Vulvar cancer
Vulvar cancer is a cancer of the vulva, the outer portion of the female genitals.[1] It most commonly affects the outer vaginal lips.[1] Less often, the inner vaginal lips, clitoris, or vaginal glands.[1] Symptoms include a lump, itchiness, changes in the skin, or bleeding from the vulva.[1]
| Vulvar cancer | |
|---|---|
_(14581300578).jpg) | |
| Drawing of vulvar cancer | |
| Specialty | Gynecology |
| Symptoms | Lump, itchiness, changes in the skin, or bleeding of the vulva[1] |
| Usual onset | After the age of 45[2] |
| Types | Squamous cell cancer, adenocarcinoma, melanoma, sarcoma, basal cell carcinoma.[3] |
| Risk factors | Vulvar intraepithelial neoplasia (VIN), HPV infection, genital warts, smoking, many sexual partners[1][3] |
| Diagnostic method | Physical examination, tissue biopsy[1] |
| Differential diagnosis | Lichen sclerosus, hyperplasia[4] |
| Prevention | HPV vaccination[5] |
| Treatment | Surgery, radiation therapy, chemotherapy, biologic therapy[1] |
| Prognosis | Five-year survival ~ 71% (US 2015)[2] |
| Frequency | 44,200 (2018)[6] |
| Deaths | 15,200 (2018)[6] |
Risk factors include vulvar intraepithelial neoplasia (VIN), HPV infection, genital warts, smoking, and many sexual partners.[1][3] Most vulvar cancers are squamous cell cancers.[4] Other types include adenocarcinoma, melanoma, sarcoma, and basal cell carcinoma.[3] Diagnosis is suspected based on physical examination and confirmed by tissue biopsy.[1] Routine screening is not recommended.[3]
Prevention may include HPV vaccination.[5] Standard treatments may include surgery, radiation therapy, chemotherapy, and biologic therapy.[1] Vulvar cancer newly affected about 44,200 people and resulted in 15,200 deaths globally in 2018.[6] In the United States, it newly occurred in about 6,070 people with 1,280 deaths a year.[2] Onset is typically after the age of 45.[2] The five-year survival rates for vulvar cancer is around 71% as /of 2015.[2] Outcomes, however, are affected by whether spread has occurred to lymph nodes.[4]
Signs and symptoms
_(14750388526).jpg)
The signs and symptoms can include:
- Itching, burn, or bleeding on the vulva that does not go away.
- Changes in the color of the skin of the vulva, so that it looks redder or whiter than is normal.
- Skin changes in the vulva, including what looks like a rash or warts.
- Sores, lumps, or ulcers on the vulva that do not go away.
- Pain in the pelvis, especially during urination or sex.[7]
Typically, a lesion presents in the form of a lump or ulcer on the labia majora and may be associated with itching, irritation, local bleeding or discharge, in addition to pain with urination or pain during sexual intercourse.[8] The labia minora, clitoris, perineum and mons are less commonly involved.[9] Due to modesty or embarrassment, people may put off seeing a doctor.[10]
Melanomas tend to display the typical asymmetry, uneven borders and dark discoloration as do melanomas in other parts of the body.
Adenocarcinoma can arise from the Bartholin gland and present with a painful lump.[11]
Causes
Two main pathophysiological pathways are currently understood to contribute to development of vulvar cancer - human papillomavirus (HPV) infection and chronic inflammation or autoimmunity affecting the vulvar area.[12][13][14]
HPV DNA can be found in up to 87% of vulvar intraepithelial neoplasia (VIN) and 29% of invasive vulvar cancers; HPV 16 is the most commonly detected subtype in VIN and vulvar cancer, followed by HPV 33 and HPV 18. [15] VIN is a superficial lesion of the skin that has not invaded the basement membrane—or a pre-cancer.[16] VIN may progress to carcinoma-in-situ and, eventually, squamous cell cancer.
Chronic inflammatory conditions of the vulva that may be precursors to vulvar cancer include lichen sclerosus, which can predispose to differentiated VIN. [17][18]
Risk factors
Risk factors for vulvar cancer are largely related to the causal pathways above, involving exposure or infection with the HPV virus and/or acquired or innate auto-immunity.[19][20]
- Increasing age
- History of vulvar or cervical intraepithelial neoplasia
- Increased number of male sexual partners
- Prior history pre-invasive or invasive cervical cancer
- History of cigarette smoking
- Infection with human immunodeficiency virus (HIV)
- Vulvar lichen sclerosus
- Immunodeficiency syndromes
- Northern European ancestry
Diagnosis
Examination of the vulva is part of the gynecologic evaluation and should include a thorough inspection of the perineum, including areas around the clitoris and urethra, and palpation of the Bartholin's glands.[21] The exam may reveal an ulceration, lump or mass in the vulvar region. Any suspicious lesions need to be sampled, or biopsied. This can generally be done in an office setting under local anesthesia. Small lesions can be removed under local anesthesia as well. Additional evaluation may include a chest X-ray, an intravenous pyelogram, cystoscopy or proctoscopy, as well as blood counts and metabolic assessment.
