Herpes zoster ophthalmicus
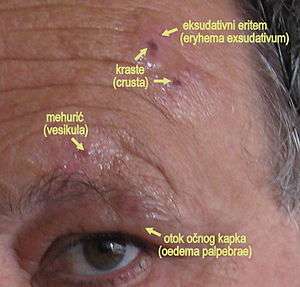
Herpes zoster ophthalmicus (HZO) and also known as ophthalmic zoster is a disease characterised by reactivation of dormant varicella zoster virus residing within the ophthalmic nerve (the first division of the trigeminal nerve).[1]:380[2] This condition is an important subtype of shingles, representing 15% of all cases.[3] Herpes zoster ophthalmicus is transmitted via direct contact or droplets. Varicella zoster virus is a DNA virus which produces acidophilic intranuclear inclusion bodies. The virus is neurotropic in nature.
| Ophthalmic zoster | |
|---|---|
 | |
| Herpes zoster ophthalmicus | |
| Specialty | Infectious disease |
The frontal nerve is more commonly affected than the nasociliary nerve or lacrimal nerve.[4]
Signs and symptoms

Skin
- Viral prodrome
- Preherpetic neuralgia
- Rash, transitioning from papules to vesicles to pustules to scabs.
- Hutchinson's sign: cutaneous involvement of the tip of the nose, indicating nasociliary nerve involvement. A positive Hutchinson's sign increases the likelihood of ocular complications associated with HZO.
- Disseminated distribution in individuals with immunodeficiency.[3]
Cornea
- Epithelial: punctate epithelial erosions and pseudodendrites: often have anterior stromal infiltrates. Onset 2 to 3 days after the onset of the rash, resolving within 2–3 weeks. Common.
- Stromal:
- Nummular keratitis: have anterior stromal granular deposits. Occurs within 10 days of onset of rash. Uncommon
- Necrotising interstitial keratitis: Characterised by stromal infiltrates, corneal thinning and possibly perforation. Occurs between 3 months and several years after onset of rash. Rare.
- Disciform Keratitis (Disciform Endotheliitis): a disc of corneal oedema, folds in Descemet's membrane, mild inflammation evident within the anterior chamber and fine keratic precipitates. Chronic. Occurs between 3 months and several years after the onset of the rash. Uncommon.
- Neurotrophic: corneal nerve damage causes persistent epithelial defect, thinning and even perforation. Cornea becomes susceptible to bacterial and fungal keratitis. Chronic. Late onset. Uncommon.
- Mucous plaques: linear grey elevations loosely adherent to the underlying diseased epithelium/stroma. Chronic. Onset between 3 months and several years after the onset of the rash.[3]
Uveal
Anterior uveitis develops in 40–50% of cases with HZO within 2 weeks of onset of the skin rashes. Typical HZO keratitis at least mild iritis, especially if Hutchinson's sign is positive for the presence of vesicles upon the tip of the nose.
Features:[4]
This non-granulomatous iridocyclitis is associated with:
- Small keratic precipitates
- Mild aqueous flare
- Occasionally haemorrhagic Hypopyon.
HZO uveitis is associated with complications such as iris atrophy and secondary glaucoma are not uncommon. Complicated cataract may develop in the late stages of the disease.
Treatment
Treatment is usually with antivirals such as acyclovir by mouth.
Uveal
- Cycloplegics prevent synechiae from forming. Avoid steroid use at all cost in the first week, as it will end either cause a corneal ulcer or worsen it dendritic ulcer. Steroids can be started after the virus has been suppressed and there are no other infections at the time.
- Acyclovir facilitates the early control of HZO lesions. 3% acyclovir can be applied topically: 3 to 5 drops a day. Systemic use of oral acyclovir is also possible: 800mg 5 times a day.[4]
References
- James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- "Oxford Handbook of Ophthalmology". google.com.au.
- "Comprehensive Ophthalmology". google.com.au.
External links
| Wikimedia Commons has media related to Herpes zoster ophthalmicus. |
| Classification | |
|---|---|
| External resources |
