Twin-to-twin transfusion syndrome
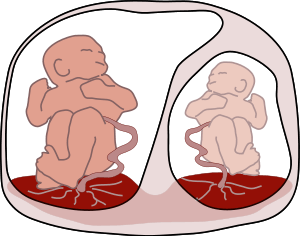
Twin-to-twin transfusion syndrome (TTTS), also known as feto-fetal transfusion syndrome (FFTS), twin oligohydramnios-polyhydramnios sequence (TOPS) and stuck twin syndrome is a complication of disproportionate blood supply, resulting in high morbidity and mortality. It can affect monochorionic multiples, that is, multiple pregnancies where two or more fetuses share a chorion and hence a single placenta. Severe TTTS has a 60–100% mortality rate.[1]
| Twin-to-twin transfusion syndrome | |
|---|---|
 | |
| Twin-to-twin transfusion syndrome | |
| Specialty | Perinatology, neonatology |
Cause
As a result of sharing a single placenta, the blood supplies of monochorionic twin fetuses can become connected, so that they share blood circulation: although each fetus uses its own portion of the placenta, the connecting blood vessels within the placenta allow blood to pass from one twin to the other. It is thought that most monochorionic placentae have these "shared connections" that cross the placenta, with the net flow volumes being equal between them. This state is sometimes referred to as "flow balance". Depending on the number, type and direction of the interconnecting blood vessels (anastomoses), blood can be transferred disproportionately from one twin (the "donor") to the other (the "recipient"), due to a state of "flow imbalance" imparted by new blood vessel growth across the placental "equator", the line that divides each baby's proportion of the shared placenta. This state of transfusion causes the donor twin to have decreased blood volume, retarding the donor's development and growth, and also decreased urinary output, leading to a lower than normal level of amniotic fluid (becoming oligohydramnios). The blood volume of the recipient twin is increased, which can strain the fetus's heart and eventually lead to heart failure, and also higher than normal urinary output, which can lead to excess amniotic fluid (becoming polyhydramnios).
TTTS usually develops during the period of peak placental growth, starting in week 16 and proceeding through week 25; after this point, the placenta's growth decelerates, essentially stopping just after week 30. While TTTS has occasionally been detected beyond this timepoint, it is thought that its occurrence beyond week 30 may be due to a placental embolism that upsets the flow balance of the shared connections between the babies. TTTS is potentially lethal to either or both twins, no matter when it is detected. However, when detected past week 25, emergency delivery may be considered to rescue the babies if the TTTS is severe.
Other than requiring a monochorionic twin (or higher multiple) pregnancy, the underlying causes of TTTS are not known. It is not known to be hereditary or genetic.
Imbalance in development
Some doctors recommend complete bed-rest for the mother coupled with massive intakes of protein as a therapy to try to counteract the syndrome. Research completed shows these nutritional supplements do work. Diet supplementation was associated with lower overall incidence of TTTS (20/52 versus 8/51, P = 0.02) and with lower prevalence of TTTS at delivery (18/52 versus 6/51, P = 0.012) when compared with no supplementation. In the study, nutritional supplementation contained 250kcal, consisting of 6g of lipids, 40g of carbohydrates, 9g of protein, vitamins and minerals, consumed three times per day. Nutritional intervention also significantly prolonged the time between the diagnosis of TTTS and delivery (9.4 ± 3.7 weeks versus 4.6 ± 6.5 weeks; P = 0.014). The earlier nutritional regimen was introduced, the lesser chance of detecting TTTS ( P = 0.001). Although not statistically significant, dietary intervention was also associated with lower Quintero stage, fewer invasive treatments, and lower twin birth weight discordance. Diet supplementation appears to counter maternal metabolic abnormalities in monochorionic twin pregnancies and improve perinatal outcomes in TTTS when combined with the standard therapeutic options. Nutritional therapy appears to be most effective in mitigating cases that are caught in Quintero Stage I, little effect has been observed in those that are beyond Stage I.[2]
Diagnosis
Quintero Stages
A staging system is commonly used to classify the severity of TTTS.[3]
Stage I: A small amount of amniotic fluid (oligohydramnios) is found around the donor twin and a large amount of amniotic fluid (polyhydramnios) is found around the recipient twin.
Stage II: In addition to the description above, the ultrasound is not able to identify the bladder in the donor twin.
Stage III: In addition to the characteristics of Stages I and II, there is abnormal blood flow in the umbilical cords of the twins.
Stage IV: In addition to all of the above findings, the recipient twin has swelling under the skin and appears to be experiencing heart failure (fetal hydrops).
Stage V: In addition to all of the above findings, one of the twins has died. This can happen to either twin. The risk to either the donor or the recipient is roughly equal & is quite high in Stage II or higher TTTS.
