Suicide in the United States
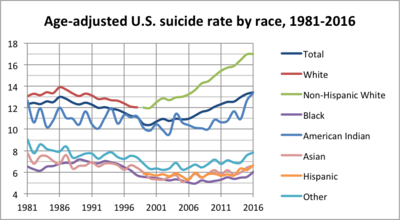
Suicide is a major national public health issue in the United States. In 2017, there were 47,173 recorded suicides,[2] up from 42,773 in 2014, according to the CDC's National Center for Health Statistics (NCHS).[3][4][5] On average, adjusted for age, the annual U.S. suicide rate increased 24% between 1999 and 2014, from 10.5 to 13.0 suicides per 100,000 people, the highest rate recorded in 28 years.[6][7] Due to the stigma surrounding suicide, it is suspected that suicide generally is underreported.[8] In April 2016, the CDC released data showing that the suicide rate in the United States had hit a 30-year high,[9][10] and later in June 2018, released further data showing that the rate has continued to increase and has increased in every U.S. state except Nevada since 1999.[11][12] Surging death rates from suicide, drug overdoses and alcoholism, what researchers refer to as "deaths of despair", are largely responsible for a consecutive three year decline of life expectancy in the U.S.[13][14][15][16] This constitutes the first three-year drop in life expectancy in the U.S. since the years 1915-1918.[15]
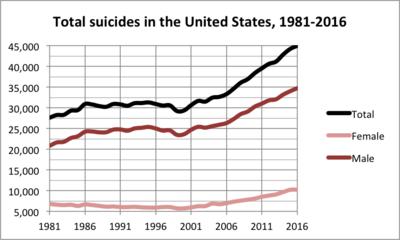
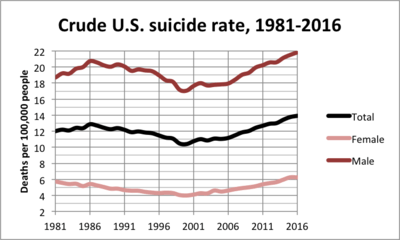
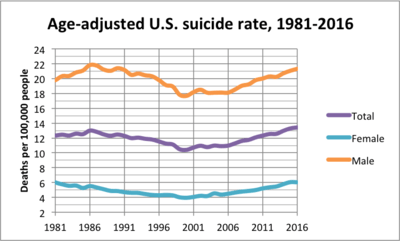
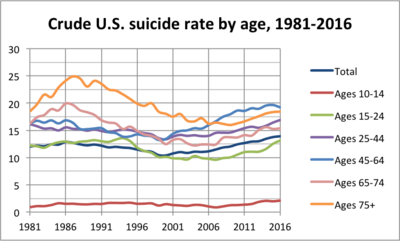
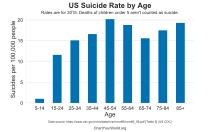
In 2015, suicide was the seventh leading cause of death for males and the 14th leading cause of death for females.[17] Additionally, it was the second leading cause of death for young people aged 15 to 34 and the third leading cause of death for those between the ages of 10 and 14.[18] From 1999 to 2010, the suicide rate among Americans aged 35 to 64 increased nearly 30 percent. The largest increases were among women aged 60 to 64, with rates rising 60 percent, then men in their fifties, with rates rising nearly 50 percent.[7] In 2008, it was observed that U.S. suicide rates, particularly among middle-aged white women, had increased, although the causes were unclear.[19]
The American Foundation for Suicide Prevention reported that in 2016 suicide was the 10th leading cause of death in the U.S., imposing a cost of $69 billion to the US annually.[8][17] Other statistics reported are:[8]
- The annual age-adjusted suicide rate is 13.42 per 100,000 individuals.
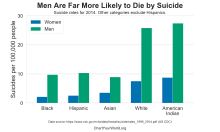
- Men die by suicide 3.53x more often than women.
- On average, there are 123 suicides per day.
