Cardiac allograft vasculopathy
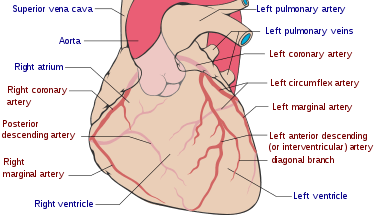
Cardiac allograft vasculopathy (CAV) is a common long-term complication of heart transplantation affecting up to half of people within 10 years.[1][2] It arises when the blood vessels supplying the transplanted heart gradually narrow and restrict its blood flow, subsequently leading to impairment of the heart muscle or sudden death.[3] The other major causes of death following heart transplantation include graft failure, organ rejection and infection.[4]
| Cardiac allograft vasculopathy | |
|---|---|
 | |
| Coronary arteries | |
| Specialty | Cardiology, angiology |
| Usual onset | After heart transplantation |
| Frequency | Up to 50% (in 10 years) |
People with CAV may present with a wide range of symptoms including tiredness and breathlessness, but there is typically no chest pain. As well as the same risk factors for coronary artery disease due to atherosclerosis, CAV risk factors also include older donors, cytomegalovirus infection and explosive brain death in the donor.[1]
Its pathogenesis involves immunological (innate and adaptive) and nonimmunological factors, with distinct features on histological samples of coronary arteries.[1]
Diagnosis is by regular follow-up and monitoring of the transplanted heart for early signs of disease. This involves invasive diagnostics including coronary angiography and intravascular ultrasound, and non-invasive investigations including dobutamine stress echocardiography, positron emission tomography, computed tomographic angiography (CT angiography) and a variety of biomarkers.[1]
Statins and aspirin are commenced early after transplantation and on detection of CAV. Medications including sirolimus and everolimus can slow disease progression, but a repeat heart transplantation may be needed.[1]
Signs and symptoms
Unlike the ischaemic chest pain in those who have not had a heart transplant, people with CAV typically do not experience chest pain because the donor heart is denervated. A few reinnervate some years later and may develop atypical chest pain.[5] People with CAV may present with a broad spectrum of symptoms including tiredness, nausea, or abdominal discomfort or may have no symptoms at all.[1] Shortness of breath and arrythmias may also occur.[5]
Risk factors
Similar to coronary artery disease in those who have not had a heart transplant, risk factors to CAV include high blood pressure, high cholesterol, and diabetes mellitus. Other risk factors exclusive to CAV include older donors, cytomegalovirus infection and circulating antibodies after heart transplantation.[1] The mechanism of donor brain death,[5] particularly explosive brain death in the donor has been shown to be a significant factor. It is probably the combination of injuries to the allograft that determine the risk of developing CAV.[1]
Mechanism
Immunological (innate and adaptive) and nonimmunological factors contribute to the complex pathogenesis of CAV.[1]
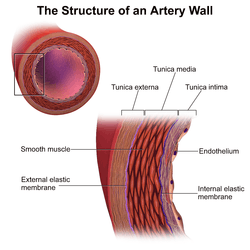
In those nontransplanted people who develop coronary artery disease due to atherosclerosis, progression of disease is slow, histological changes are confined mainly to the main coronary arteries and arterial dilatation is observed as a form of compensatory remodelling.[5] However, in CAV, histology specimens typically show concentric thickening of the intimal layer of the main coronary arteries on the surface of the heart and in intramyocardial arteries[1] which can become obliterated within a few years.[5] There is smooth muscle cell migration, foamy macrophages and lymphocytic infiltrates. This can be seen to affect the whole length of the coronary arteries and often the smaller arteries.[1] Calcification does not always occur in CAV and if it does appear, it happens late. The compensatory arterial dilation does not occur in CAV.[5] Unlike in nontransplanted people with coronary artery disease due to atherosclerosis, in CAV occlusion with thrombus of the vessel lumen is rare.[1]
Inflammation and endothelial injury can be triggered by the donor arrest, organ procurement, and allograft ischaemia and reperfusion.[1]
Diagnosis
As symptoms are so variable and often absent, diagnosis has been a challenge. Hence, regular follow-up and monitoring of the allograft for early signs of disease is advocated.[1]
Coronary angiography
Surveillance is performed by regularly repeating coronary angiography in the cardiac catheterization laboratory, the diagnostic test of choice.[1] This is typically performed annually for the first five years after transplantation.[5] Angiography in CAV characteristically demonstrates diffuse stenoses in large coronary arteries and a reduced number of smaller coronary arteries, also known as "peripheral pruning".[1][2] However, because CAV frequently affects the entire length of the coronary artery, CAV may not be apparent by angiography alone.[1]
Intravascular ultrasound (IVUS)
Intravascular ultrasound (IVUS) is more sensitive at reliably detecting subtle changes in the thickness of the intimal layer of the artery walls and provide measurements of artery lumen. Following transplantation, serial measurements are compared to the baseline. A greater than 0.5 mm increase in intimal thickness one year after transplantation is predictive of CAV changes on angiography within five years. The paradoxical reduction in the number of blood vessels, can also be detected by intravascular ultrasound.[1][5]
