders, pulmonary function, respiratory muscles, occupational lung disease, pulmonary infections, and social issues in AJRCCM in 2004". Am. J. Respir. Crit. Care Med. 171 (6): 554–62. doi:10.1164/rccm.2412009. PMID 15753485.
- Walton D, Farmer P (2000). "MSJAMA: the new white plague". JAMA. 284 (21): 2789. doi:10.1001/jama.284.21.2789. PMID 11105192.
External links
| Wikimedia Commons has media related to Tuberculosis. |
- Tuberculosis in India at Curlie
- Centers for Disease Control and Prevention (CDC), Division of Tuberculosis Elimination. Core Curriculum on Tuberculosis: What the Clinician Should Know. 4th edition (2000). Updated Aug 2003.
- (CDC) - Division of Tuberculosis Elimination News and updates.
- (CDC) - Questions and Answers About TB, 2005.
- BioHealthBase Bioinformatics Resource Center. Database of Mycobacterium tuberculosis genome sequences and related information.
- Kaiser Family Foundation. Tuberculosis. Globalhealthfacts.org.
- The Nobel Prize Website. Tuberculosis Educational Game
- United States Agency for International Development (USAID). The Tuberculosis Coalition for Technical Assistance (TBCTA).
- World Health Organization (WHO). Tuberculosis.
- Medical Research Council (MRC) Tuberculosis
- "Hindustan Times". Hindustan Times. 24 January 2015. Retrieved April 1, 2015.
- (SciDev.Net) Tuberculosis:
- An introduction to TB and our online resource:
- Facts & figures on the prevalence of TB in the developing world:
- Opinions – key stakeholder views on collaboration, treatment and diagnostics:
- A feature examining the threat of bovine TB to human health:
- Articles – all SciDev.Net's latest TB coverage:
- Policy – summaries of relevant policy briefs:
- Key documents – short summaries of significant publications:
- Links to key organisations relevant to TB treatment and control:
- Definitions – a directory of terms used in TB research, treatment and control: