Bulimia nervosa
Bulimia nervosa, also known as simply bulimia, is an eating disorder characterized by binge eating followed by purging.[2] Binge eating refers to eating a large amount of food in a short amount of time.[2] Purging refers to the attempts to get rid of the food consumed.[2] This may be done by vomiting or taking laxatives.[2] Other efforts to lose weight may include the use of diuretics, stimulants, water fasting, or excessive exercise.[2][4] Most people with bulimia are at a normal weight.[1] The forcing of vomiting may result in thickened skin on the knuckles and breakdown of the teeth.[2] Bulimia is frequently associated with other mental disorders such as depression, anxiety, and problems with drugs or alcohol.[2] There is also a higher risk of suicide and self-harm.[3]
| Bulimia nervosa | |
|---|---|
| Other names | Bulimia |
| Loss of enamel (acid erosion) from the inside of the upper front teeth as a result of bulimia | |
| Specialty | Psychiatry, clinical psychology |
| Symptoms | Eating a large amount of food in a short amount of time followed by vomiting or the use of laxatives, often normal weight[1][2] |
| Complications | Breakdown of the teeth, depression, anxiety, substance abuse, suicide[2][3] |
| Causes | Genetic and environmental factors[2][4] |
| Diagnostic method | Based on person's medical history[5] |
| Differential diagnosis | Anorexia, binge eating disorder, Kleine-Levin syndrome, borderline personality disorder[5] |
| Treatment | Cognitive behavioral therapy[2][6] |
| Medication | Selective serotonin reuptake inhibitors, tricyclic antidepressant[4][7] |
| Prognosis | Half recover over 10 years with treatment[4] |
| Frequency | 3.6 million (2015)[8] |
Bulimia is more common among those who have a close relative with the condition.[2] The percentage risk that is estimated to be due to genetics is between 30% and 80%.[4] Other risk factors for the disease include psychological stress, cultural pressure to attain a certain body type, poor self-esteem, and obesity.[2][4] Living in a culture that promotes dieting and having parents that worry about weight are also risks.[4] Diagnosis is based on a person's medical history;[5] however, this is difficult, as people are usually secretive about their binge eating and purging habits.[4] Further, the diagnosis of anorexia nervosa takes precedence over that of bulimia.[4] Other similar disorders include binge eating disorder, Kleine-Levin syndrome, and borderline personality disorder.[5]
Cognitive behavioral therapy is the primary treatment for bulimia.[2][6] Antidepressants of the selective serotonin reuptake inhibitor (SSRI) or tricyclic antidepressant classes may have a modest benefit.[4][7] While outcomes with bulimia are typically better than in those with anorexia, the risk of death among those affected is higher than that of the general population.[3] At 10 years after receiving treatment about 50% of people are fully recovered.[4]
Globally, bulimia was estimated to affect 3.6 million people in 2015.[8] About 1% of young women have bulimia at a given point in time and about 2% to 3% of women have the condition at some point in their lives.[3] The condition is less common in the developing world.[4] Bulimia is about nine times more likely to occur in women than men.[5] Among women, rates are highest in young adults.[5] Bulimia was named and first described by the British psychiatrist Gerald Russell in 1979.[9][10]
Signs and symptoms
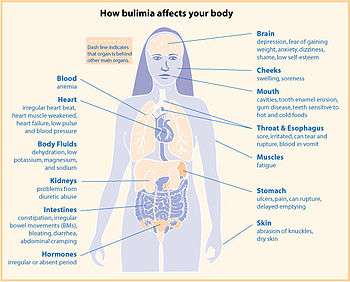

Bulimia typically involves rapid and out-of-control eating, which may stop when the person is interrupted by another person or the stomach hurts from over-extension, followed by self-induced vomiting or other forms of purging. This cycle may be repeated several times a week or, in more serious cases, several times a day[12] and may directly cause:
- Chronic gastric reflux after eating, secondary to vomiting[13]
- Dehydration and hypokalemia due to renal potassium loss in the presence of alkalosis and frequent vomiting[14]
- Electrolyte imbalance, which can lead to abnormal heart rhythms, cardiac arrest, and even death
- Esophagitis, or inflammation of the esophagus
- Mallory-Weiss tears
- Boerhaave syndrome, a rupture in the esophageal wall due to vomiting
- Oral trauma, in which repetitive insertion of fingers or other objects causes lacerations to the lining of the mouth or throat
- Russell's sign: calluses on knuckles and back of hands due to repeated trauma from incisors[15][16]
- Perimolysis, or severe dental erosion of tooth enamel[17]
- Swollen salivary glands (for example, in the neck, under the jaw line)[17][18]
- Gastroparesis, or delayed gastric emptying
- Constipation or diarrhea
- Tachycardia or palpitations
- Hypotension
- Peptic ulcers
- Infertility
- Constant weight fluctuations are common
- Elevated blood sugar, cholesterol, and amylase levels may occur
- Hypoglycemia may occur after vomiting
These are some of the many signs that may indicate whether someone has bulimia nervosa:[19]
- A fixation on the number of calories consumed
- A fixation on and extreme consciousness of one's weight
- Low self-esteem and/or self-harming
- Suicidal tendencies
- An irregular menstrual cycle in women
- Regular trips to the bathroom, especially soon after eating
- Depression, anxiety disorders and sleep disorders
- Frequent occurrences involving consumption of abnormally large portions of food[20]
- The use of laxatives, diuretics, and diet pills
- Compulsive or excessive exercise
- Unhealthy/dry skin, hair, nails and lips
- Fatigue, or exhaustion
As with many psychiatric illnesses, delusions can occur, in conjunction with other signs and symptoms, leaving the person with a false belief that is not ordinarily accepted by others.[21]
People with bulimia nervosa may also exercise to a point that excludes other activities.[21]
Interoceptive
With regards to interoception, people with bulimia report reduced sensitivity to many kinds of internal and external sensations. For example, some show increased thresholds to heat pain compared and report the same level of satiety after consuming more calories than do healthy subjects.[22]
Related disorders
People with bulimia are more likely than people without bulimia to have an affective disorder, such as depression or general anxiety disorder. One study found 70% had depression at some time in their lives (as opposed to 26% for adult females in the general population), rising to 88% for all affective disorders combined.[23] Another study by the Royal Children's Hospital in Melbourne on a cohort of 2,000 adolescents similarly found that those meeting at least two of the DSM-IV criteria for bulimia nervosa or anorexia nervosa had a sixfold increase in risk of anxiety and a doubled risk for substance dependency.[24] Some with anorexia nervosa exhibit episodes of bulimic tendencies through purging (either through self-induced vomiting or laxatives) as a way to quickly remove food in their system.[25] There may be an increased risk for diabetes mellitus type 2.[26] Bulimia also has negative effects on a person's teeth due to the acid passed through the mouth from frequent vomiting causing acid erosion, mainly on the posterior dental surface.