IVUS, however, tends to be used for research due to its drawbacks of being invasive, requiring the use of contrast material and cost.[5]
Dobutamine stress-echocardiography (DSE)
Alternatively, dobutamine stress echocardiography (DSE) is commonly performed and has an 85% sensitivity for the presence of CAV. A negative DSE correlates with a good prognosis.[5]
Other noninvasive diagnostics include positron emission tomography and computed tomographic angiography (CT angiography).[1] In addition, ECGs may show atypical features of ischaemia.[5]
Biomarkers
Biomarkers for increased risk of CAV include C-reactive protein, serum brain natriuretic peptide and troponin I have been suggested.[1]
Classification
The degree of CAV after heart transplantation has been obtained from a variety of sources including The Cardiac Transplant Research Database, the ISHLT registry and The United Network for Organ Sharing registry.[5]
The International Society for Heart and Lung Transplantation (ISHLT) have formulated and standardized a terminology, based on diagnostic findings, to define the presence and severity of CAV, which in turn reflects prognosis.[5][7] The severity of CAV is defined by the degree of narrowing of the coronary arteries and the presence of restrictive heart disease.[5]
| Code | Severity | Diagnostic findings |
|---|---|---|
| ISHLT CAV0 | Not significant | No detectable lesions on angiography |
| ISHLT CAV1 | Mild | Angiographic left main (LM) 50%, or primary vessel with maximum lesion of 70%, or any branch stenosis 70% (including diffuse narrowing) without allograft dysfunction |
| ISHLT CAV2 | Moderate | Angiographic LM 50%; a single primary vessel 70%, or isolated branch stenosis 70% in branches of 2 systems, without allograft dysfunction |
| ISHLT CAV3 | Severe | Angiographic LM 50%, or two or more primary vessels 70% stenosis, or isolated branch stenosis 70% in all 3 systems; or ISHLT CAV1 or CAV2 with allograft dysfunction (defined as LVEF 45% usually in the presence of regional wall motion abnormalities) or evidence of significant restrictive physiology |
Treatment
Statins
Prevention of CAV progression is important as once developed, CAV existing treatments are often ineffective. Commencing the statins pravastatin and simvastatin early after transplantation reduce the incidence and severity of CAV.[1][5]
Vitamins
When combined with immunosuppressants, the progression of CAV could possibly be slowed by vitamins C and E.[5]
Aspirin
Since the role of aspirin is already established in coronary artery disease in those who have not had a heart transplant, it is usually given after heart transplantation too.[1]
Antiproliferative agents
On detection of CAV, medications including mTOR inhibitors sirolimus and everolimus have been shown to slow disease progression.[1]
Other treatment options
Clinically significant CAV may require percutaneous coronary interventions for focal disease, but the likelihood of restenosis is high. A repeat heart transplantation may be considered.[1]
Prognosis
Once there is reduced left ventricular ejection fraction and symptoms of heart failure, the prognosis is typically poor.[1]
The risk of major adverse cardiovascular events is increased by 3.4 fold if CAV is present on angiography.[5]
Epidemiology
The frequency of CAV after heart transplantation has been obtained from a variety of sources including The Cardiac Transplant Research Database, the ISHLT registry and The United Network for Organ Sharing registry.[5] In comparison to between 1994 and 2001, there has been a decline in incidence of CAV between 2001 and 2007. ISHLT figures show an incidence of CAV of around 50% at 10 years after heart transplantation.[5]
CAV is a leading cause of late mortality following heart transplantation.[1]
History
Unlike rejection and infection, CAV in the transplanted heart was not initially a predicted outcome. Early survivors of heart transplants soon developed this form of vasculopathy of their coronary arteries, initially identified at the post-mortems. There were early suggestions that preventing cytomegalovirus (CMV) infection could decrease the prevalence of CAV. The impact of CAV has changed over time, with early recipients being younger, having more rejection and cardiovascular risk factors and less use of statins. Later recipients used statins routinely and were introduced to the immunosuppressive agent mycophenolate mofetil (MMF) and CMV prophylaxis. In addition, the later recipients were monitored for antibody-mediated cardiac allograft rejection (AMR).[9]
Before 2010 there was no uniform international standards for the nomenclature of CAV. A consensus statement on a standard language for CAV was first published in 2010 by the ISHLT.[3] This was devised in a similar way to the earlier acute rejection grading system by endomyocardial biopsy.[7][10]
Research directions
Antibody-mediated cardiac allograft rejection (AMR) is a significant factor leading to the rapid progression of CAV. Future research directions in this area may include prospective databases that correlate clinical factors with surveillance of the incidence and severity of AMR, the frequency of CMV infection, and the use of immunosuppressants. The role of inducing immune tolerance has yet to be established.[9]
References
- Stehlik Josef; Kobashigawa Jon; Hunt Sharon A.; Reichenspurner Hermann; Kirklin James K. (2 January 2018). "Honoring 50 Years of Clinical Heart Transplantation in Circulation". Circulation. 137 (1): 71–87. doi:10.1161/CIRCULATIONAHA.117.029753. PMID 29279339.