- White males accounted for 7 of 10 suicides in 2016.
- A firearm is used in almost 50% of all suicides.
- The rate of suicide is highest in middle age—white men in particular.
The U.S. government seeks to prevent suicides through its National Strategy for Suicide Prevention, a collaborative effort of Substance Abuse and Mental Health Services Administration, Centers for Disease Control and Prevention, National Institutes of Health, Health Resources and Services Administration, and Indian Health Service.[20] Their plan consists of eleven goals aimed at preventing suicides.[21] Older adults are disproportionately likely to commit suicide.[22] Some U.S. jurisdictions have laws against suicide or against assisting suicide. In recent years, there has been increased interest in rethinking these laws.[23] These policies focus on the recovery of the individual through the treatment of the mental disease. The aim is to assure the wellness and the health of the person affected as well as make sure that they recover and take advantage of their all potential.[24]
Suicide has been associated with tough economic conditions, including unemployment rate.[25]
There are significant variations in the suicide rates of the different states,[26] ranging from 28.89 per 100,000 people in Montana to 8.11 per 100,000 people in New York.[8]
Approximately half of suicides are committed using a firearm, accounting for two-thirds of all firearm deaths.[27] Firearms were used in 56.9% of suicides among males in 2016, making it the most commonly used method by them.[17]
Trends in suicide attempts
The spike in suicide rates in the United States during the 21st century has gained public and clinical attention. Studies have found that despite all efforts to minimize suicide rates, rates have steadily increased by approximately 2% per year from 2006 to 2014.[28] A national epidemiologic survey of 69 341 US adults found the percentage of adults attempting suicide increased from 0.62% in 2004 through 2005 to 0.79% in 2012 through 2013.[29] Because of this, clinicians aim to determine whether this is a coincident national increase in suicide attempts. In order to achieve this, trends in suicide attempts are characterized among sociodemographic and clinical groups. It was found that suicide attempts impact "younger adults with less formal education and those with antisocial personality disorder, anxiety disorders, depressive disorders, and a history of violence” at disproportional rates.[29] It is important for trends in suicide attempts to be investigated and researched for they help to determine the cause of the increase in suicide rates. Knowing the trends in suicide also allow preventative measures to be taken. Suicide prevention is possible through early identification and treatment of individuals deemed high risk.[30]
Suicide as a public health crisis
Suicide prevention has been thought of as the responsibility of mental health professionals within clinical settings between 2000-2010.[31] As of 2019, suicide prevention is being recognized as a public health responsibility rather than within clinical settings due to the trend in increasing suicide rates.[32] In 1960-2010, population-based risk reduction approaches have been used for other diseases such as myocardial infarction. However, as of 2019, the urgency of development of effective suicide prevention has been recognized by the CDC. While suicide is often thought of as an individual problem, suicides may impact families, communities, and society in general. The responsibility of public health would be to develop policies to reduce people's risk of suicidal behavior through addressing factors at the individual to societal levels.[32]"Public health emphasizes efforts to prevent violence (in this case, toward oneself) before it happens. This approach requires addressing factors that put people at risk for, or protect them from, engaging in suicidal behavior."[32] The CDC has created a National Suicide Prevention Lifeline where they provide free and confidential support for people in distress, prevention and crisis resources for people who are in need of such help, and best practices for professionals.[33] In May 2019, Bloomberg reported that in spite of the recent mental health crisis, insurance companies, including UnitedHealth Group, are doing what they can to limit coverage and deny claims for mental health related issues.[34]
A 2019 study by a private non-profit called National Bureau of Economic Research says there is a direct causal link between worker's wages and suicide rates, and that raising the minimum wage would result in a quick drop in the suicide rate.[14]
Subgroups
Age and sex
The National Violent Death Reporting System (NVDRS) keeps data on U.S. suicides.