Causes
Biological
As with anorexia nervosa, there is evidence of genetic predispositions contributing to the onset of this eating disorder.[27] Abnormal levels of many hormones, notably serotonin, have been shown to be responsible for some disordered eating behaviors. Brain-derived neurotrophic factor (BDNF) is under investigation as a possible mechanism.[28][29]
There is evidence that sex hormones may influence appetite and eating in women, and the onset of bulimia nervosa. Studies have shown that women with hyperandrogenism and polycystic ovary syndrome have a dysregulation of appetite, along with carbohydrates and fats. This dysregulation of appetite is also seen in women with bulimia nervosa. In addition, gene knockout studies in mice have shown that mice that have the gene encoding estrogen receptors have decreased fertility due to ovarian dysfunction and dysregulation of androgen receptors. In humans, there is evidence that there is an association between polymorphisms in the ERβ (estrogen receptor β) and bulimia, suggesting there is a correlation between sex hormones and bulimia nervosa.[30]
Bulimia has been compared to drug addiction, though the empirical support for this characterization is limited.[31] However, people with bulimia nervosa may share dopamine D2 receptor-related vulnerabilities with those with substance abuse disorders.[32]
Dieting, a common behaviour in bulimics, is associated with lower plasma tryptophan levels.[33] Decreased tryptophan levels in the brain, and thus the synthesis of serotonin, increases bulimic urges in currently and formerly bulimic individuals within hours.[34][35]
Abnormal blood levels of peptides important for the regulation of appetite and energy balance are observed in individuals with bulimia nervosa, but it remains unknown if this is a state or trait.[36]
Social
Media portrayals of an 'ideal' body shape are widely considered to be a contributing factor to bulimia.[21] In a 1991 study by Weltzin, Hsu, Pollicle, and Kaye, it was stated that 19% of bulimics undereat, 37% of bulimics eat an average or normal amount of food, and 44% of bulimics overeat.[37] A survey of 15- to 18-year-old high school girls in Nadroga, Fiji, found the self-reported incidence of purging rose from 0% in 1995 (a few weeks after the introduction of television in the province) to 11.3% in 1998.[38] In addition, the suicide rate among people with bulimia nervosa is 7.5 times higher than in the general population.[39]
When attempting to decipher the origin of bulimia nervosa in a cognitive context, Christopher Fairburn et al.'s cognitive behavioral model is often considered the golden standard. Fairburn et al.'s model discusses the process in which an individual falls into the binge-purge cycle and thus develops bulimia. Fairburn et al. argue that extreme concern with weight and shape coupled with low self-esteem will result in strict, rigid, and inflexible dietary rules. Accordingly, this would lead to unrealistically restricted eating, which may consequently induce an eventual "slip" where the individual commits a minor infraction of the strict and inflexible dietary rules. Moreover, the cognitive distortion due to dichotomous thinking leads the individual to binge. The binge subsequently should trigger a perceived loss of control, promoting the individual to purge in hope of counteracting the binge. However, Fairburn et al. assert the cycle repeats itself, and thus consider the binge-purge cycle to be self-perpetuating.[40]
In contrast, Byrne and Mclean's findings differed slightly from Fairburn et al.'s cognitive behavioral model of bulimia nervosa in that the drive for thinness was the major cause of purging as a way of controlling weight. In turn, Byrne and Mclean argued that this makes the individual vulnerable to binging, indicating that it is not a binge-purge cycle but rather a purge-binge cycle in that purging comes before bingeing. Similarly, Fairburn et al.'s cognitive behavioral model of bulimia nervosa is not necessarily applicable to every individual and is certainly reductionist. Everyone differs from another, and taking such a complex behavior like bulimia and applying the same one theory to everyone would certainly be invalid. In addition, the cognitive behavioral model of bulimia nervosa is very cultural bound in that it may not be necessarily applicable to cultures outside of the Western society. To evaluate, Fairburn et al..'s model and more generally the cognitive explanation of bulimia nervosa is more descriptive than explanatory, as it does not necessarily explain how bulimia arises. Furthermore, it is difficult to ascertain cause and effect, because it may be that distorted eating leads to distorted cognition rather than vice versa.[41][42]
A considerable amount of literature has identified a correlation between sexual abuse and the development of bulimia nervosa. The reported incident rate of unwanted sexual contact is higher among those with bulimia nervosa than anorexia nervosa.[43]
When exploring the etiology of bulimia through a socio-cultural perspective, the "thin ideal internalization" is significantly responsible. The thin ideal internalization is the extent to which individuals adapt to the societal ideals of attractiveness. Studies have shown that young females that read fashion magazines tend to have more bulimic symptoms than those females who do not. This further demonstrates the impact of media on the likelihood of developing the disorder.[44] Individuals first accept and "buy into" the ideals, and then attempt to transform themselves in order to reflect the societal ideals of attractiveness. J. Kevin Thompson and Eric Stice claim that family, peers, and most evidently media reinforce the thin ideal, which may lead to an individual accepting and "buying into" the thin ideal. In turn, Thompson and Stice assert that if the thin ideal is accepted, one could begin to feel uncomfortable with their body shape or size since it may not necessarily reflect the thin ideal set out by society. Thus, people feeling uncomfortable with their bodies may result in suffering from body dissatisfaction and may develop a certain drive for thinness. Consequently, body dissatisfaction coupled with a drive for thinness is thought to promote dieting and negative effects, which could eventually lead to bulimic symptoms such as purging or bingeing. Binges lead to self-disgust which causes purging to prevent weight gain.[45]
