Health in Nepal
Health care services in Nepal are provided by both public and private sectors and are generally regarded as failing to meet international standards. Prevalence of disease is significantly higher in Nepal than in other South Asian countries, especially in rural areas.[1][2] Moreover, the country's topographical and sociological diversity results in periodic epidemics of infectious diseases, epizootics and natural hazards such as floods, forest fires, landslides, and earthquakes.[2] A large section of the population, particularly those living in rural poverty, are at risk of infection and mortality by communicable diseases, malnutrition and other health-related events.[2] Nevertheless, some improvements in health care can be witnessed; most notably, there has been significant improvement in the field of maternal health. These improvements include:[3]
- Human Development Index (HDI) increased to 0.458 in 2011[4] from 0.291 in 1975.[5][6]
- Mortality rate during childbirth deceased from 850 out of 100,000 mothers in 1990 to 190 out of 100,000 mothers in 2013.[7]
- Mortality under the age of five decreased from 61.5 per 1,000 live births in 2005 to 31.4 per 1,000 live births in 2018.[8]
- Infant Mortality decreased from 97.70 in 1990 to 29.40 in 2015.[9]
- Child malnutrition: Stunting 37%, wasting 11%, and underweight 30% among children under the age of five.[10]
- Life expectancy rose from 66 years in 2005 to 71.5 years in 2018.[11][12]
| Population growth | 1.74[13] |
| Life expectancy | 71.5 [14] |
| Fertility | 2.18[15] |
| Infant mortality | 29.40[16] |
| Total expenditure on health per capita (Intl $, 2014) | 137[17] |
| Total expenditure on health as % of GDP (2014) | 5.8[17] |
Health care expenditure
In 2002, government funding for healthcare was approximately US$2.30 per person. Approximately 70% of health expenditure came from out-of-pocket contributions. Government allocation for health care was approximately 5.8% of the budget in 2009.[18] In 2012, the Nepalese government launched a pilot program for universal health insurance in five districts of the country.[19]
As of 2014, Nepal's total expenditure on health per capita was US$137.[20]
Health care infrastructure
Health care services, hygiene, nutrition, and sanitation in Nepal are of inferior quality and fail to reach a large proportion of the population, particularly in rural areas.[21] The poor have limited access to basic health care due to high costs, low availability, lack of health education and conflicting traditional beliefs.[22] Reproductive health care is limited and difficulties women. The United Nation's 2009 human development report highlighted a growing social concern in Nepal in the form of individuals without citizenship being marginalized, and denied access to government welfare benefits.[23][24][25]
These problems have led many governmental and non-governmental organizations (NGOs) to implement communication programs encouraging people to engage in healthy behavior such as family planning, contraceptive use, spousal communication and safe motherhood practices, such as the use of skilled birth attendants during delivery and immediate breastfeeding.[26]
Micro-nutrient deficiencies are widespread, with almost half of pregnant women and children under five, as well as 35% of women of reproductive age, being anaemic. Only 24% of children consume iron-rich food, 24% of children meet a minimally acceptable diet, and only half of the pregnant women take recommended iron supplementation during pregnancy. A contributing factor to deteriorating nutrition is high diarrhoeal disease morbidity, exacerbated by the lack of access to proper sanitation and the common practice of open defecation (44%) in Nepal.[27]
Nutrition of children under 5 years[28]
Periods of stagnant economic growth and political instability have contributed to acute food shortages and high rates of malnutrition, mostly affecting vulnerable women and children in the hills and mountains of the mid and far western regions. Despite the rate of individuals with stunted growth and the number of cases of underweight individuals having decreased, alongside an increase of exclusive breastfeeding in the past seven years, 41% of children under the age of five still suffer from stunted growth, a rate that increases to 60% in the western mountains. A report from DHS 2016, has shown that in Nepal, 36% of children are stunted (below -2 standard deviation), 12% are severely stunted (below -3 standard deviation), 27% of children under 5 are underweight, and 5% are severely underweight. Variation in the percentage of stunted and underweight children under 5 can be compared between urban and rural regions of Nepal, with rural areas being more affected (40% stunted and 31% underweight) than urban areas (32% stunted and 23% underweight). There is positive association between household food consumption scores and lower prevalence of stunting, underweight and wasting. Children in a secure food household have the lowest rates of stunting (33%), while children in an insecure food household have the highest rates (49%). Similarly, maternal education has an inverse relationship with childhood stunting. In addition, underweight and stunting issues are also inversely correlated to their equity possessions. Children in the lowest wealth quintile are more stunted (49%) and underweight (33%) than children in the highest quintile (17% stunted and 12% underweight).[29]
The nutritional status of children in Nepal has improved over the last two decades. Decreasing trends of children having stunted growth and being underweight have been observed since 2001. The percentage of stunted children in Nepal was 14% between 2001 and 2006, 16% between 2006 and 2011, and 12% between 2011 and 2016.[29] A similar trend can also observed for underweight children. These trends demonstrate progress towards the achievement of the Millennium Development Goal (MDG) target. However, there is still a long way to go to meet the SDG target of reducing stunting to 31% and underweight to 25% among children under 5 by 2017 (National Planning Commission 2015).