| Age (years) | 10 – 14 | 15 – 24 | 25 – 34 | 35 – 44 | 45 – 54 | 55 – 64 | 65 – 74 | 75+ | Unknown | All |
|---|---|---|---|---|---|---|---|---|---|---|
| Males | 265 | 4575 | 5887 | 5294 | 6198 | 5745 | 3463 | 3291 | 2 | 34727 |
| Females | 171 | 1148 | 1479 | 1736 | 2239 | 2014 | 940 | 510 | 1 | 10238 |
| Male/Female Ratio | 1.5 | 4.0 | 4.0 | 3.0 | 2.8 | 2.9 | 3.7 | 6.5 | 1.0 | 3.4 |
| Total | 436 | 5723 | 7366 | 7030 | 8437 | 7759 | 4403 | 3801 | 3 | 44965 |
Based on the NVDRS 2016 data, the New York Times acknowledged that, among men, those over 65—who make up a smaller proportion of the population—are at greatest risk of death by suicide.[36] The NVDRS 2015 data showed that, among men of all races, men over 65 were the most likely to die of suicides (27.67 suicides per 100,000), closely followed by men 40–64 (27.10 suicides per 100,000). Men 20–39 (23.41 per 100,000) and 15–19 (13.81 per 100,000) were less likely to die of suicides.[37]
By state
There are significant variations in the suicide rates of the different states.[26] A number of theories for these differences have been suggested, ranging from socioeconomics to access to firearms and isolation (low population densities),[38] and a study in 2011 found a correlation between altitude above sea level and suicide.[39]
| Suicide rate by state (2017)[40] | ||
|---|---|---|
| Rank | State | Suicide rate per 100,000 people |
| 1 | Montana | 28.9 |
| 2 | Alaska | 27.0 |
| 3 | Wyoming | 26.9 |
| 4 | New Mexico | 23.3 |
| 5 | Idaho | 23.2 |
| 6 | Utah | 22.7 |
| 7 | South Dakota | 22.5 |
| 8 | West Virginia | 21.1 |
| 9 | Arkansas | 20.8 |
| 10 | Nevada | 20.3 |
| 11 | Colorado | 20.3 |
| 12 | North Dakota | 20.1 |
| 13 | Oklahoma | 19.1 |
| 14 | Kansas | 19.1 |
| 15 | Oregon | 19.0 |
| 16 | New Hampshire | 18.9 |
| 17 | Maine | 18.9 |
| 18 | Missouri | 18.5 |
| 19 | Vermont | 18.3 |
| 20 | Arizona | 18.2 |
| 21 | Washington | 16.9 |
| 22 | Kentucky | 16.9 |
| 23 | Tennessee | 16.8 |
| 24 | Alabama | 16.6 |
| 25 | South Carolina | 16.3 |
| 26 | Indiana | 16.3 |
| 27 | Wisconsin | 15.4 |
| 28 | Louisiana | 15.2 |
| 29 | Hawaii | 15.2 |
| 30 | Pennsylvania | 15.0 |
| 31 | Mississippi | 15.0 |
| 32 | Iowa | 15.0 |
| 33 | Ohio | 14.8 |
| 34 | Nebraska | 14.7 |
| 35 | North Carolina | 14.3 |
| 36 | Michigan | 14.1 |
| 37 | Florida | 14.0 |
| 38 | Minnesota | 13.8 |
| 39 | Georgia | 13.6 |
| 40 | Virginia | 13.4 |
| 41 | Texas | 13.4 |
| 42 | Rhode Island | 11.8 |
| 43 | Delaware | 11.6 |
| 44 | Illinois | 11.2 |
| 45 | Connecticut | 10.5 |
| 46 | California | 10.5 |
| 47 | Maryland | 9.8 |
| 48 | Massachusetts | 9.5 |
| 49 | New Jersey | 8.3 |
| 50 | New York | 8.1 |
College students
Suicide in the subgroup of college students is very prevalent. In the college population, suicide is the second highest cause of death.[41] Yet, the severity of this issue among the youth in college is underestimated. Many falsely believe that young people do not have thoughts about suicide.[42] The suicide rate for male students is about three times higher than for women.[43] The study of suicide rates and trends were not something very common in the past but is gaining more attention in 2019. Allan Schwartz, an associate professor in psychology at the University of Rochester and senior staff at the University Counseling Center, stated that the reported rates of suicide are not reflected in society.