A study dedicated to investigating the thin ideal internalization as a factor of bulimia nervosa is Thompson's and Stice's research. The aim of their study was to investigate how and to what degree media affects the thin ideal internalization. Thompson and Stice used randomized experiments (more specifically programs) dedicated to teaching young women how to be more critical when it comes to media, in order to reduce thin ideal internalization. The results showed that by creating more awareness of the media's control of the societal ideal of attractiveness, the thin ideal internalization significantly dropped. In other words, less thin ideal images portrayed by the media resulted in less thin ideal internalization. Therefore, Thompson and Stice concluded that media greatly affected the thin ideal internalization.[46] Papies showed that it is not the thin ideal itself, but rather the self-association with other persons of a certain weight that decide how someone with bulimia nervosa feels. People that associate themselves with thin models get in a positive attitude when they see thin models and people that associate with overweight get in a negative attitude when they see thin models. Moreover, it can be taught to associate with thinner people.[47]
Diagnosis
The onset of bulimia nervosa is often during adolescence, between 13 and 20 years of age, and many cases have previously suffered from obesity, with many sufferers relapsing in adulthood into episodic bingeing and purging even after initially successful treatment and remission.[48] A lifetime prevalence of 0.5 percent and 0.9 percent for adult and adolescent sufferers, respectively, is estimated among the United States population.[49] Bulimia nervosa may affect up to 1% of young women and, after 10 years of diagnosis, half will recover fully, a third will recover partially, and 10–20% will still have symptoms.[4]
Adolescents with bulimia nervosa are more likely to have self-imposed perfectionism and compulsivity issues in eating compared to their peers. This means that the high expectations and unrealistic goals that these individuals set for themselves are internally motivated rather than by social views or expectations.[50]
Criteria
Bulimia nervosa can be difficult to detect, compared to anorexia nervosa, because bulimics tend to be of average or slightly above or below average weight. Many bulimics may also engage in significantly disordered eating and exercise patterns without meeting the full diagnostic criteria for bulimia nervosa.[51] Recently, the Diagnostic and Statistical Manual of Mental Disorders was revised, which resulted in the loosening of criteria regarding the diagnoses of bulimia nervosa and anorexia nervosa.[52] The diagnostic criteria utilized by the DSM-5 includes repetitive episodes of binge eating (a discrete episode of overeating during which the individual feels out of control of consumption) compensated for by excessive or inappropriate measures taken to avoid gaining weight.[53] The diagnosis also requires the episodes of compensatory behaviors and binge eating to happen a minimum of once a week for a consistent time period of 3 months.[54] The diagnosis is made only when the behavior is not a part of the symptom complex of anorexia nervosa and when the behavior reflects an overemphasis on physical mass or appearance. Purging often is a common characteristic of a more severe case of bulimia nervosa.[55]
Treatment
There are two main types of treatment given to those suffering with bulimia nervosa; psychopharmacological and psychosocial treatments.[56]
Psychotherapy
There are several supported psychosocial treatments for bulimia. Cognitive behavioral therapy (CBT), which involves teaching a person to challenge automatic thoughts and engage in behavioral experiments (for example, in session eating of "forbidden foods") has a small amount of evidence supporting its use.[57]
By using CBT people record how much food they eat and periods of vomiting with the purpose of identifying and avoiding emotional fluctuations that bring on episodes of bulimia on a regular basis.[58] Barker (2003) states that research has found 40–60% of people using cognitive behaviour therapy to become symptom free. He states in order for the therapy to work, all parties must work together to discuss, record and develop coping strategies. Barker (2003) claims by making people aware of their actions they will think of alternatives.[59][60] People undergoing CBT who exhibit early behavioral changes are most likely to achieve the best treatment outcomes in the long run.[61] Researchers have also reported some positive outcomes for interpersonal psychotherapy and dialectical behavior therapy.[62][63]
Maudsley family therapy, developed at the Maudsley Hospital in London for the treatment of anorexia has been shown promising results in bulimia.[64]
The use of Cognitive Behavioral Therapy (CBT) has been shown to be quite effective for treating bulimia nervosa (BN) in adults, but little research has been done on effective treatments of BN for adolescents.[65] Although CBT is seen as more cost efficient and helps individuals with BN in self-guided care, Family Based Treatment (FBT) might be more helpful to younger adolescents who need more support and guidance from their families. Adolescents are at the stage where their brains are still quite malleable and developing gradually.[66] Therefore, young adolescents with BN are less likely to realize the detrimental consequences of becoming bulimic and have less motivation to change,[67] which is why FBT would be useful to have families intervene and support the teens.[65] Working with BN patients and their families in FBT can empower the families by having them involved in their adolescent's food choices and behaviors, taking more control of the situation in the beginning and gradually letting the adolescent become more autonomous when they have learned healthier eating habits.[65]
Medication