Micro-nutrient deficiencies are widespread, with almost half of pregnant women and children under five, as well as 35% of women of reproductive age, being anaemic. Only 24% of children consume iron-rich food, 24% of children meet a minimally acceptable diet, and only half of the pregnant women take recommended iron supplementation during pregnancy. A contributing factor to deteriorating nutrition is high diarrheal disease morbidity, exacerbated by the lack of access to proper sanitation and the common practice of open defecation (44%) in Nepal.[27]
| Urban areas | Rural areas | Overall | |
|---|---|---|---|
| Stunted | 27% | 42% | 41% |
| Wasted | 8% | 11% | 11% |
| Underweight | 17% | 30% | 29% |
Geographical constraints
Much of rural Nepal is located on hilly or mountainous regions. Nepal's rugged terrain and the lack of properly enabling infrastructure make it highly inaccessible, limiting the availability of basic health care in many rural mountain areas.[30] In many villages, the only mode of transportation is by foot. This results in a delay of treatment, which can be detrimental to patients in need of immediate medical attention.[31] Most of Nepal's health care facilities are concentrated in urban areas. Rural health facilities often lack adequate funding.[32]
In 2003, Nepal had 10 health centers, 83 hospitals, 700 health posts, and 3,158 "sub-health posts," which serve villages. In addition, there were 1,259 physicians, one for every 18,400 persons.[18] In 2000, government funding for health matters was approximately US$2.30 per person and approximately 70% of health expenditure came from contributions. Government allocations for health were around 5.1% of the budget for the 2004 fiscal year, and foreign donors provided around 30% of the total budget for health expenditure.[5]
Political influences
Nepal's health care issues are largely attributed to its political power and resources being mostly centered in its capital, Kathmandu, resulting in the social exclusion of other parts of Nepal. The restoration of democracy in 1990 has allowed the strengthening of local institutions. The 1999 Local Self Governance Act aimed to include devolution of basic services such as health, drinking water, and rural infrastructure but the program has not provided notable public health improvements. Due to a lack of political will,[33] Nepal has failed to achieve complete decentralisation, thus limiting its political, social and physical potential.[23]
Health status
Life expectancy
In 2010, the average Nepalese lived to 65.8 years. According to the latest WHO data published in 2012, life expectancy in Nepal is 68. Life expectancy at birth for both sexes increased by 6 years over the year 2010 and 2012. In 2012, healthy expectancy in both sexes was 9-year(s) lower than overall life expectancy at birth. This lost healthy life expectancy represents 9 equivalent year(s) of full health lost through years lived with morbidity and disability[11]
Disease burden
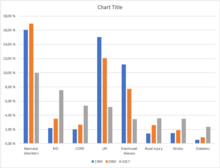
According to the Global Burden of Disease Study 2017, the eight leading causes of morbidity (illness) and mortality (death) in Nepal are: Neonatal disorders[34] (9.97%), Ischaemic Heart Disease (7.55%), COPD (5.35%), Lower respiratory infection (5.15%), Diarrhoeal disease (3.42%), Road injury[35] (3.56%), Stroke (3.49%), Diabetes (2.35%).[36]
The chart shows the burden of diseases prevalence in Nepal over the period of time. Diseases like neonatal disorder, lower respiratory tract infection and diarrhoeal diseases has shown gradual decrease in the prevalence over the period from 1990 to 2017. The reason for this decrease in number is due to the implementation of several health programs by the government with the involvement of other international organisations such as WHO and UNICEF for the maternal and child health, as these diseases are very common among the children. Whereas, there is remarkable increment in the number of other diseases like Ischemic heart disease (IHD), Chronic obstructive pulmonary disease (COPD), Road injuries, Stroke and Diabetes.
Ischemic heart disease
Ischemic Heart Disease (IHD) is gradually emerging as one of the major health challenge in Nepal. It is the most common type of heart disease and cause of heart attack. The rapid change in life style, unhealthy habits (smoking, sedentary life style etc.), economic development are considered to be responsible for the increase. Despite decrease in Ischemic Heart Disease mortality in developed countries, substantial increase have been experienced in developing countries like Nepal. IHD is the number one cause of death in adults from both low and middle income countries as well as from high income countries. The incidence of IHD is expected to increase by approximately 29% in women and 48% in men in the developed countries between 1990 and 2020.
A total of 182,751 deaths are estimated in Nepal for the year 2017. Non-communicable diseases (NCDs) are the leading causes of death – two-thirds (66%) of deaths are due to NCDs, with an additional 9% due to injuries. The remaining 25% are due to communicable, maternal, neonatal, and nutritional (CMNN) diseases. Ischemic heart disease (16.4% of total deaths), Chronic obstructive pulmonary disease (COPD) (9.8% of total deaths), Diarrheal diseases (5.6% of total deaths), Lower respiratory infections (5.1% of total deaths), and Intracerebral hemorrhage (3.8% of total deaths), were the top five causes of death in 2017[37]
Ischemic Heart Disease is second burden of disease and leading cause of death in Nepal for the last 16 years, starting from 2002. Death due to IHD is increasing in alarming rate in Nepal from 65.82 to 100.45 death per 100,000 from 2002 to 2017.[38] So, the large number of epidemiological research is necessary to determine the incidence & prevalence of IHD in Nepal and to identify the magnitude of the problem so that timely primary and secondary prevention can be done. As it is highly preventable and many risk factor are related to our lifestyle like; smoking, obesity, unhealthy diet, etc. So, knowledge and awareness regarding these risk factors is important in the prevention of IHD. Shahid Gangalal National Heart Center conducted cardiac camp in different part of Nepal from September 2008 to July 2011. The prevalence of heart disease was found higher in urban areas than rural areas where hypertension claims the major portion. The huge proportion of hypertension in every camp suggests that Nepal is in daring need of preventive programs of heart disease to prevent the catastrophic effect of IHD in near future. Also, according to this study the proportion of IHD ranges from 0.56% (Tikapur) to 15.12% (Birgunj) in Nepal.[39]
Among WHO region in European region, African region, Region of the Americas and Eastern Mediterranean death rate is in decreasing trend while in Western Pacific, South East Asia it is increasing.