[42] In the fourteen years, from 1990 to 2004, about 1,404 college students committed suicide. This is about 6.5 percent of those who committed suicide nationwide. This accounts for half of the suicide rates across the entire U.S. population, at 12.6 percent. In 2014, the adjusted age rate was higher for male than female; the suicide rate for males was 20.7 per 100,000 and 5.8 per 100,100 for females.[43] Counseling services are critical and helpful in preventing people from committing suicide. However, currently, there is a deficit between the available resources and the number of students who need such counseling searches.[41] Students who do not go to counseling services are at 18 times more at risk of suicide compared to other students. If a college student has any suicidal thoughts, it is always critical to let others, such as members of the school, family, or friends know.[43]
Military
A 2009 U.S. Army report indicates military veterans have double the suicide rate of non-veterans, and more active-duty soldiers have died from suicide than in combat in the Iraq War (2003–2011) and War in Afghanistan (2001–present).[44] Colonel Carl Castro, director of military operational medical research for the Army noted "there needs to be a cultural shift in the military to get people to focus more on mental health and fitness."[45] In 2012, the US Army reported 185 suicides among active-duty troops, exceeding the number of combat deaths in that year (176). This figure has significantly increased since 2001, when the number of suicides was 52.[46]
LGBTQ
Attempted suicide rates for lesbian, gay, bisexual, transgender and questioning (LGBTQ) youth and adults in the U.S. are three times higher than national averages.[47]
Chronic pain
Patients with chronic pain are twice as likely to attempt suicide compared with those without chronic pain.[48]
Autism
Studies have found very high rates of suicide in people with autism spectrum disorders, including high functioning autism and what was formerly known as Asperger syndrome. Autism and particularly Asperger syndrome are highly associated with clinical depression and as many as 30 percent or more of people with Asperger syndrome also suffer from depression.[49]
Murder–suicide
There have been many high-profile incidents in the United States in the 1990s, 2000s and 2010s of individuals thought to be attempting "suicide by cop" or killing others before killing themselves. Examples include the 1999 Columbine High School massacre, the 2007 Virginia Tech massacre, the 2010 Austin plane crash, the 2012 Sandy Hook Elementary School shooting and the 2014 Isla Vista killings.
Comparison between countries
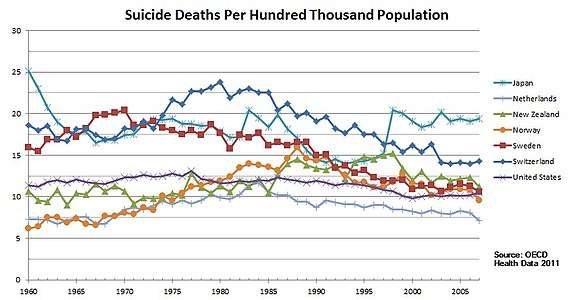 Trend of suicide deaths from 1960 to 2007 for Japan, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United States
Trend of suicide deaths from 1960 to 2007 for Japan, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United States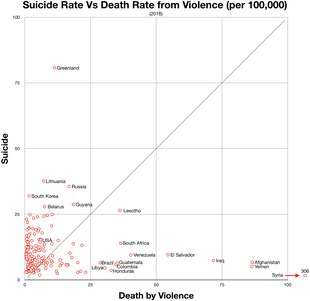 Suicide vs violent deaths 2016
Suicide vs violent deaths 2016
See also
- Assisted suicide in the United States
- Euthanasia in the United States
- National Suicide Prevention Week
- Suicide among LGBT youth
- Suicide among Native Americans in the United States
- Suicide in colleges in the United States
- Teenage suicide in the United States
References
- "WISQARS Fatal Injury Reports". Webappa.cdc.gov. Retrieved 1 June 2019.