Antidepressants of the selective serotonin reuptake inhibitors (SSRI) class may have a modest benefit.[7] This includes fluoxetine, which is FDA approved, for the treatment of bulimia, other antidepressants such as sertraline may also be effective against bulimia. Topiramate may also be useful but has greater side effects.[7]
It is not known if combining medication with counseling improves the outcomes. Any trials which originally suggested that such combinations should improve the outcome have not proven to be exceptionally powerful. Some positive outcomes of treatments can include: abstinence from binge eating, a decrease in obsessive behaviors to lose weight and in shape preoccupation, less severe psychiatric symptoms, a desire to counter the effects of binge eating, as well as an improvement in social functioning and reduced relapse rates.[4]
Alternative medicine
Some researchers have also claimed positive outcomes in hypnotherapy.[68]
Epidemiology
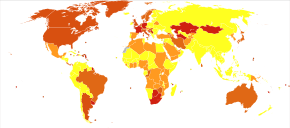
There is little data on the percentage of people with bulimia in general populations. Most studies conducted thus far have been on convenience samples from hospital patients, high school or university students. These have yielded a wide range of results: between 0.1% and 1.4% of males, and between 0.3% and 9.4% of females.[69] Studies on time trends in the prevalence of bulimia nervosa have also yielded inconsistent results.[70] According to Gelder, Mayou and Geddes (2005) bulimia nervosa is prevalent between 1 and 2 percent of women aged 15–40 years. Bulimia nervosa occurs more frequently in developed countries[58] and in cities, with one study finding that bulimia is five times more prevalent in cities than in rural areas.[71] There is a perception that bulimia is most prevalent amongst girls from middle-class families;[72] however, in a 2009 study girls from families in the lowest income bracket studied were 153 percent more likely to be bulimic than girls from the highest income bracket.[73]
There are higher rates of eating disorders in groups involved in activities which idealize a slim physique, such as dance,[74] gymnastics, modeling, cheerleading, running, acting, swimming, diving, rowing and figure skating. Bulimia is thought to be more prevalent among Caucasians;[75] however, a more recent study showed that African-American teenage girls were 50 percent more likely than Caucasian girls to exhibit bulimic behavior, including both binging and purging.[76]
| Country | Year | Sample size and type | % affected | |
|---|---|---|---|---|
| Australia | 2008 | 1,943 adolescents (ages 15–17) | 1.0% male | 6.4% female[24] |
| Portugal | 2006 | 2,028 high school students | 0.3% female[77] | |
| Brazil | 2004 | 1,807 students (ages 7–19) | 0.8% male | 1.3% female[78] |
| Spain | 2004 | 2,509 female adolescents (ages 13–22) | 1.4% female[79] | |
| Hungary | 2003 | 580 Budapest residents | 0.4% male | 3.6% female[74] |
| Australia | 1998 | 4,200 high school students | 0.3% combined[80] | |
| United States | 1996 | 1,152 college students | 0.2% male | 1.3% female[81] |
| Norway | 1995 | 19,067 psychiatric patients | 0.7% male | 7.3% female[82] |
| Canada | 1995 | 8,116 (random sample) | 0.1% male | 1.1% female[83] |
| Japan | 1995 | 2,597 high school students | 0.7% male | 1.9% female[84] |
| United States | 1992 | 799 college students | 0.4% male | 5.1% female[85] |
History
Etymology
The term bulimia comes from Greek βουλιμία boulīmia, "ravenous hunger", a compound of βοῦς bous, "ox" and λιμός, līmos, "hunger".[86] Literally, the scientific name of the disorder, bulimia nervosa, translates to "nervous ravenous hunger".
Before the 20th century
Although diagnostic criteria for bulimia nervosa did not appear until 1979, evidence suggests that binging and purging were popular in certain ancient cultures. The first documented account of behavior resembling bulimia nervosa was recorded in Xenophon's Anabasis around 370 B.C, in which Greek soldiers purged themselves in the mountains of Asia Minor. It is unclear whether this purging was preceded by binging.[87] In ancient Egypt, physicians recommended purging once a month for three days in order to preserve health.[88] This practice stemmed from the belief that human diseases were caused by the food itself. In ancient Rome, elite society members would vomit in order to "make room" in their stomachs for more food at all day banquets.[88] Emperors Claudius and Vitellius both were gluttonous and obese, and they often resorted to habitual purging.[88]
Historical records also suggest that some saints who developed anorexia (as a result of a life of asceticism) may also have displayed bulimic behaviors.[88] Saint Mary Magdalen de Pazzi (1566–1607) and Saint Veronica Giuliani (1660–1727) were both observed binge eating—giving in, as they believed, to the temptations of the devil.[88] Saint Catherine of Siena (1347–1380) is known to have supplemented her strict abstinence from food by purging as reparation for her sins. Catherine died from starvation at age thirty-three.[88]
While the psychological disorder "bulimia nervosa" is relatively new, the word "bulimia," signifying overeating, has been present for centuries.[88] The Babylon Talmud referenced practices of "bulimia," yet scholars believe that this simply referred to overeating without the purging or the psychological implications bulimia nervosa.[88] In fact, a search for evidence of bulimia nervosa from the 17th to late 19th century revealed that only a quarter of the overeating cases they examined actually vomited after the binges. There was no evidence of deliberate vomiting or an attempt to control weight.[88]
20th century
At the turn of the century, bulimia (overeating) was described as a clinical symptom, but rarely in the context of weight control.[89] Purging, however, was seen in anorexic patients and attributed to gastric pain rather than another method of weight control.[89]