[38]Table 1: Comparison of Death per 100,000 due to Ischemic Heart Disease Between Nepal, Global and 6 WHO Region
| Year | Global | Nepal | European Region | African Region | Western Pacific Region | South East Asia Region | Region of the America | Eastern Mediterranean |
| 1990 | 108,72 | 62,72 | 270,32 | 46,77 | 57,29 | 69,11 | 142,27 | 117,37 |
| 2004 | 108,33 | 69,05 | 278,53 | 45,53 | 77,75 | 74 | 114,73 | 114,51 |
| 2010 | 111,15 | 85,32 | 255,58 | 41,26 | 97,39 | 90,74 | 105,73 | 109,89 |
| 2017 | 116,88 | 100,45 | 245,3 | 39,26 | 115,94 | 103,47 | 111,91 | 112,63 |
Distribution according to age and sex :
Incidence of IHD occurs in men between 35 and 45 years age. After the age of 65 the incidence of men and women equalizes, although there is evidence suggesting that more women are being seen with IHD earlier because of increased stress, smoking and menopause.The risk of IHD increases as age increases. Middle aged adults are mostly affected by IHD .For men, the risk starts to climb at about age 45, and by age 55, the risk becomes double. It continues to increase until, by age 85. For women, the risk of IHD also climbs with age, but the trend begins about 10 years later than in men and especially with the onset of menopause
HIV/AIDS
Making up approximately 8.1% of the total estimated population of 40,723, there were about 3,282 children aged 14 years or younger living with HIV in Nepal in 2013. There are 3,385 infections estimated among the population aged 50 years and above (8.3% of the total population). By sex, males account for two‐thirds (66%) of the infections and the remaining, more than one‐third (34%) of infections are in females, out of which around 92.2% are in the reproductive age group of 15‐49 years. The male to female sex ratio of total infection decreased from 2.15 in 2006 to 1.95 in 2013 and is projected to be 1.86 by 2020.[40] The epidemic in Nepal is driven by injecting drug users, migrants, sex workers & their clients and MSM. Results from the 2007 Integrated Bio-Behavioral Surveillance Study (IBBS) among IDUs in Kathmandu, Pokhara, and East and West Terai indicate that the highest prevalence rates have been found among urban IDUs, 6.8% to 34.7% of whom are HIV-positive, depending on location. In terms of absolute numbers, Nepal's 1.5 million to 2 million labor migrants account for the majority of Nepal's HIV-positive population. In one subgroup, 2.8% of migrants returning from Mumbai, India, were infected with HIV, according to the 2006 IBBS among migrants.[41]
As of 2007, HIV prevalence among female sex workers and their clients was less than 2% and 1%, respectively, and 3.3% among urban-based MSM. HIV infections are more common among men than women, as well as in urban areas and the far western region of Nepal, where migrant labor is more common. Labor migrants make up 41% of the total known HIV infections in Nepal, followed by clients of sex workers (15.5 percent) and IDUs (10.2 percent).[41]
Maternal health
Nepal has made significant progress in improving the health of women and children and is on track in 2013 to achieve Millennium Development Goal (MDGs) No. 4 (to reduce child mortality) and #5A (to reduce maternal mortality). This review provided an opportunity for the MoHP and other stakeholders in Nepal to synthesize and document how these improvements were made, focusing on effective policy and program management practices.
Nepal has made significant progress in improving maternal health. Maternal mortality rate was reduced from 748 per 100,000 live births in 1990[42] to 190 per 100,000 live births on 2014. Nepal also has made some progress on reducing total fertility rate (TFR), from 5.3 in 1991[43] to 2.3 in 2014.[44]:241
Despite other indicators related to maternal health, the indicator of contraceptive prevalence rate is showing a decreasing trend: 2006 (44.2%) and 2011 (43.2%),[45] and has been attributed to high rates of spousal separation due to migration to other countries for employment (3/4 of youth in rural areas). The use of maternal health services has improved (increased) since 1996, with increases in the coverage and number of ANC visits (60% for at least four antenatal visits) in 2014,[44]:242 rates of institutional deliveries as well as deliveries attended by a skilled birth attendant (56%).[44]:242
Oral health

Oral health is an essential prerequisite for a healthy life. Attempting to maintain good oral health in developing countries like Nepal is a challenging task. According to the Annual report of Department of Health Services (2009/10),[44] 392,831 have dental caries/toothache, 73,309 have periodontal diseases, 62,747 and 113,819 have oral ulcer, mucosa and other related diseases. The data shows high prevalence of oral health problems in the population of the country. Many of these diseases in the population are due to poverty and lack of oral health awareness. According to the Journal of Nepal Dental Association National Oral Health 'Pathfinder' Survey 2004[46] shows prevalence of dental decay in adolescents studying in school is lower, which is 25.6% for 12 to 16 years of age. This can be due to the use of fluoridated toothpaste and awareness in the school going adults. However, periodontal/gum diseases cases tends to be higher in adolescents which is 62.8% for 12 to 13 years and 61% for 15 to 16 years. And the incidence of oral cancer ranges from 1 to 10 cases per 1,000,000 populations in most countries[47]
In countries like Nepal where majority of people are living under poverty, access to healthcare, education and awareness programs have been major constraints in improving oral health. High consumption of both smoked and smokeless form of tobacco in the people has been strongly associated with the majority of the oral health problems. Prevalence of cleaning teeth at least once a day was 94.9% , while that of cleaning teeth at least twice a day was measured to be only 9.9%. Use of fluoridated toothpaste was seen among 71.4%. It is also very common among people in the rural area to brush their teeth with the thin bamboo stick which is called "Datiwan" in the local language, sand and ash. And only 3.9% have made a dental visit in the last 6 months.[48]
Table: Distribution of oral hygiene practices among different age groups
| Age Groups (years) | Cleaning teeth at least once a day | Cleaning teeth at least twice a day | Fluoridated toothpaste | Dental visits (within 6 months) |
|---|---|---|---|---|
| 15-29 | 97.9% | 13.1% | 79.3% | 2.8% |
| 30-44 | 94.8% | 8.2% | 69.1% | 4.0% |
| 45-69 | 89.6% | 6.2% | 57.6% | 6.1% |
Government of Nepal do not advocate for institutions like WHO or UNICEF to provide the kind of support that they do for other medical issues because they do not prioritize oral health. Also several misconceptions are very relevant among people like loosening of teeth is normal with increasing age and losing some teeth won't kill people. Majority of people only seeks treatment when the disease has worsen up or causes unbearable pain.