- "Deaths From Drugs and Suicide Reach a Record in the U.S." The New York Times. March 7, 2019.
- "Products – Data Briefs – Number 241 – April 2016". Cdc.gov. Retrieved 9 November 2017.
- "Data Brief 241: Increase in Suicide in the United States, 1999–2014 : Data table for Figure 1. Age-adjusted suicide rates, by sex: United States, 1999–2014" (PDF). Cdc.gov. Retrieved 9 November 2017.
- "Deaths: Final Data for 2014" (PDF). Cdc.gov. Retrieved 9 November 2017.
- Tavernise, Sabrina (22 April 2016). "U.S. Suicide Rate Surges to a 30-Year High". NYTimes.com.
- TARA PARKER-POPE (May 2013). "Suicide Rates Rise Sharply in U.S."
- "Suicide Statistics — AFSP". AFSP. Retrieved 2017-05-16.
- "U.S. suicide rate surges to three decade high". Chicago Tribune. Tronc. April 22, 2016. Retrieved September 14, 2018.
- Tavernise, Sabrina (April 22, 2016). "U.S. Suicide Rate Surges to a 30-Year High". The New York Times. The New York Times Company. Retrieved September 14, 2018.
- Maggie, Fox (June 7, 2018). "Suicide rates are up 30 percent since 1999, CDC says". NBC News. Retrieved September 14, 2018.
- Hedegaard, Holly; Curtin, Sally C.; Warner, Margaret (June 2018). Suicide Rates in the United States Continue to Increase (PDF). NCHS Data Brief No. 309 (Report). Centers for Disease Control and Prevention.
- Kight, Stef W. (March 6, 2019). "Deaths by suicide, drugs and alcohol reached an all-time high last year". Axios. Retrieved May 21, 2019.
- Cerullo, Megan (April 30, 2019). "Want to decrease suicide? Raise the minimum wage, researchers suggest". CBS News. Retrieved June 24, 2019.
- Koons, Cynthia (June 20, 2019). "Latest Suicide Data Show the Depth of U.S. Mental Health Crisis". Bloomberg. Retrieved July 5, 2019.
- Ducharme, Jamie (June 13, 2019). "More Millennials Are Dying 'Deaths of Despair,' as Overdose and Suicide Rates Climb". TIME. Retrieved July 10, 2019.
- "Facts at a Glance 2015" (PDF). Cdc.gov. Retrieved 1 June 2019.
- "Suicide". National Institute of Mental Health. Retrieved 8 September 2017.
- "U.S. Suicide Rate Increases". Jhsph.edu. 2009-09-03. Retrieved 2011-08-06.
- "Suicide Prevention, Substance Abuse and Mental Health Services Administration". Mentalhealth.samhsa.gov. Archived from the original on 2010-05-28. Retrieved 2011-08-06.
- "Substance Abuse and Mental Health Publications| SAMHSA Store". Mentalhealth.samhsa.gov. Archived from the original on 2010-05-28. Retrieved 2011-08-06.
- "In Harm's Way: Suicide in America – MHM: Suicide". Mental-health-matters.com. 2009-02-17. Retrieved 2011-08-06.
- Engelhardt, H. Tristram Jr.; Malloy, Michele (1982–1983), Suicide and Assisting Suicide: A Critique of Legal Sanctions, 36, Sw. L.J., p. 1003
- ASPA (2013-03-12). "Recovery is Possible". Mentalhealth.gov. Retrieved 2017-05-16.
- DS Hamermesh; NM Soss (1974), An economic theory of suicide, The journal of political economy, JSTOR 1830901
- "2015 Annual Report". America's Health Rankings. Retrieved 3 November 2017.