In 1930, admissions of anorexia nervosa patients to the Mayo Clinic from 1917 to 1929 were compiled. Fifty-five to sixty-five percent of these patients were reported to be voluntarily vomiting in order to relieve weight anxiety.[89] Records show that purging for weight control continued throughout the mid-1900s. Several case studies from this era reveal patients suffering from the modern description of bulimia nervosa.[89] In 1939, Rahman and Richardson reported that out of their six anorexic patients, one had periods of overeating and another practiced self-induced vomiting.[89] Wulff, in 1932, treated "Patient D," who would have periods of intense cravings for food and overeat for weeks, which often resulted in frequent vomiting.[88] Patient D, who grew up with a tyrannical father, was repulsed by her weight and would fast for a few days, rapidly losing weight. Ellen West, a patient described by Ludwig Binswanger in 1958, was teased by friends for being fat and excessively took thyroid pills to lose weight, later using laxatives and vomiting.[88] She reportedly consumed dozens of oranges and several pounds of tomatoes each day, yet would skip meals. After being admitted to a psychiatric facility for depression, Ellen ate ravenously yet lost weight, presumably due to self-induced vomiting.[88] However, while these patients may have met modern criteria for bulimia nervosa, they cannot technically be diagnosed with the disorder, as it had not yet appeared in the Diagnostic and Statistical Manual of Mental Disorders at the time of their treatment.[88]
An explanation for the increased instances of bulimic symptoms may be due to the 20th century's new ideals of thinness.[89] The shame of being fat emerged in the 1940s, when teasing remarks about weight became more common. The 1950s, however, truly introduced the trend of an aspiration for thinness.[89]
In 1979, Gerald Russell first published a description of bulimia nervosa, in which he studied patients with a "morbid fear of becoming fat" who overate and purged afterwards.[9] He specified treatment options and indicated the seriousness of the disease, which can be accompanied by depression and suicide.[9] In 1980, bulimia nervosa first appeared in the DSM-III.[9]
After its appearance in the DSM-III, there was a sudden rise in the documented incidences of bulimia nervosa.[88] In the early 1980s, incidences of the disorder rose to about 40 in every 100,000 people.[88] This decreased to about 27 in every 100,000 people at the end of the 1980s/early 1990s.[88] However, bulimia nervosa's prevalence was still much higher than anorexia nervosa's, which at the time occurred in about 14 people per 100,000.[88]
In 1991, Kendler et al. documented the cumulative risk for bulimia nervosa for those born before 1950, from 1950 to 1959, and after 1959.[90] The risk for those born after 1959 is much higher than those in either of the other cohorts.[90]
See also
- Anorectic Behavior Observation Scale
- Eating disorders and development
- Eating recovery
- Binge eating disorder
- List of people with bulimia nervosa
References
- Bulik, CM; Marcus, MD; Zerwas, S; Levine, MD; La Via, M (October 2012). "The changing "weightscape" of bulimia nervosa". The American Journal of Psychiatry. 169 (10): 1031–6. doi:10.1176/appi.ajp.2012.12010147. PMC 4038540. PMID 23032383.
- "Bulimia nervosa fact sheet". Office on Women's Health. July 16, 2012. Archived from the original on 19 June 2015. Retrieved 27 June 2015.
- Smink, FR; van Hoeken, D; Hoek, HW (August 2012). "Epidemiology of eating disorders: incidence, prevalence and mortality rates". Current Psychiatry Reports. 14 (4): 406–14. doi:10.1007/s11920-012-0282-y. PMC 3409365. PMID 22644309.
- Hay PJ, Claudino AM; Claudino (2010). "Bulimia nervosa". Clinical Evidence. 2010: 1009. PMC 3275326. PMID 21418667.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (Fifth ed.). Arlington, VA: American Psychiatric Publishing. pp. 345–349. ISBN 978-0-89042-555-8.
- Hay, P (July 2013). "A systematic review of evidence for psychological treatments in eating disorders: 2005–2012". The International Journal of Eating Disorders. 46 (5): 462–9. doi:10.1002/eat.22103. PMID 23658093.
- McElroy, SL; Guerdjikova, AI; Mori, N; O'Melia, AM (October 2012). "Current pharmacotherapy options for bulimia nervosa and binge eating disorder". Expert Opinion on Pharmacotherapy. 13 (14): 2015–26. doi:10.1517/14656566.2012.721781. PMID 22946772.
- GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Russell G (1979). "Bulimia nervosa: An ominous variant of anorexia nervosa". Psychological Medicine. 9 (3): 429–48. doi:10.1017/S0033291700031974. PMID 482466.
- Palmer R (2004). "Bulimia nervosa: 25 years on". The British Journal of Psychiatry. 185 (6): 447–8. doi:10.1192/bjp.185.6.447. PMID 15572732.
- Dorfman J, The Center for Special Dentistry.
- "Bulimia Nervosa" (PDF). Let's Talk Facts: 1. 2005. Retrieved 13 September 2013.
- Mehler PS (2003). "Bulimia Nervosa". The New England Journal of Medicine. 349 (9): 875–81. doi:10.1056/NEJMcp022813. PMID 12944574.
- Mehler, PS.; Crews, C.; Weiner, K. (2004). "Bulimia: medical complications". J Womens Health (Larchmt). 13 (6): 668–75. doi:10.1089/jwh.2004.13.668. PMID 15333281.
- Joseph AB, Herr B; Herr (1985). "Finger calluses in bulimia". The American Journal of Psychiatry. 142 (5): 655. doi:10.1176/ajp.142.5.655a. PMID 3857013.
- Wynn DR, Martin MJ; Martin (1984). "A physical sign of bulimia". Mayo Clinic Proceedings. 59 (10): 722. doi:10.1016/s0025-6196(12)62063-1. PMID 6592415.
- "Eating Disorders". Oral Health Topics A–Z. American Dental Association. Archived from the original on February 3, 2009.
- Mcgilley BM, Pryor TL; Pryor (June 1998). "Assessment and Treatment of Bulimia Nervosa". American Family Physician. 57 (11): 2743–50. PMID 9636337.
- "Symptoms Of Bulimia Nervosa". Illawarra Mercury. February 23, 2001. Archived from the original on February 21, 2016.
- "Bulimia Nervosa". Proud2BME. The National Eating Disorders Association. Archived from the original on 10 December 2014. Retrieved 5 December 2014.
- Barker, P (2003). Psychiatric and Mental Health Nursing: The Craft of Caring. Great Britain: Arnold. ISBN 978-0340810262.
- Khalsa, Sahib S., and Rachel C. Lapidus. “Can Interoception Improve the Pragmatic Search for Biomarkers in Psychiatry?” Frontiers in Psychiatry 7 (2016): 121. PMC. Web. 15 June 2017.
- Walsh BT, Roose SP, Glassman AH, Gladis M, Sadik C (1985). "Bulimia and depression". Psychosomatic Medicine. 47 (2): 123–31. doi:10.1097/00006842-198503000-00003. PMID 3863157.