Child health
Nepal is also on track to achieve MDG 4, having attained a rate of 35.8 under 5 child deaths per 1000 live births in 2015,[49] down from 162 in 1991[43] according to national data. Global estimates indicate that the rate has been reduced by 65% from 128 to 48 per 1000 live births between 1991 and 2013.[50] Nepal has successfully improved coverage of effective interventions to prevent or treat the most important causes of child mortality through a variety of community-based and national campaign approaches. These include high coverage of semiannual vitamin A supplementation and deworming; CB-IMCI; high rates of full child immunization; and moderate coverage of exclusive breastfeeding of children under 6 months. However, in the past few years, the NMR has remained stagnant with it being stated at around 22.2 deaths per 1000 live births in 2015. This compares to a rate of 27.7 in India (2015) and 45.5 in Pakistan (2015).[49]
The NMR is a serious concern in Nepal, accounting for 76% of the infant mortality rate (IMR) and 58% of the under 5 mortality rate (U5MR) as of 2015, and is one of its challenges going forward.[49] Typically, a history of conflict negatively affects health indicators. However, Nepal made progress in most health indicators despite its decade-long armed conflict. Attempts to understand this has provided a number of possible explanations including the fact that in most instances the former rebels did not purposely disrupt delivery of health services; pressure was applied on health workers to attend clinics and provide services in rebel base areas; the conflict created an environment for improved coordination among key actors; and Nepal's public health system adopted approaches that targeted disadvantaged groups and remote areas, particularly community-based approaches for basic service delivery with a functional community support system through female community health volunteers (FCHVs), women's groups and Health Facility Operational Management Committees (HFOMCs).[51]
Child health programmes
The Nepalese Child Health Division of the Ministry of Health and Population (MOHP), has launched several child survival interventions, including various operational initiatives, to improve the health of children in Nepal. These include the Expanded Program on Immunisation (EPI), the Community-Based Integrated Management of Childhood Illnesses (CB-IMCI) program, the Community-Based Newborn Care Program (CB-NCP), the Infant and Young Child Feeding program, a micro-nutrients supplementation program, vitamin A and deworming campaign, and the Community-Based Management of Acute Malnutrition program.[44]:29
Immunization
The National Immunisation Program is a priority 1 (P1) program in Nepal. Since the inception of the program, it has been universally established and successfully implemented. Immunisation services can be obtained for free from EPI clinics in hospitals, other health centers, mobile and outreach clinics, non-governmental organizations and private clinics. The government has provided all vaccines and immunization-related logistics without any cost to hospitals, private institutions, and nursing homes. Nepal has since gained recognition for the success of the program, in relation to its successful coverage of 97% population equally, regardless of wealth, gender and age. However, despite the widespread success of the National Immunisation Program, inequities still exist. Nevertheless, the trends in last past 15 years have shown promising positive changes indicating possibilities of achieving complete immunization coverage.[52] Two more vaccines were introduced between 2014 and 2015 – the inactivated poliomyelitis vaccine (IPV) and the pneumococcal conjugate vaccine (PCV). Six districts of Nepal are declared with 99.9% immunization coverage. Nepal achieved polio-free status on 27 March 2014. Neonatal and maternal tetanus was already eliminated in 2005 and Japanese encephalitis is in a controlled state. Nepal is also on track to meet the target of the elimination of measles by 2019.[44]:i,8 One percent of children in Nepal have not yet received any of the vaccine coverage.
Community-Based Integrated Management of Childhood Illnesses (CB-IMCI)
The Community-Based Integrated Management of Childhood Illness (CB-IMCI) program is an integrated package that addresses the management of diseases such as pneumonia, diarrhea, malaria, and measles, as well as malnutrition, among children aged 2 months to 5 years. It also includes management of infection, Jaundice, Hyperthermia and counseling on breastfeeding for young infants less than 2 months of age. CB-IMCI program has been implemented up to the community level in all the districts of Nepal and it has shown positive results in the management of childhood illnesses. Over the past decade, Nepal has had success in reducing under-five mortality, largely due to the implementation of the CB-IMCI program. Initially, the Control of Diarrheal Diseases (CDD) Program began in 1982; and the Control of Acute Respiratory Infections (ARI) Program was initiated in 1987. The CDD and ARI programs were merged into the CB-IMCI program in 1998.[45]
Community-Based Newborn Care Program (CB-NCP)
The Nepal Family Health Survey 1996, Nepal Demographic and Health Surveys, and World Health Organization estimations over time have shown that neonatal mortality in Nepal has been decreasing at a slower rate than infant and child mortality. The Nepal Demographic and Health Survey 2011 has shown 33 neonatal deaths per 1,000 live births, which accounts for 61% of under 5 deaths. The major causes of neonatal death in Nepal are an infection, birth asphyxia, preterm birth, and hypothermia. Given Nepal's existing health service indicators, it becomes clear that strategies to address neonatal mortality in Nepal must consider the fact that 72% of births take place at home (NDHS 2011).[45]
Therefore, as an urgent step to reduce neonatal mortality, Ministry of Health and Population (MoHP) initiated a new program called 'Community-Based Newborn Care Package' (CB-NCP) based on the 2004 National Neonatal Health Strategy.[45]
National Nutritional Program
The National Nutrition Program under the Department of Health Services has set it's ultimate goal as "all Nepali people living with adequate nutrition, food safety and food security for adequate physical, mental and social growth and equitable human capital development and survival" with the mission to improve the overall nutritional status of children, women of childbearing age, pregnant women, and all ages through the control of general malnutrition and the prevention and control of micronutrient deficiency disorders having a broader inter and intra sectoral collaboration and coordination, partnership among different stakeholders and high level of awareness and cooperation of population in general.[53]