Types
Many cancer can develop in vulvar structures.[22]
Squamous cell carcinoma
Most vulvar cancer (approximately 90%)[23] is squamous cell carcinoma, which originates from epidermal squamous cells, the most common type of skin cell. Carcinoma-in-situ is a precursor lesion of squamous cell cancer that does not invade through the basement membrane. While this type of lesion is more common with older age, young women with risk factors may also be affected. In the elderly, complications may occur due to the presence of other medical conditions.
Squamous lesions tend to arise in a single site and occur most commonly in the vestibule.[24] They grow by local extension and spread via the local lymph system. The lymphatics of the labia drain to the upper vulva and mons, then to both superficial and deep inguinal and femoral lymph nodes. The last deep femoral node is called the Cloquet’s node.[24] Spread beyond this node reaches the lymph nodes of the pelvis. The tumor may also invade nearby organs such as the vagina, urethra, and rectum and spread via their lymphatics.
A verrucous carcinoma of the vulva is a rare subtype of squamous cell cancer and tends to appear as a slowly growing wart. Verrucous vulvar cancers tend to have good overall prognoses.[25]
Melanoma
Melanoma is the second most common type of vulvar cancer and causes 8–10% of vulvar cancer cases.[24] These lesions arise from melanocytes, the cells that give skin color and are most common in Caucasian women 50–80 years old.[26] Melanoma of the vulva behaves like melanoma in any other location and may affect a much younger population.
There are three distinct types of vulvar melanoma: superficial spreading, nodular, and acral lentigous melanoma. Vulvar melanomas are unique in that they are microstaged with the Chung, Clark and/or Breslow systems, which specify stage and tumor depth of invasion. In general, they come with a high risk of metastasis and carry a poor overall prognosis.[24]
Basal cell carcinoma
Basal cell carcinoma makes up about 1–2% of vulvar cancer. These tend to be slow-growing lesions on the labia majora but can occur anywhere on the vulva. Their behavior is similar to basal cell cancers in other locations. They often grow locally and have low risk for deep invasion or metastasis.
Treatment involves excision, but these lesions have a tendency to recur if not completely removed.[27]
Bartholin gland carcinoma
The Bartholin gland is a rare malignancy and usually occurs in women in their mid-sixties.
Other lesions
Other lesions, such as adenocarcinoma (of the Bartholin glands, for example) or sarcoma, may cause vulvar cancer as well.[28] Erythroplasia of Queyrat, typically found on the penis may affect the vulvae in females.[29]
Staging
Anatomical staging supplemented preclinical staging starting in 1988. FIGO’s revised TNM classification system uses tumor size (T), lymph node involvement (N) and presence or absence of metastasis (M) as criteria for staging. Stages I and II describe the early stages of vulvar cancer that still appear to be confined to the site of origin. Stage III cancers include greater disease extension to neighboring tissues and inguinal lymph nodes on one side. Stage IV indicates metastatic disease to inguinal nodes on both sides or distant metastases.[30]
- Illustrations showing stages of vulvar cancer'"`UNIQ--ref-0000004C-QINU`"'
 Stage 1A and 1B vulvar cancer
Stage 1A and 1B vulvar cancer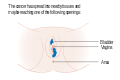 Stage 2 vulvar cancer
Stage 2 vulvar cancer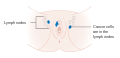 Stage 3 vulvar cancer
Stage 3 vulvar cancer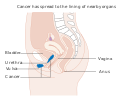 Stage 4A vulvar cancer
Stage 4A vulvar cancer Stage 4B vulvar cancer
Stage 4B vulvar cancer
Differential diagnosis
Other cancerous lesions in the differential diagnosis include Paget's disease of the vulva and vulvar intraepithelial neoplasia (VIN). Non-cancerous vulvar diseases include lichen sclerosus, squamous cell hyperplasia, and vulvar vestibulitis. A number of diseases cause infectious lesions including herpes genitalis, human papillomavirus, syphilis, chancroid, granuloma inguinale, and lymphogranuloma venereum.