- Patton GC, Coffey C, Carlin JB, Sanci L, Sawyer S (2008). "Prognosis of adolescent partial syndromes of eating disorder". The British Journal of Psychiatry. 192 (4): 294–9. doi:10.1192/bjp.bp.106.031112. PMID 18378993.
- Carlson, N.R., et al. (2007). Psychology: The Science of Behaviour – 4th Canadian ed. Toronto, ON: Pearson Education Canada.
- Nieto-Martínez, Ramfis; González-Rivas, Juan P.; Medina-Inojosa, José R.; Florez, Hermes (2017-11-22). "Are Eating Disorders Risk Factors for Type 2 Diabetes? A Systematic Review and Meta-analysis". Current Diabetes Reports. 17 (12): 138. doi:10.1007/s11892-017-0949-1. ISSN 1534-4827. PMID 29168047.
- "Biological Causes of Anorexia Nervosa and Bulimia Nervosa". Archived from the original on 2 May 2016. Retrieved 4 July 2016.
- Ribasés M, Gratacòs M, Fernández-Aranda F, Bellodi L, Boni C, Anderluh M, Cavallini MC, Cellini E, Di Bella D, Erzegovesi S, Foulon C, Gabrovsek M, Gorwood P, Hebebrand J, Hinney A, Holliday J, Hu X, Karwautz A, Kipman A, Komel R, Nacmias B, Remschmidt H, Ricca V, Sorbi S, Wagner G, Treasure J, Collier DA, Estivill X (2004). "Association of BDNF with anorexia, bulimia and age of onset of weight loss in six European populations". Human Molecular Genetics. 13 (12): 1205–1212. doi:10.1093/hmg/ddh137. PMID 15115760.
- Wonderlich, Stephen; Mitchell, James E.; de Zwaan, Martina; Steiger, Howard, eds. (2008). "1". Annual Review of Eating Disorders – part 2. Radcliffe Publishing. pp. 14–15. ISBN 978-1-84619-244-9.
- Hirschberg AL (2012). "Sex hormones, appetite and eating behaviour in women". Maturitas. 71 (3): 248–56. doi:10.1016/j.maturitas.2011.12.016. PMID 22281161.
- Broft A, Shingleton R, Kaufman J, Liu F, Kumar D, Slifstein M, Abi-Dargham A, Schebendach J, Van Heertum R, Attia E, Martinez D, Walsh BT (July 2012). "Striatal dopamine in bulimia nervosa: A pet imaging study". The International Journal of Eating Disorders. 45 (5): 648–656. doi:10.1002/eat.20984. PMC 3640453. PMID 22331810.
- Kaye WH, Wierenga CE, Bailer UF, Simmons AN, Wagner A, Bischoff-Grethe A (2013). "Does a Shared Neurobiology for Foods and Drugs of Abuse Contribute to Extremes of Food Ingestion in Anorexia and Bulimia Nervosa?". Biological Psychiatry. 73 (9): 836–42. doi:10.1016/j.biopsych.2013.01.002. PMC 3755487. PMID 23380716.
- Strasser, Barbara (2016). "Diet Versus Exercise in Weight Loss and Maintenance: Focus on Tryptophan". International Journal of Tryptophan Research. 9: 9–16. doi:10.4137/IJTR.S33385. PMC 4864009. PMID 27199566.
- Smith KA, Fairburn CG, Cowen PJ (1999). "Symptomatic Relapse in Bulimia Nervosa Following Acute Tryptophan Depletion". Archives of General Psychiatry. 56 (2): 171–6. doi:10.1001/archpsyc.56.2.171. PMID 10025442.
- Weltzin TE, Fernstrom MH, Fernstrom JD, Neuberger SK, Kaye WH (1995). "Acute tryptophan depletion and increased food intake and irritability in bulimia nervosa". The American Journal of Psychiatry. 152 (11): 1668–71. doi:10.1176/ajp.152.11.1668. PMID 7485633.
- Tortorella, Alfonso; Brambilla, Francesca; Fabrazzo, Michele; Volpe, Umberto; Monteleone, Alessio Maria; Mastromo, Daniele; Monteleone, Palmiero (2014-06-18). "Central and Peripheral Peptides Regulating Eating Behaviour and Energy Homeostasis in Anorexia Nervosa and Bulimia Nervosa: A Literature Review". European Eating Disorders Review. 22 (5): 307–320. doi:10.1002/erv.2303. ISSN 1072-4133. PMID 24942507.
- Carlson, Neil R.; Buskist, William; Heth, C. Donald; Schmaltz, Rod (2010). Psychology: the science of behaviour (4th Canadian ed.). Toronto: Pearson Education Canada. p. 415. ISBN 978-0-205-70286-2.
- Becker AE, Burwell RA, Gilman SE, Herzog DB, Hamburg P (2002). "Eating behaviours and attitudes following prolonged exposure to television among ethnic Fijian adolescent girls". The British Journal of Psychiatry. 180 (6): 509–14. doi:10.1192/bjp.180.6.509. PMID 12042229.
- Nolen-Hoeksema, Susan (2014). "Bulimia Nervosa" Abnormal Psychology. 6e. pg 344.
- Fairburn, C. G.; Beglin, S. J. (April 1, 1990). "Studies of the epidemiology of bulimia nervosa". American Journal of Psychiatry. 147 (4): 401–408. doi:10.1176/ajp.147.4.401. ISSN 0002-953X. PMID 2180327.
- Trull, Thimothy (2010-10-08). Abnormal Psychology and Life: A Dimensional Approach. Belmont CA: Wadsworth, Cengage Learning. pp. 236–8. ISBN 978-1-111-34376-7. Archived from the original on 2016-02-07.
- Byrne SM, McLean NJ; McLean (2002). "The cognitive-behavioral model of bulimia nervosa: A direct evaluation". The International Journal of Eating Disorders. 31 (1): 17–31. doi:10.1002/eat.10002. PMID 11835294.