- "FastStats". Cdc.gov. Retrieved 9 November 2017.
- Curtin, Sally C.; Warner, Margaret; Hedegaard, Holly (April 2016). "Increase in suicide in the United States, 1999-2014. NCHS Data Brief No. 214" (PDF). NCHS Data Brief. 241 – via CDC.
- Olfson, Blanco, Wall,, Mark, Carlos, Melanie (2017-11-01). "National Trends in Suicide Attempts Among Adults in the United States". JAMA Psychiatry. 74 (11): 1095–1103. doi:10.1001/jamapsychiatry.2017.2582. PMC 5710225.CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)
- US Department of Health and Human Services Office of the Surgeon General; National Action Alliance for Suicide Prevention (September 2012). "2012 National Strategy for Suicide Prevention: Goals and Objectives for Action". US Department of Health and Human Services.
- Knox, Kelly (2015). ""If Suicide Is a Public Health Problem, What Are We Doing to Prevent It?"". American Journal of Public Health.
- "Applying Science. Advancing Practice" (PDF).
- "Home". suicidepreventionlifeline.org. Retrieved 2019-04-17.
- Koons, Cynthia; Tozzi, John (May 16, 2019). "As Suicides Rise, Insurers Find Ways to Deny Mental Health Coverage". Bloomberg. Retrieved May 21, 2019.
- 2016, United States: Suicide Injury Deaths and Rates per 100,000. (All Races, Both Sexes, All Ages)". Retrieved 3 March 2018 – via WISQARS Fatal Injury Reports – CDC.
- Span, Paula (25 May 2018). "In Elderly Hands, Firearms Can Be Even Deadlier Image". New York Times. Retrieved 27 May 2018.
- "National Violent Death Reporting System". Centers for Disease Control and Prevention. Retrieved 27 May 2018.
- Thompson, J. (14 January 2015). "Is altitude causing suicide in the West?". High Country News. Retrieved 3 November 2017.
- Barry Brenner; David Cheng; Sunday Clark (2011), "Positive Association between Altitude and Suicide in 2584 U.S. Counties", High Alt. Med. Biol., High Altitude Medicine and Biology, 12: 31–5, doi:10.1089/ham.2010.1058, PMC 3114154, PMID 21214344
- "Stats of the State - Suicide Mortality". CDC National Center for Health Statistics. 10 January 2019. Retrieved 24 October 2019.
- Schwartz, Allan (2006). "College Students Suicide in the United States: 1990-1991 Through 2003-2004". Journal of Journal American Health. 54: 341. doi:10.3200/jach.54.6.341-352.
- "Youth". suicidepreventionlifeline.org. Retrieved 2019-04-17.
- "Welcome to CDC stacks | Increase in suicide in the United States, 1999–2014 - 39008 | Stephen B. Thacker CDC Library collection". stacks.cdc.gov. Retrieved 2019-03-29.
- Woods, Tyler (September 7, 2009). "This Week Is National Suicide Prevention Week". Emax Health. Retrieved 14 June 2012.
- Jelinek, Pauline (September 5, 2008). "Army: soldier suicide rate may set record again". USA Today/Associated Press. Retrieved 14 June 2012.
- Wood, David (September 25, 2013). "Army Chief Ray Odierno Warns Military Suicides 'Not Going To End' After War Is Over". Huffington Post. Retrieved 11 July 2014.
- Melin, Amy (September 11, 2008). "AFSP walkathon raises suicide awareness". Western Herald. Retrieved 14 June 2012.
- "Patients With Chronic Pain Are Twice as Likely to Attempt Suicide". Clinical Pain Advisor. 4 October 2017.
- Johnny L. Matson; Marie S. Nebel-Schwalm. "Comorbid psychopathology with autism spectrum disorder in children: An overview" (PDF). Vcuautismcenter.org. Retrieved 9 November 2017.