Malnutrition remains a serious obstacle to child survival, growth, and development in Nepal. The most common form of malnutrition is protein-energy malnutrition (PEM). Other common forms of malnutrition are iodine, iron, and vitamin A deficiency. These deficiencies often appear together in many cases. Moderately acute and severely acutely malnourished children are more likely to die from common childhood illness than those adequately nourished. In addition, malnutrition constitutes a serious threat to young children and is associated with about one-third of child mortality. Major causes of PEM in Nepal is low birth weight of below 2.5 kg due to poor maternal nutrition, inadequate dietary intake, frequent infections, household food insecurity, poor feeding behaviour and poor care & practices leading to an intergenerational cycle of malnutrition.[54]
An analysis of the causes of stunted growth in Nepal reveals that around half is rooted in poor maternal nutrition, and the other half in poor infant and young child nutrition. Around a quarter of babies are born with a low birth weight. As per the findings of Nepal Demographic and Health Survey (NDHS, 2011), 41 percent of children below 5 years of age are stunted. A survey by NDHS and NMICS also showed that 30% of the children are underweight and 11% of children below 5 years are wasted.[44]:241
In order to address under-nutrition problems in young children, the Government of Nepal (GoN) has implemented:
- a) Infant and Young Child Feeding (IYCF)
- b) Control of Protein Energy Malnutrition (PEM)
- c) Control of Iodine Deficiency Disorder (IDD)
- d) Control of Vitamin A Deficiency (VAD)
- e) Control of Iron Deficiency Anaemia (IDA)
- f) Deworming of children aged 1 to 5 years and vitamin A capsule distribution
- g) Community Management of Acute Malnutrition (CMAM)
- h) Hospital-based nutrition management and rehabilitation
The hospital-based nutrition management and rehabilitation program treats severe malnourished children at Out-patient Therapeutic Program (OTP) centres in Health Facilities. As per requirement, the package is linked with the other nutrition programs such as the Child Nutrition Grant, Micronutrient powder (MNP) distribution to young children (6 to 23 months)[44]:22,24 and food distribution in the food insecure areas.
Infant and Young Child Feeding program
UNICEF and WHO recommended that children be exclusively breastfed (no other liquid, solid food, or plain water) during the first six months of life (WHO/UNICEF, 2002). The nutrition program under the 2004 National Nutrition Policy and Strategy promotes exclusive breastfeeding through the age of 6 months and, thereafter, the introduction of semisolid or solid foods along with continued breast milk until the child is at least age 2. Introducing breast milk substitutes to infants before age 6 months can contribute to breastfeeding failure. Substitutes, such as formula, other kinds of milk and porridge are often watered down and provide too few calories. Furthermore, possible contamination of these substitutes exposes the infant to the risk of illness. Nepal's Breast Milk Substitute Act (2049) of 1992 promotes and protects breastfeeding and regulates the unauthorized or unsolicited sale and distribution of breast milk substitutes.[55]
After six months, a child requires adequate complementary foods for normal growth. Lack of appropriate complementary feeding may lead to malnutrition and frequent illnesses, which in turn may lead to death. However, even with complementary feeding, the child should continue to be breastfed for two years or more.[55]
Practice of exclusive breastfeeding after Normal delivery and C section
Adequate nutrition during infancy is crucial for child survival, optimal growth and development throughout life. It has been postulated that 13% of the current under five mortality rate could be averted by promoting proper breastfeeding practices, which is seemingly the single most cost effective intervention to reduce child mortality in resource-constrained settings such as in Nepal.Childhood malnutrition and growth faltering affects more than half of children under five in developing countries, and usually starts during infancy, possibly due to improper breastfeeding and mixed feeding practices.[56]
According to WHO, exclusive breastfeeding is defined as no other food or drink, not even water, except breastmilk (including milk expressed or from a wet nurse) for 6 months of life, but allows the infant to receive ORS, drops and syrups (vitamins, minerals and medicines). Exclusive breastfeeding for the first 6 months of life is the recommended way of feeding infants, followed by continued breastfeeding with appropriate complementary foods for up to 2 years or beyond.[57]
As per the study carried out in Paropakar Maternity & Women's Hospital, Thapathali, 2017, the participants of normal delivery had an opportunity to breastfeed within an hour while almost all participants going through C section were not offered to do so.[57]
The reason for participants to not practice breastfeeding within an hour were mother's sickness, unable to hold the baby due to suture, baby taken away from mother and less or no production of breast milk soon after surgery to feed the child. In addition, (as shown in table below) 84.7% of normal delivery participants did not feed anything other than breast milk to their babies while 78% of C sectioned participants fed formula to their babies after they had started breastfeeding.
| Methods of delivery | Fed anything other than breast milk to baby | Percent |
| Normal delivery | Yes | 15.33 |
| No | 84.66 | |
| Total | 100 | |
| Cesarean delivery | Yes | 56 |
| No | 44 | |
| Total | 100 |
The participants assumed that formula fed babies were more likely to gain weight more quickly than breastfeed babies. These might be the major increasing drawbacks for the practice of exclusive breastfeeding in Nepal.
The perspective towards breastfeeding is found to be optimistic, believing to the benefits of breastfeeding were not only for limited period; is always convenient, healthier and cheaper than formula. Exclusive breastfeeding has always been considered as an ideal food for the baby up to six months after birth.