- Waller, G (1992). "Sexual abuse and the severity of bulimic symptoms". The British Journal of Psychiatry. 161: 90–3. doi:10.1192/bjp.161.1.90. PMID 1638336.
- Nolen-Hoeksema, Susan (2013). (Ab)normal Psychology. McGraw Hill. p. 338. ISBN 978-0078035388.
- Zieve, David. "Bulimia". PubMed Health. Archived from the original on February 11, 2011. Retrieved April 18, 2011.
- Thompson, J. Kevin; Stice, Eric (2001). "Thin-Ideal Internalization: Mounting Evidence for a New Risk Factor for Body-Image Disturbance and Eating Pathology". Current Directions in Psychological Science. 10 (5): 181–3. doi:10.1111/1467-8721.00144. JSTOR 20182734.
- Papies EK, Nicolaije KA; Nicolaije (2012). "Inspiration or deflation? Feeling similar or dissimilar to slim and plus-size models affects self-evaluation of restrained eaters". Body Image. 9 (1): 76–85. doi:10.1016/j.bodyim.2011.08.004. PMID 21962524.
- Shader, Richard I. (2004). Manual of Psychiatric Therapeutics. Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-4459-1.
- [Nolen-Hoeksema, S. (2013)."(Ab)normal Psychology"(6th edition). McGraw-Hill. p.344]
- Castro-Fornieles J, Gual P, Lahortiga F, Gila A, Casulà V, Fuhrmann C, Imirizaldu M, Saura B, Martínez E, Toro J (September 2007). "Self-oriented perfectionism in eating disorders". The International Journal of Eating Disorders. 40 (6): 562–568. doi:10.1002/eat.20393. PMID 17510925.
- Walsh JM, Wheat ME, Freund K (2000). "Detection, evaluation, and treatment of eating disorders". Journal of General Internal Medicine. 15 (8): 577–90. doi:10.1046/j.1525-1497.2000.02439.x. PMC 1495575. PMID 10940151.
- [Nolen-Hoeksema, S. (2013)."(Ab)normal Psychology"(6th edition). McGraw-Hill. p.343]
- American Psychiatric Association (2000). "Diagnostic criteria for 307.51 Bulimia Nervosa". Diagnostic and Statistical Manual of Mental Disorders (4th, text revision (DSM-IV-TR) ed.). ISBN 978-0-89042-025-6.
- [Nolen-Hoeksema, S. (2013)."(Ab)normal Psychology" (6th edition). McGraw-Hill. p.343]
- Nolan-Hoeksema, Susan (2014). Abnormal Psychology (6 ed.). McGraw-Hill Education. p. 345. ISBN 978-0-07-803538-8.
- Hoste RR, Labuschagne Z, Le Grange D (2012). "Adolescent Bulimia Nervosa". Current Psychiatry Reports. 14 (4): 391–7. doi:10.1007/s11920-012-0280-0. PMID 22614677.
- Hay, PP; Bacaltchuk, J; Stefano, S; Kashyap, P (7 October 2009). "Psychological treatments for bulimia nervosa and binging". The Cochrane Database of Systematic Reviews (4): CD000562. doi:10.1002/14651858.CD000562.pub3. PMID 19821271.
- Gelder, Michael Graham; Mayou, Richard; Geddes, John (2005). Psychiatry. ISBN 978-0-19-852863-0.
- Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC (2000). "Outcome Predictors for the Cognitive Behavior Treatment of Bulimia Nervosa: Data from a Multisite Study". The American Journal of Psychiatry. 157 (8): 1302–8. doi:10.1176/appi.ajp.157.8.1302. PMID 10910795.
- Wilson GT, Loeb KL, Walsh BT, Labouvie E, Petkova E, Liu X, Waternaux C (1999). "Psychological versus pharmacological treatments of bulimia nervosa: Predictors and processes of change". Journal of Consulting and Clinical Psychology. 67 (4): 451–9. CiteSeerX 10.1.1.583.7568. doi:10.1037/0022-006X.67.4.451. PMID 10450615.
- Trunko ME, Rockwell RE, Curry E, Runfola C, Kaye WH (2007). "Management of bulimia nervosa". Women's Health (London, England). 3 (2): 255–65. doi:10.2217/17455057.3.2.255. PMID 19803857.
- Fairburn CG, Agras WS, Walsh BT, Wilson GT, Stice E (2004). "Prediction of Outcome in Bulimia Nervosa by Early Change in Treatment". The American Journal of Psychiatry. 161 (12): 2322–4. doi:10.1176/appi.ajp.161.12.2322. PMID 15569910.
- Safer DL, Telch CF, Agras WS (2001). "Dialectical Behavior Therapy for Bulimia Nervosa". The American Journal of Psychiatry. 158 (4): 632–4. doi:10.1176/appi.ajp.158.4.632. PMID 11282700.
- Lock J, le Grange D; Le Grange (2005). "Family-based treatment of eating disorders". The International Journal of Eating Disorders. 37: S64–7, discussion S87–9. doi:10.1002/eat.20122. PMID 15852323.
- Keel PK, Haedt A; Haedt (2008). "Evidence-Based Psychosocial Treatments for Eating Problems and Eating Disorders". Journal of Clinical Child and Adolescent Psychology. 37 (1): 39–61. doi:10.1080/15374410701817832. PMID 18444053.
- Le Grange D, Lock J, Dymek M (2003). "Family-based therapy for adolescents with bulimia nervosa". American Journal of Psychotherapy. 57 (2): 237–51. doi:10.1176/appi.psychotherapy.2003.57.2.237. PMID 12817553.
- Castro-Fornieles J, Bigorra A, Martinez-Mallen E, Gonzalez L, Moreno E, Font E, Toro J (2011). "Motivation to change in adolescents with bulimia nervosa mediates clinical change after treatment". European Eating Disorders Review. 19 (1): 46–54. doi:10.1002/erv.1045. PMID 20872926.