Treatment
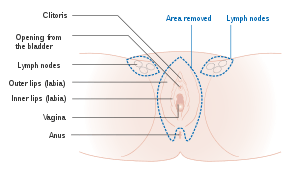
Surgery is a mainstay of therapy depending on anatomical staging and is usually reserved for cancers that have not spread beyond the vulva.[30] Surgery may involve a wide local excision, radical partial vulvectomy, or radical complete vulvectomy with removal of vulvar tissue, inguinal and femoral lymph nodes. In cases of early vulvar cancer, the surgery may be less extensive and consist of wide excision or a simple vulvectomy. Surgery is significantly more extensive when the cancer has spread to nearby organs such as the urethra, vagina, or rectum. Complications of surgery include wound infection, sexual dysfunction, edema and thrombosis, as well as lymphedema secondary to dissected lymph nodes.[31]
Sentinel lymph node (SLN) dissection is the identification of the main lymph node(s) draining the tumor, with the aim of removing as few nodes as possible, decreasing the risk of adverse effects. Location of the sentinel node(s) may require the use of technetium(99m)-labeled nano-colloid, or a combination of technetium and 1% isosulfan blue dye, wherein the combination may reduce the number of women with "'missed"' groin node metastases compared with technetium only.[31]
Radiation therapy may be used in more advanced vulvar cancer cases when disease has spread to the lymph nodes and/or pelvis. It may be performed before or after surgery. Chemotherapy is not usually used as primary treatment but may be used in advanced cases with spread to the bones, liver or lungs. It may also be given at a lower dose together with radiation therapy.[32]
Women with vulvar cancer should have routine follow-up and exams with their oncologist, often every 3 months for the first 2–3 years after treatment. They should not have routine surveillance imaging to monitor the cancer unless new symptoms appear or tumor markers begin rising.[33] Imaging without these indications is discouraged because it is unlikely to detect a recurrence or improve survival and is associated with its own side effects and financial costs.[33]
Prognosis
Overall, five-year survival rates for vulvar cancer are around 78%[24] but may be affected by individual factors including cancer stage, cancer type, patient age and general medical health. Five-year survival is greater than 90% for patients with stage I lesions but decreases to 20% when pelvic lymph nodes are involved. Lymph node involvement is the most important predictor of prognosis.[34]
Prognosis dependents on the stage of cancer, which refers the amount and spread of cancer in the body.[35] The stages are broken into 4 categories. Stage one also called "localized" and is when the cancer is limited to one part of the body.[35] This has the highest survival rate of 59%.[35] When the cancer starts to spread this is referred to "distant" or "regional", this stage usually involves the cancer being spread to the lymph nodes.[35] This survival rate is 29%. The third stage is when the cancer has metastasized and spread throughout the body, this is the lowest survival rate of 6%. When vulvar cancer is caught early that is when the survival rate is at its highest.[35]
Epidemiology
Vulvar cancer newly affected about 44,200 people and resulted in 15,200 deaths globally in 2018.[6]
Vulvar cancer can be split up into two types. One starts as an infection by human papillomavirus, which leads to vulvar intraepithelial neoplasia (VIN) and potentially on to vulvar cancer.[36] This is most common in younger women, predominantly under the age of 40.[36] The second type is vulvar non-neoplastic epithelial disorders (VNED). This is most common in older women, due to the increased risk for developing cellular atypia which in turn leads to cancer.[36]
United Kingdom
Vulvar cancer causes less than 1% of all cancer cases and deaths but around 6% of all gynecologic cancers diagnosed in the UK. Around 1,200 women were diagnosed with the disease in 2011, and 400 women died in 2012.[37] In the United Kingdom 7 out of 10 vulval cancer patients have major surgical resection as part of their cancer treatment.[38] 22% of patients use radiotherapy and only 7% use chemotherapy as a treatment plan.[38] There are very high survival rates, patients diagnosed with vulvar cancer have a 82% of living more than one year, a 64% chance of living at least 5 years and a 53% chance of living ten or more years. [38] The rate of survival increases dependent on age of patient and the stage the cancer was found in.
United States
In the United States, it newly occurred in about 6,070 people with 1,280 deaths a year.[2] It makes up about 0.3% of new cancer cases,[2] and 5% of gynecologic cancers in the United States.[39] Vulvar cancer cases have been rising in the United States at an increase of .6% each year for the past ten years.[40]
References
- "Vulvar Cancer Treatment". National Cancer Institute. 9 April 2019. Retrieved 31 May 2019.