We can say that mode of delivery is significant with initiation of breastfeeding within an hour. Which means the practice of exclusive breastfeeding is higher among normal deliveries than c-sections. From analysis of Nepal demographic and health survey, 2011; Two in every three mothers had initiated breastfeeding within one hour of childbirth.[57]
In some cultures including Nepal there is a preference for the introduction of prelacteal feeds. Economic status and the mother's education status were significant factors associated with the introduction of prelacteal feeds. The lower socio-economic groups have less access to the expensive prelacteal feeds such as ghee or honey and therefore exclusive breastfeeding is the only option available. This might be a reason for the reported lower prelacteal feeding practice rates amongst the poorest wealth groups in Nepal.[58]
Geriatric health

There are no active and effective policies and programs to mainstream aging population in national, social and political discourse in Nepal. About 9% of the total population accounts for 60+ populations and the number is projected to be around 20% by 2050. The decline in fertility rate and increased life expectancy is the main cause for the increased number of old age people in Nepal.[59] Increase in the number of aged people and availability of no healthcare services in a developing country like Nepal, aging could be a matter of challenge.
Geriatric services
Out of 2.1million elderly people (2011 census), only 3 geriatric specialists are registered to take care of them. Nepal not only lacks geriatric specialists, but geriatric nurses and caregivers are also lacking.[60] There is only one shelter for elderly people run by the government (Pashupatinath Bridrashram) which was established in 1976 as the first residential facility for elders and has the capacity for only 230 elderly people. Official data of Social Welfare Council shows that the total number of old age homes (OAHs) registered as of 2005 was 153. However, most of these homes either do not exist today or operate in very poor condition. Only about twenty homes are currently functional throughout the country.[61] These organizations vary in their organizational status (government, private, NGO, personal charity), capacity, facilities, and the services they provide. Most of them are charity organizations. About 1,500 elders are living in these old-age homes at present.[62]
Government has initiated to provide geriatric care services by formulating certain plans and policies but these could not be effective due to lack of resources. Madrid Plan of Action on Aging (2002), Senior Citizen Policy (2002), National Plan of Action on Aging (2005), Senior Citizen Act (2006) and The senior Citizens regulations (2008) are the initiatives taken by Nepal government. The Ministry of Health and Population started social service units in 8 hospitals and geriatric wards in 3 hospitals. About 70 registered old age homes are available in the country out of which 11 get government grants.
In March 2012, a residential health care home for elderly people named Health Home Care Nepal with 15 beds was established by private investment. It aims to provide comprehensive holistic package services for needy elderly people. It was the first model care home managed by medical professionals.[63]Old age homes which are giving services for free in Nepal are listed below:
– Sri Sathya Sai Seva organisation
Geriatric diseases
There is little baseline information on the prevalence of geriatric diseases among the elderly which is an obstacle for health care planning and management. Prevalence of chronic diseases in old age is a common phenomenon. Most of the common geriatric diseases in Nepal include gastritis, arthritis, hypertension, COPD, infections, eye problems, back pain, dementia, headache, diabetes, paralysis and heart problems.[64] Specific and exact data related to geriatric population is lacking behind as this section is not more concerned as that of child and women health. More research should be conducted from the public level to get the specific data which can give a focussed idea to develop effective health policies for the old people.
The table below shows the status of diseased state of elderly people in a certain number of aged people in Kathmandu.
| Major Chronic Health Problem | % (N= 509) |
|---|---|
| High Blood Pressure | 39.7 |
| Diabetes | 22.3 |
| Respiratory Diseases | 21.7 |
| Arthritis | 16 |
| Back Pain | 14.3 |
| Heart diseases | 8.3 |
| Liver and Gull Bladder Diseases | 4.7 |
| Bone Fracture | 4.7 |
| Stroke | 4.3 |
| Cancer | 0.7 |
source: Socio-Demographic and Health Status of Nepalese Elderly [65]
These are the only data from a specific place in a specific number of people. More research and studies are to be conducted at the national level to know the exact health status of elderly people in Nepal. The government of Nepal should focus its concern in this field so that elderly from Nepal can get some heath benefits. More research should be conducted from the public level to get the specific data which can give a focussed idea to develop effective health policies for the old people.
Road traffic accidents
Road traffic injuries are one of the global health burdens, an eighth leading cause of death worldwide. Globally, approximately 1.25 million lives are cut short every year because of a road traffic injuries. Ranging from 20 to 50 million people become victims of non-fatal injuries, with many acquiring a disability for the rest of the life as a result of their injury.[66] In Nepal, a road traffic accident rank eighth among killer causes of disability-adjusted life years and also eighth among premature cause of death after Non-Communicable Diseases and Communicable Diseases.[67]
A substantial problem of road traffic accident with fatalities occurs mainly on highways caused by bus crashes in Nepal. Due to the country's geography, bus accidents mostly happen in the hilly region and along the long-distance route causing 31 percent of fatalities and serious injuries every year.[68] Accidents involving motorcycles, micro-buses, cars etc. highly prevail in the capital city, Kathmandu compared to other cities and lowland areas. The number of Road Traffic Accidents in the capital city was (53.5±14.1) of the number for the entire country.[69] People between 15 and 40 ages are the most affected group followed by those above 50 years and majorities were male making 73 percent of disability-adjusted life years. The number of registered vehicles in Bagmati Zone was 129,557, a 29.6 percent of the whole nation in fiscal year 2017/2018.[70][69]
The table below shows the trend of fatality per 10000 vehicles between 2005 and 2013.
| Year | Accidents | Fatalities | Total Vehicles | Fatality per 10000
vehicles |
|---|---|---|---|---|
| 2005-6 | 3894 | 825 | 536443 | 15.38 |
| 2006-7 | 4546 | 953 | 625179 | 15.24 |
| 2007-8 | 6821 | 1131 | 710917 | 15.91 |
| 2008-9 | 8353 | 1356 | 813487 | 16.67 |
| 2009-10 | 11747 | 1734 | 1015271 | 17.08 |
| 2010-11 | 140131 | 1689 | 1175824 | 14.36 |
| 2011-12 | 14291 | 1837 | 1342927 | 13.68 |
| 2012-13 | 13582 | 1816 | 1545988 | 11.75 |
source: Traffic Accidents Record, Traffic Directorate, Nepal Police, 2013.[70]
Mental health
In terms of the network of mental health facilities, there are 18 outpatient mental health facilities, 3-day treatment facilities, and 17 community-based psychiatric inpatient units available in the country. The majority of the mental health service users are treated in outpatient facilities. Thirty-seven percent of patients are female. The patients admitted to mental hospitals belong primarily to the following two diagnostic groups: Schizophrenia, schizotypal and delusional disorders (34%) and Mood [affective] disorders (21%). On average, patients spend 18.85 days in mental hospitals. All of the patients spent less than one year in the mental hospital during the year of assessment.