- Barabasz M (2007). "Efficacy of Hypnotherapy in the Treatment of Eating Disorders". The International Journal of Clinical and Experimental Hypnosis. 55 (3): 318–35. doi:10.1080/00207140701338688. PMID 17558721.
- Makino M, Tsuboi K, Dennerstein L (2004). "Prevalence of eating disorders: a comparison of Western and non-Western countries". MedGenMed : Medscape General Medicine. 6 (3): 49. PMC 1435625. PMID 15520673. Archived from the original on 2013-02-19.
- Hay PJ, Mond J, Buttner P, Darby A (2008). Murthy RS (ed.). "Eating Disorder Behaviors Are Increasing: Findings from Two Sequential Community Surveys in South Australia". PLOS ONE. 3 (2): e1541. doi:10.1371/journal.pone.0001541. PMC 2212110. PMID 18253489.
- van Son GE, van Hoeken D, Bartelds AI, van Furth EF, Hoek HW (2006). "Urbanisation and the incidence of eating disorders". The British Journal of Psychiatry. 189 (6): 562–3. doi:10.1192/bjp.bp.106.021378. PMID 17139044.
- "Bulimia". finddoctorsonline.com. Archived from the original on 2012-07-09.
- Grohol, John (March 19, 2009). "Black Girls At Risk for Bulimia". Archived from the original on May 24, 2012.
- Tölgyes T, Nemessury J; Nemessury (2004). "Epidemiological studies on adverse dieting behaviours and eating disorders among young people in Hungary". Social Psychiatry and Psychiatric Epidemiology. 39 (8): 647–54. doi:10.1007/s00127-004-0783-z. PMID 15300375.
- Franko DL, Becker AE, Thomas JJ, Herzog DB (2007). "Cross-ethnic differences in eating disorder symptoms and related distress". The International Journal of Eating Disorders. 40 (2): 156–64. doi:10.1002/eat.20341. PMID 17080449.
- McBride, Hugh. "Study Reveals Stunning Prevalence of Bulimia Among African-American Girls". Archived from the original on February 10, 2012.
- Machado PP, Machado BC, Gonçalves S, Hoek HW (2007). "The prevalence of eating disorders not otherwise specified". The International Journal of Eating Disorders. 40 (3): 212–7. doi:10.1002/eat.20358. hdl:1822/5722. PMID 17173324.
- Vilela JE, Lamounier JA, Dellaretti Filho MA, Barros Neto JR, Horta GM (2004). "Transtornos alimentares em escolares" [Eating disorders in school children]. Jornal de Pediatria (in Portuguese). 80 (1): 49–54. doi:10.1590/S0021-75572004000100010. PMID 14978549.
- Lahortiga-Ramos F, De Irala-Estévez J, Cano-Prous A, Gual-García P, Martínez-González MA, Cervera-Enguix S (2005). "Incidence of eating disorders in Navarra (Spain)". European Psychiatry. 20 (2): 179–85. doi:10.1016/j.eurpsy.2004.07.008. PMID 15797704.
- Hay P (1998). "The epidemiology of eating disorder behaviors: An Australian community-based survey". The International Journal of Eating Disorders. 23 (4): 371–82. doi:10.1002/(SICI)1098-108X(199805)23:4<371::AID-EAT4>3.0.CO;2-F. PMID 9561427.
- Pemberton AR, Vernon SW, Lee ES (1996). "Prevalence and Correlates of Bulimia Nervosa and Bulimic Behaviors in a Racially Diverse Sample of Undergraduate Students in Two Universities in Southeast Texas". American Journal of Epidemiology. 144 (5): 450–5. doi:10.1093/oxfordjournals.aje.a008950. PMID 8781459.
- Götestam KG, Eriksen L, Hagen H (1995). "An epidemiological study of eating disorders in Norwegian psychiatric institutions". The International Journal of Eating Disorders. 18 (3): 263–8. doi:10.1002/1098-108X(199511)18:3<263::AID-EAT2260180308>3.0.CO;2-O. PMID 8556022.
- Garfinkel PE, Lin E, Goering P, Spegg C, Goldbloom DS, Kennedy S, Kaplan AS, Woodside DB (July 1995). "Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups". The American Journal of Psychiatry. 152 (7): 1052–8. doi:10.1176/ajp.152.7.1052. PMID 7793442.
- Suzuki K, Takeda A, Matsushita S (1995). "Coprevalence of bulimia with alcohol abuse and smoking among Japanese male and female high school students". Addiction. 90 (7): 971–5. doi:10.1111/j.1360-0443.1995.tb03506.x. PMID 7663319.
- Heatherton TF, Nichols P, Mahamedi F, Keel P (November 1995). "Body weight, dieting, and eating disorder symptoms among college students, 1982 to 1992". The American Journal of Psychiatry. 152 (11): 1623–9. doi:10.1176/ajp.152.11.1623. PMID 7485625.
- Douglas Harper (November 2001). "Online Etymology Dictionary: bulimia". Online Etymology Dictionary. Archived from the original on 2008-06-17. Retrieved 2008-04-06.
- Giannini, A. J. (1993). "A history of bulimia". In The Eating disorders (pp. 18–21). Springer New York.
- Russell, G. (1997). The history of bulimia nervosa. D. Garner & P. Garfinkel (Eds.), Handbook of Treatment for Eating Disorders (2nd ed., pp. 11–24). New York, NY: The Guilford Press.
- Casper, Regina C. (1983). "On the emergence of bulimia nervosa as a syndrome a historical view". International Journal of Eating Disorders. 2 (3): 3–16. doi:10.1002/1098-108X(198321)2:3<3::AID-EAT2260020302>3.0.CO;2-D.
- Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L (1991). "The genetic epidemiology of bulimia nervosa". The American Journal of Psychiatry. 148 (12): 1627–37. doi:10.1176/ajp.148.12.1627. PMID 1842216.
External links
| Wikimedia Commons has media related to Bulimia nervosa. |
| Wikiquote has quotations related to: Bulimia nervosa |
| Classification | |
|---|---|
| External resources |