- "Cancer of the Vulva - Cancer Stat Facts". SEER. Retrieved 30 May 2019.
- Sam, A; George, J; Mathew, B (April 2019). "Less Common Gynecologic Malignancies: An Integrative Review". Seminars in Oncology Nursing. 35 (2): 175–181. doi:10.1016/j.soncn.2019.02.004. PMID 30867101.
- "Vulvar Cancer Treatment". National Cancer Institute. 1 February 2019. Retrieved 31 May 2019.
- Signorelli, C; Odone, A; Ciorba, V; Cella, P; Audisio, RA; Lombardi, A; Mariani, L; Mennini, FS; Pecorelli, S; Rezza, G; Zuccotti, GV; Peracino, A (July 2017). "Human papillomavirus 9-valent vaccine for cancer prevention: a systematic review of the available evidence". Epidemiology and Infection. 145 (10): 1962–1982. doi:10.1017/S0950268817000747. PMID 28446260.
- "Cancer today". IARC. Retrieved 30 May 2019.
- "What Are the Symptoms of Vaginal and Vulvar Cancers?". CDC. 13 March 2014. Retrieved 2016-03-26.
- "Vulvar Cancer Treatment". National Cancer Institute. 1980-01-01. Retrieved 2015-04-14.
- "What is vulvar cancer?". cancer.org. Retrieved 2015-04-14.
- Zacur H, Genadry R, Woodruff JD (April 1980). "The patient-at-risk for development of vulvar cancer". Gynecologic Oncology. 9 (2): 199–208. doi:10.1016/0090-8258(80)90028-1. PMID 7372192.
- Copeland LJ, Sneige N, Gershenson DM, McGuffee VB, Abdul-Karim F, Rutledge FN (June 1986). "Bartholin gland carcinoma". Obstetrics and Gynecology. 67 (6): 794–801. doi:10.1097/00006250-198606000-00009. PMID 3010205.
- de Koning MN, Quint WG, Pirog EC (March 2008). "Prevalence of mucosal and cutaneous human papillomaviruses in different histologic subtypes of vulvar carcinoma". Modern Pathology. 21 (3): 334–44. doi:10.1038/modpathol.3801009. PMID 18192968.
- Weberpals JI, Lo B, Duciaume MM, Spaans JN, Clancy AA, Dimitroulakos J, Goss GD, Sekhon HS (August 2017). "Vulvar Squamous Cell Carcinoma (VSCC) as Two Diseases: HPV Status Identifies Distinct Mutational Profiles Including Oncogenic Fibroblast Growth Factor Receptor 3". Clinical Cancer Research. 23 (15): 4501–4510. doi:10.1158/1078-0432.CCR-16-3230. PMID 28377483.
- Halec G, Alemany L, Quiros B, Clavero O, Höfler D, Alejo M, Quint W, Pawlita M, Bosch FX, de Sanjose S (April 2017). "Biological relevance of human papillomaviruses in vulvar cancer". Modern Pathology. 30 (4): 549–562. doi:10.1038/modpathol.2016.197. PMID 28059099.
- de Sanjosé S, Alemany L, Ordi J, Tous S, Alejo M, Bigby SM, et al. (November 2013). "Worldwide human papillomavirus genotype attribution in over 2000 cases of intraepithelial and invasive lesions of the vulva". European Journal of Cancer. 49 (16): 3450–61. doi:10.1016/j.ejca.2013.06.033. PMID 23886586.
- "What is Vulvar Cancer?". Society of Gynecologic Oncology. Retrieved 19 November 2014.
- van de Nieuwenhof HP, Bulten J, Hollema H, Dommerholt RG, Massuger LF, van der Zee AG, de Hullu JA, van Kempen LC (February 2011). "Differentiated vulvar intraepithelial neoplasia is often found in lesions, previously diagnosed as lichen sclerosus, which have progressed to vulvar squamous cell carcinoma". Modern Pathology. 24 (2): 297–305. doi:10.1038/modpathol.2010.192. PMID 21057461.
- Bigby SM, Eva LJ, Fong KL, Jones RW (November 2016). "The Natural History of Vulvar Intraepithelial Neoplasia, Differentiated Type: Evidence for Progression and Diagnostic Challenges". International Journal of Gynecological Pathology. 35 (6): 574–584. doi:10.1097/PGP.0000000000000280. PMID 26974999.
