Candida dubliniensis
Candida dubliniensis is a fungal opportunistic pathogen originally isolated from AIDS patients. It is also occasionally isolated from immunocompetent individuals. It is a dimorphic yeast of the genus Candida, very closely related to Candida albicans but forming a distinct phylogenetic cluster in DNA fingerprinting. It is most commonly isolated from oral cavities,[1] and is also occasionally found in other anatomical sites.
| Candida dubliniensis | |
|---|---|
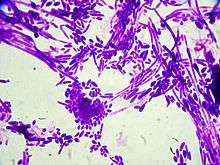 | |
| Gram stain of Candida dubliniensis cells (1000-fold magnification) | |
| Scientific classification | |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Debaryomycetaceae |
| Genus: | Candida |
| Species: | C. dubliniensis |
| Binomial name | |
| Candida dubliniensis Sullivan et al. (1995) | |
Prevalence and epidemiology
Candida dubliniensis is cosmopolitan (found around the world), and has been described as a separate species in 1995.[2] Retrospective studies have shown that previously it had been commonly identified as Candida albicans, with which C. dubliniensis is closely related and shares a number of characteristics.
One test for distinguishing C. dubliniensis from C. albicans, is laboratory culture of the organism at 42 °C. Most C. albicans strains grow at this temperature,[3] whereas most C. dubliniensis isolates do not.[2] There are also significant differences in the conditions that lead to the formation of chlamydospores between C. albicans and C. dubliniensis, although they are otherwise phenotypically very similar.[2]
A European study of 2,589 isolates, that had originally been identified as C. albicans, revealed that 52 of them (2.0%) were C. dubliniensis. Most of these isolates were from oral or faecal specimens from HIV-positive patients, though one vaginal and two oral isolates were from healthy individuals. Another study in the United States surveyed 1,251 yeasts previously identified as C. albicans, and identified 15 isolates (1.2%) as C. dubliniensis. Most of these isolates were from immunocompromised individuals, such as AIDS, chemotherapy, or organ transplant patients. The majority of C. dubliniensis strains were recovered from respiratory, urine and stool specimens. The Memorial Sloan-Kettering Cancer Center also conducted several studies, both retrospective and prospective. In 974 germ-tube positive yeasts, 22 isolates (2.3%) from 16 patients were C. dubliniesis. All individuals were immunologically compromised with either malignancy or AIDS, and the isolates came from a variety of different sites. C. dubliniensis was also isolated from the mouths of 18% of patients with diabetes and who use insulin.[4]
Antifungal susceptibility
In one study, all 20 C. dubliniensis isolates tested were susceptible to itraconazole, ketoconazole and amphotericin B.[5]
Fluconazole
Many isolates of C. dubliniensis are sensitive to fluconazole. In one study, 16 of 20 isolates were sensitive to fluconazole, while four were resistant.[5] It has been hypothesized that C. dubliniensis has the ability to rapidly develop resistance to fluconazole, especially in patients who are on long-term therapy.[5]
Stable fluconazole resistance could be induced in vitro by subjecting sensitive strains to increasing concentrations of this antifungal. This resistance is mediated by a multidrug transporter that can be mobilized rapidly in vitro, on exposure to fluconazole.
Cases in America have also shown the emergence of fluconazole-resistant C. dubliniensis. Three isolates were discovered in Texas, two of which were resistant (MIC, 64 µg/mL), and one had dose-dependent susceptibility (MIC, 16 µg/mL). Among C. dubliniensis isolates in HIV+ patients in Maryland, most isolates were highly susceptible to fluconazole. A study of 71 isolates in Ireland, showed that both the fluconazole-resistant and susceptible strains were susceptible to itraconazole, amphotericin B, and 5-fluorocytosine (microdilution). They were also susceptible to experimental triazoles and voriconazole and echinocandin.
References
- Gilfillan, G. D.; Sullivan, D. J.; Haynes, K.; Parkinson, T.; Coleman, D. C.; Gow, N. A. R (1998). "Candida dubliniensis: phylogeny and putative virulence factors". Microbiology. 144 (4): 829–838. doi:10.1099/00221287-144-4-829. PMID 9579058.
- Sullivan DJ, Westerneng TJ, Haynes KA, Bennett DE, Coleman DC (1995). "Candida dubliniensis sp. nov.: phenotypic and molecular characterization of a novel species associated with oral candidosis in HIV-infected individuals". Microbiology. 141 (7): 1507–21. doi:10.1099/13500872-141-7-1507. PMID 7551019.
- Kamiyama A; Niimi M; Tokunaga M; . Nakayama H (1989). "Adansonian study of Candida albicans: intraspecific homogeneity excepting C. stellatoidea strains". J Med Vet Mycol. 27 (4): 229–241. doi:10.1080/02681218980000311. PMID 2677300.
- Willis AM, Coulter WA, Sullivan DJ, Coleman DC, Hayes JR, Bell PM, Lamey PJ (2000). "Isolation of C. dubliniensis from insulin-using diabetes mellitus patients". J Oral Pathol Med. 29 (2): 86–90. doi:10.1034/j.1600-0714.2000.290206.x. PMID 10718404.
- Moran GP, Sullivan DJ, Henman MC, McCreary CE, Harrington BJ, Shanley DB, Coleman DC (March 1997). "Antifungal drug susceptibilities of oral Candida dubliniensis isolates from human immunodeficiency virus (HIV)-infected and non-HIV-infected subjects and generation of stable fluconazole-resistant derivatives in vitro". Antimicrob. Agents Chemother. 41 (3): 617–23. doi:10.1128/AAC.41.3.617. PMC 163761. PMID 9056003.