Accessory pathway
An accessory pathway is an additional electrical connection between two parts of the heart.[1] These pathways can lead to abnormal heart rhythms or arrhythmias associated with symptoms of palpitations. Some pathways may activate a region of ventricular muscle earlier than would normally occur, referred to as pre-excitation, which may be seen on an electrocardiogram. Accessory pathways causing pre-excitation and arrhythmias can be said to be causing Wolff-Parkinson-White syndrome.[2]
Accessory pathways are often diagnosed using an electrocardiogram, but characterisation and location of the pathway may require an electrophysiological study. Accessory pathways may not require any treatment, but those causing symptoms may be treated with medication including calcium channel antagonists, beta blockers or flecainide.[3] Alternatively, the electrical conduction through an accessory pathways can be abolished using catheter ablation, potentially offering a permanent cure.[3]
Mahaim pathways
The commonest sites for accessory pathways are connections between muscle tissue in the atria and the ventricles (atrio-ventricular pathways), bypassing the atrioventricular node. Rarer sites include connections between atrial muscle and the conducting tissue within the ventricles (atrio-fascicular pathways), between the atrioventricular node and the muscle tissue of the ventricle (nodo-ventricular pathways), and between the conducting tissue of the ventricle and the ventricular muscle (fasciculo-ventricular pathways). These rarer accessory pathways are sometimes collectively referred to as Mahaim pathways or Mahaim fibres.[4]
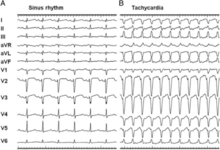
Mahaim pathways are typically seen on the right side of the heart, with their ventricular connection lying within or close to the right bundle branch.[4] The fibres often conduct slowly and only from the atria to the ventricles (antegrade) without conducting in the reverse (retrograde) direction. Unlike most atrio-ventricular accessory pathways, their speed of conduction varies according to the frequency with which they are stimulated, referred to as decremental conduction.[4] If conduction to the ventricles occurs solely through the pathway (maximal pre-excitation), as occurs during arrhythmias like antidromic atrioventricular re-entrant tachycardia, the ECG appearance is of QRS complexes with a left bundle branch block morphology which can be mistaken for ventricular tachycardia. However, due to their slow, decremental conduction, during sinus rhythm the 12-lead ECG will often show little pre-excitation.[4]
References
- Josephson, Mark E.,. Josephson's clinical cardiac electrophysiology : techniques and interpretations. Preceded by: Josephson, Mark E. (Fifth ed.). Baltimore, MD. ISBN 9781496326614. OCLC 938434294.CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link)
- Bhatia, Atul; Sra, Jasbir; Akhtar, Masood (March 2016). "Preexcitation Syndromes". Current Problems in Cardiology. 41 (3): 99–137. doi:10.1016/j.cpcardiol.2015.11.002. ISSN 1535-6280. PMID 26897561.
- Katritsis, Demosthenes G.; Boriani, Giuseppe; Cosio, Francisco G.; Hindricks, Gerhard; Jaïs, Pierre; Josephson, Mark E.; Keegan, Roberto; Kim, Young-Hoon; Knight, Bradley P.; Kuck, Karl-Heinz; Lane, Deirdre A. (2017-03-01). "European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardiaca y Electrofisiologia (SOLAECE)". Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology. 19 (3): 465–511. doi:10.1093/europace/euw301. ISSN 1532-2092. PMID 27856540.
- Katritsis, Demosthenes G.; Wellens, Hein J.; Josephson, Mark E. (April 2017). "Mahaim Accessory Pathways". Arrhythmia & Electrophysiology Review. 6 (1): 29–32. doi:10.15420/aer.2016:35:1. ISSN 2050-3369. PMC 5430943. PMID 28507744.