- Madsen BS, Jensen HL, van den Brule AJ, Wohlfahrt J, Frisch M (June 2008). "Risk factors for invasive squamous cell carcinoma of the vulva and vagina--population-based case-control study in Denmark". International Journal of Cancer. 122 (12): 2827–34. doi:10.1002/ijc.23446. PMID 18348142.
- Brinton LA, Thistle JE, Liao LM, Trabert B (May 2017). "Epidemiology of vulvar neoplasia in the NIH-AARP Study". Gynecologic Oncology. 145 (2): 298–304. doi:10.1016/j.ygyno.2017.02.030. PMC 5629039. PMID 28236455.
- "Vulvar Cancer". Gynecologic Neoplasms. Armenian Health Network, Health.am. 2005. Retrieved 2007-11-08.
- Hoffman, Barbara (2012). Williams Gynecology (2nd. ed.). New York: McGraw-Hill Medical. pp. 794–806. ISBN 9780071716727.
- Canavan TP, Cohen D (October 2002). "Vulvar cancer". American Family Physician. 66 (7): 1269–74. PMID 12387439. Retrieved 2010-03-06.
- Hoffman B, Schorge J, Schaffer J, Halvorson L, Bradshaw K, Cunningham G (2012). Williams Gynecology (2nd ed.). The McGraw-Hill Company, Inc. ISBN 978-0-07-171672-7.
- "American Cancer Society: What is Vulvar Cancer?". www.cancer.org. Retrieved 2014-06-11.
- Evans RA (December 1994). "Review and current perspectives of cutaneous malignant melanoma". Journal of the American College of Surgeons. 179 (6): 764–7. PMID 7952494.
- DeCherney AH, Nathan L, Laufer N, Roman AS (2013). Current Diagnosis and Treatment: Obstetrics and Gynecology (11th ed.). USA: The McGraw-Hill Companies, Inc. ISBN 978-0-07-163856-2.
- Visco AG, Del Priore G (February 1996). "Postmenopausal bartholin gland enlargement: a hospital-based cancer risk assessment". Obstetrics and Gynecology. 87 (2): 286–90. doi:10.1016/0029-7844(95)00404-1. PMID 8559540.
- Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 1050. ISBN 978-1-4160-2999-1.
- International Federation of Gynecologists and Obstetricians (FIGO) (2000). "Staging classification and clinical practice guidelines of gynaecologic cancers" (PDF). Archived from the original (PDF) on 2006-04-23. Retrieved 2006-10-13.
- Lawrie TA, Patel A, Martin-Hirsch PP, Bryant A, Ratnavelu ND, Naik R, Ralte A (June 2014). "Sentinel node assessment for diagnosis of groin lymph node involvement in vulval cancer". The Cochrane Database of Systematic Reviews (6): CD010409. doi:10.1002/14651858.CD010409.pub2. PMC 6457826. PMID 24970683.
- "What are the treatment options?". Society of Gynecologic Oncology. Retrieved 19 November 2014.
- Society of Gynecologic Oncology (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, Society of Gynecologic Oncology, retrieved 19 February 2013
- Farias-Eisner R, Cirisano FD, Grouse D, Leuchter RS, Karlan BY, Lagasse LD, Berek JS (April 1994). "Conservative and individualized surgery for early squamous carcinoma of the vulva: the treatment of choice for stage I and II (T1-2N0-1M0) disease". Gynecologic Oncology. 53 (1): 55–8. doi:10.1006/gyno.1994.1087. PMID 8175023.
- "Cancer of the Vulva - Cancer Stat Facts". SEER. Retrieved 2019-12-03.
- Alkatout, Ibrahim; Schubert, Melanie; Garbrecht, Nele; Weigel, Marion; Jonat, Walter; Mundhenke, Christoph; Gunther, Veronika (March 20, 2015). "Vulvar cancer: epidemiology, clinical presentation, and management options". International Journal of Women's Health. 7: 305–313. Retrieved 17 November 2019.
- "Vulval cancer statistics". Cancer Research UK. Retrieved 28 October 2014.
- "Vulval cancer statistics". Cancer Research UK. 2015-05-14. Retrieved 2019-12-03.
- "Vulvar Cancer Treatment". National Cancer Institute. 1980-01-01. Retrieved 12 May 2015.
- "Cancer of the Vulva - Cancer Stat Facts". SEER. Retrieved 2019-12-03.
External links
| Classification | |
|---|---|
| External resources |
- Information from the National Cancer Institute
- Vulvar Cancer. Timothy P. Canavan and Donna Cohen. Am Fam Physician 2002;66:1269–74,1276. Review article for general practitioners.