Two percent of the training for medical doctors is devoted to mental health, and the same percentage is provided for nurses. One Non Government Organization is running a community mental health service in 7 of the 75 districts in the country. In other districts, community mental health services are not available, as mental health services are not yet integrated into the general health service system.
Even though Nepal's mental health policy was formulated in 1996, there is no mental health legislation as yet. In terms of financing, less than one percent (0.17%) of health care expenditures by the government are directed towards mental health. There is no human right review body to inspect mental health facilities and impose sanctions on those facilities that persistently violate patients' rights.[71]
See also
- Gender inequality in Nepal
References
- "REBUILDING NEPAL'S HEALTHCARE SYSTEM". Possible Health.
- "Health System in Nepal: Challenges and Strategic Options" (PDF). World Health Organization. November 2007.
- Nepali Times Issue #561 (8 July 2011 – 14 July 2011)
- "gapminder world". gapminder.org. Retrieved 6 September 2016.
- Nepal country profile. Library of Congress Federal Research Division (November 2005). This article incorporates text from this source, which is in the public domain.
- HDI 2010 index from article Let's Talk Human Development - Data challenges in estimating the HDI: The cases of Cuba, Palau and the Occupied Palestinian Territory
- "gap minder world". gapminder.org. Retrieved 6 September 2016.
- "gapminder world". Retrieved 6 September 2016.
- "gapminder world". gapminder.org. Retrieved 6 September 2016.
- "Annual_Report_FY_2071_72" (PDF). dohs.gov.np. Retrieved 7 September 2016.
- "Nepal: WHO Statistical Profile". who.int. Retrieved 12 September 2016.
- "Gapminder Tools". Retrieved 9 September 2018.
- "world bank". gapminder.org. Retrieved 7 September 2016.
- "Nepal: Country Profile". who.int. Retrieved 11 September 2016.
- "gapminder world". gapminder.org. Retrieved 7 September 2016.
- "gapminder world". gapminder.org. Retrieved 7 September 2016.
- "WHO". Retrieved 7 September 2016.
- Nepal Health Profile World Health Organisation data (2010)
- "Health for all". My Republica. Archived from the original on 9 November 2012. Retrieved 14 November 2012.
- "Nepal". World Health Organization. Retrieved 18 March 2018.
- "HEALTH CARE SERVICES IN NEPAL OFFERING COMPREHENSIVE HEALTH CARE AND EDUCATION TO UNDER-SERVED COMMUNITIES". Karuna-Shechen Humanitarian Projects in the Himalayan Region.
- Beine, David. 2001. "Saano Dumre Revisited: Changing Models of Illness in a Village of Central Nepal
- Nepal human development report 2009-State transformation and human development by United Nations Development Programme
- Contributions to Nepalese Studies 28(2): 155-185.
- Beine, David. 2003. Ensnared by AIDS: Cultural Contexts of HIV/AIDS in Nepal. Kathmandu, Nepal: Mandala Book Point.
- Karki, Yagya B.; Agrawal, Gajanand (May 2008). "Effects of Communication Campaigns on the Health Behavior of Women of Reproductive Age in Nepal, Further Analysis of the 2006 Nepal Demographic and Health Survey" (PDF). Macro International Inc. Retrieved 14 November 2012.
- "Nepal: Nutrition Profile" (PDF). usaid.gov. Retrieved 10 September 2016.
- Nepal Demographic and Health Survey. Nepal: Ministry of Health and Population. 2011.
- Nepal Demographic and Health Survey. Nepal: Ministry of Health and Population. 2016.
- International Fund for Agricultural Development (IFAD) retrieved 20 September 2011
- United Methodist Committee on relief; retrieved on 20 September 2011
- Shiba Kumar Rai, Kazuko Hirai, Ayako Abe, Yoshimi Ohno 2002 "Infectious Diseases and Malnutrition Status in Nepal: an Overview"
- Raj Panta, Krishna PhD. "Decentralization of Corruption and Local Public Service Delivery in Nepal" (PDF). Nepal Rastra Bank.
- "Neonatology Conferences 2019 | Perinatology Conferences | Fetal Medicine conferences | Pediatrics conferences 2019 | Neonatal Conferences | Kyoto | Japan". neonatologycongress.pediatricsconferences.com. Retrieved 17 September 2019.
- "Road traffic injuries". www.who.int. Retrieved 17 September 2019.
- "Nepal: Country Profile". vizhub.healthdata.org. Retrieved 16 September 2016.
- "NEPAL BURDEN OF DISEASE 2017" (PDF).
- "GBD Compare | IHME Viz Hub". vizhub.healthdata.org. Retrieved 19 September 2019.
- "Current cenario of Heart Diseases in Nepal: At a glance".
- "annual health report" (PDF). dohs.gov.np. Retrieved 11 September 2016.
- "Health Profile: Nepal" (PDF). United States Agency for International Development. March 2008. Archived from the original (PDF) on 17 August 2008. Retrieved 25 August 2008.

- "Gap minder : Maternal mortality rate 1991 Nepal". Gapminder. Retrieved 4 September 2016.