- Lee, Michael S.; Tadwalkar, Rigved V.; Fearon, William F.; Kirtane, Ajay J.; Patel, Amisha J.; Patel, Chetan B.; Ali, Ziad; Rao, Sunil V. (2018-12-01). "Cardiac allograft vasculopathy: A review". Catheterization and Cardiovascular Interventions. 92 (7): E527–E536. doi:10.1002/ccd.27893. ISSN 1522-726X. PMID 30265435.(subscription required)
- Elsevier (2010). "New ISHLT Cardiac Allograft Vasculopathy Standardized Nomenclature: A Common International Definition Will Benefit Heart Transplant Patients". www.elsevier.com. Elsevier. Retrieved 27 January 2019.
- Dipchand, Anne I. (2018-01-02). "Current state of pediatric cardiac transplantation". Annals of Cardiothoracic Surgery. 7 (1): 31–55–55. doi:10.3978/16443 (inactive 2019-10-29). ISSN 2225-319X.
- Eisen, Howard J. (2016). "19. Complications after cardiac transplantation". In Domanski, Michael J.; Mehra, Mandeep R.; Pfeffer, Marc A. (eds.). Oxford Textbook of Advanced Heart Failure and Cardiac Transplantation. Oxford University Press. p. 323. ISBN 9780198734871.
- Blausen.com staff; staff, Blausen com (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine. 1 (2): 10. doi:10.15347/wjm/2014.010. ISSN 2002-4436.
- Mehra, Mandeep R.; Crespo-Leiro, Maria G.; Dipchand, Anne; Ensminger, Stephan M.; Hiemann, Nicola E.; Kobashigawa, Jon A.; Madsen, Joren; Parameshwar, Jayan; Starling, Randall C. (July 2010). Patricia A. Uber. "International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy—2010". The Journal of Heart and Lung Transplantation. 29 (7): 717–27. doi:10.1016/j.healun.2010.05.017. PMID 20620917. Retrieved 27 January 2019.
- Nascimento, Bruno Ramos; Gomes, Thalles Oliveira; Borges, Júlio César; Athayde, Guilherme Rafael Sant'Anna; de Andrade, Sílvio Amadeu; Moreira, Maria da Consolação Vieira (2013). "Primary Angioplasty for Cardiac Allograft Vasculopathy Presenting as ST-Elevation Acute Myocardial Infarction during Endomyocardial Biopsy". Case Reports in Transplantation. 2013: 606481. doi:10.1155/2013/606481. ISSN 2090-6943. PMC 3771468. PMID 24066253.
- Hunt, Sharon A. (2017-11-27). "Cardiac Allograft Vasculopathy: It Really Has Changed Over Time". JACC: Heart Failure. 5 (12): 902–903. doi:10.1016/j.jchf.2017.09.013. ISSN 2213-1779. PMID 29191296.
- Mehra, M. R. (2006). "Contemporary Concepts in Prevention and Treatment of Cardiac Allograft Vasculopathy". American Journal of Transplantation. 6 (6): 1248–1256. doi:10.1111/j.1600-6143.2006.01314.x. ISSN 1600-6143. PMID 16686747.