- Nepal fertility, family planning and health survey: (NFHS, 1991). Kathmandu Nepal. 1993.
- "Annual Report 2013/2014" (PDF). Ministry of Health and Population of Nepal, Department of Health Services. January 2015. Retrieved 24 January 2017.
- "Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population (MoHP), New ERA and ICF International, Calverton, Maryland; 2012" (PDF).
- "JNDA : National Pathfinder Survey in Nepal". jnda. Retrieved 17 September 2019.
- "Oral health : oral health in Nepal". dentistryiq. Retrieved 16 September 2019.
- Thapa, P.; Aryal, K. K.; Mehata, S.; Vaidya, A.; Jha, B. K.; Dhimal, M.; Pradhan, S.; Dhakal, P.; Pandit, A.; Pandey, A. R.; Bista, B.; Pokhrel, A. U.; Karki, K. B. (2016). "NCBI : Oral hygiene practice in Nepal". BMC Oral Health. 16: 105. doi:10.1186/s12903-016-0294-9. PMC 5041565. PMID 27686858.
- "World Development Indicators [online database]. Washington DC: The World Bank; 2015". World Development Indicators [online database]. Retrieved 6 September 2016.
- "Gapminder Under five mortality from 1991 to 2011". Gapminder. Retrieved 6 September 2015.
- Devkota, Bhimsen (1 December 2010). "Understanding effects of armed conflict on health outcomes: the case of Nepal". Conflict and Health. 4: 20. doi:10.1186/1752-1505-4-20. PMC 3003631. PMID 21122098.
- Kc, Ashish; Nelin, Viktoria; Raaijmakers, Hendrikus; Kim, Hyung Joon; Singh, Chahana; Målqvist, Mats (2017). "Increased immunization coverage addresses the equity gap in Nepal". Bulletin of the World Health Organization. 95 (4): 261–269. doi:10.2471/BLT.16.178327. PMC 5407251. PMID 28479621. Retrieved 9 September 2017.
- Multi-sector Nutrition Plan 2013-2017 (2023). http://scalingupnutrition.org/wp-content/uploads/2013/03/Nepal_MSNP_2013-2017.pdf: GOVERNMENT OF NEPAL / National Planning Commission. 2013.
- "A case-control study on risk factors associated with malnutrition in Dolpa district of Nepal". Retrieved 11 September 2016.
- Policy - Mother's Milk Substitutes (Control of Sale and Distribution) Act, 2049 (1992). https://extranet.who.int/nutrition/gina/sites/default/files/NPL%201992%20Mother%27s%20Milk%20Substitues%20Control%20of%20sale%20and%20distribution%20Act%202049.pdf.
- Strand, Tor A.; Shrestha, Prakash S.; Mellander, Lotta; Chandyo, Ram K.; Ulak, Manjeswori (January 2012). "Infant feeding practices in Bhaktapur, Nepal: a cross-sectional, health facility based survey". International Breastfeeding Journal. 7 (1): 1–8. doi:10.1186/1746-4358-7-1. ISSN 1746-4358. PMC 3285083. PMID 22230510.
- Sharma, Kashyap Kumar; Aryal, Rachana (25 November 2017). "Comparative Study between the Practices of Exclusive Breastfeeding After Normal Delivery and Cesarean Delivery in Paropakar Maternity and Women's Hospital, Thapathali, Kathmandu Nepal". Advanced Journal of Social Science. 1 (1): 40–52. doi:10.21467/ajss.1.1.40-52. ISSN 2581-3358.
- Khanal, Vishnu; Adhikari, Mandira; Sauer, Kay; Zhao, Yun (8 August 2013). "Factors associated with the introduction of prelacteal feeds in Nepal: findings from the Nepal Demographic and Health Survey 2011". International Breastfeeding Journal. 8 (1): 9. doi:10.1186/1746-4358-8-9. ISSN 1746-4358. PMC 3750657. PMID 23924230.

- http://ageingnepal.org/monthly-discussion-forum-on-ageing-annual-report-2018/
- https://kathmandupost.com/health/2019/08/29/without-specialised-care-older-adults-deprived-of-basic-health-care-facilities
- http://ageingnepal.org/wp-content/uploads/2015/05/OAH-Study-Final.pdf
- USAID Country Health Statistical Report Nepal December 2009. Retrieved on 12 November 2010 form http://pdf.usaid.gov/pdf_docs/PNADR595.pdf
- https://www.ifa-fiv.org/wp-content/uploads/2013/03/IFA-presentation-2014.pdf
- http://ageingnepal.org/wp-content/uploads/2015/05/OAH-Study-Final.pdf
- https://www.academia.edu/28571934/Socio-Demographic_and_Health_Status_of_Nepalese_Elderly
- "Road traffic injuries". World Health Organization. Retrieved 9 September 2018.
- "Nepal | Institute for Health Metrics and Evaluation". www.healthdata.org. 9 September 2015. Retrieved 9 September 2018.
- "opennepal/datasources" (PDF). GitHub. 6 March 2018. Retrieved 9 September 2018.
- Huang, Ling; Poudyal, Amod K.; Wang, Nanping; Maharjan, Ramesh K.; Adhikary, Krishna P.; Onta, Sharad R. (1 October 2017). "Burden of road traffic accidents in Nepal by calculating disability-adjusted life years". Family Medicine and Community Health. 5 (3): 179–187. doi:10.15212/fmch.2017.0111. ISSN 2305-6983.
- "Annual Accidental Description". traffic.nepalpolice.gov.np. Retrieved 9 September 2018.
- "Organization of mental health services in developing countries: Sixteenth Report of the WHO Expert Committee on Mental Health". 1975. doi:10.1037/e409862004-001. Cite journal requires
|journal=(help)
External links
- The State of the World's Midwifery - Nepal Country Profile