The Quintero staging does not provide information about prognosis, and other staging systems have been proposed.[4]
Treatment
Various treatments for TTTS include:
Non treatment
This is equivalent of zero intervention. It has been associated with almost 100% mortality rate of one or all fetuses. Exceptions to this include patients that are still in Stage 1 TTTS and are past 22 weeks' gestation.
Adjustment of amniotic fluid
Serial amniocentesis
This procedure involves removal of amniotic fluid periodically throughout the pregnancy under the assumption that the extra fluid in the recipient twin can cause preterm labor, perinatal mortality, or tissue damage. In the case that the fluid does not reaccumulate, the reduction of amniotic fluid stabilizes the pregnancy. Otherwise the treatment is repeated as necessary. There is no standard procedure for how much fluid is removed each time. There is a danger that if too much fluid is removed, the recipient twin could die. This procedure is associated with a 66% survival rate of at least one fetus, with a 15% risk of cerebral palsy and average delivery occurring at 29 weeks' gestation.
Septostomy, or iatrogenic disruption of the dividing membrane
This procedure involves the tearing of the dividing membrane between fetuses such that the amniotic fluid of both twins mixes under the assumption that pressure is different in either amniotic sac and that its equilibration will ameliorate progression of the disease. It has not been proven that pressures are different in either amniotic sac. Use of this procedure can preclude use of other procedures as well as make difficult the monitoring of disease progression. In addition, tearing the dividing membrane has contributed to cord entanglement and demise of fetuses through physical complications.
Adjustment of blood supply
Laser therapy
This procedure involves endoscopic surgery using laser to interrupt the vessels that allow exchange of blood between fetuses under the assumption that the unequal sharing of blood through these vascular communications leads to unequal levels of amniotic fluid. Each fetus remains connected to its primary source of blood and nutrition, the placenta, through the umbilical cord. This procedure is conducted once, with the exception of all vessels not having been found. The use of endoscopic instruments allows for short recovery time. This procedure has been associated with 85% survival rate of at least one fetus, with a 6–7% risk of cerebral palsy and average delivery occurring at 32–33 weeks' gestation.[5]
Twin anemia-polycythemia sequence (TAPS) may occur after laser surgery for TTTS (post-laser form). The spontaneous form of TAPS complicates approximately 3 to 5% of monochorionic twin pregnancies, whereas the post-laser form occurs in 2 to 13% of TTTS cases.[6][7] The pathogenesis of TAPS is based on the presence of few, minuscule arterio-venous (AV) placental anastomoses (diameter <1mm)[8] allowing a slow transfusion of blood from the donor to the recipient and leading gradually to highly discordant Hb levels.[9]
A recent review found that laser coagulation resulted in fewer fetal and perinatal deaths than amnioreduction and septostomy, and recommended its use for all states of TTTS.[10]
Umbilical cord occlusion
This procedure involves the ligation or otherwise occlusion of the umbilical cord to interrupt the exchange of blood between the fetuses. The procedure is typically offered in cases where one of the fetuses is presumed moribund and endangering the life or health of the other twin through resultant hypotension. Use of this treatment has decreased as TTTS is identified and treated in earlier stages and with better outcomes. When used, it is associated with an 85% survival rate of the remaining fetus(es) with 5% risk of cerebral palsy and a 33–39 weeks of gestation at delivery.
Epidemiology
Based on recent (2005) US NCHS data, the rate of multiple births is now approximately 3.4% (4,138,349 total births, of which 139,816 were twins or higher-order multiple births). The majority of identical twins share a common (monochorionic) placenta, and of these approximately 15% go on to develop TTTS. By extrapolating the number of expected identical twins (about one-third) from annual multiple births, and the number of twins with monochorionic placentae (about two-thirds), and from these the number thought to develop TTTS (about 15%), there are at least 4,500 TTTS cases per year in the U.S. alone: 139,816 × .33 × .66 × .15 = 4,568 cases of TTTS per year in U.S. (involving more than 9,000 babies.) Since spontaneous pregnancy losses and terminations that occur prior to 20 weeks go uncounted by the C.D.C., this estimate of TTTS cases may be very conservative. Although infertility treatments have increased the rate of multiple birth, they have not appreciably diluted the expected incidence of identical twins. Studies show a higher rate of identical twins (up to 20 times with IVF) using these treatments versus spontaneous pregnancy rates.
One Australian study, however, noted an occurrence of only 1 in 4,170 pregnancies, or 1 in 58 twin gestations. This distinction could be partly explained by the "hidden mortality" associated with MC multifetal pregnancies—instances lost due to premature rupture of membrane (PROM) or intrauterine fetal demise before a thorough diagnosis of TTTS can be made.[11]
History
TTTS was first described by a German obstetrician, Friedrich Schatz, in 1875. Once defined by neonatal parameters—differences in birth weight and cord hemoglobin at the time of delivery—TTTS is now defined differently. Today, it is known that discordant fetal weights will most likely be a late manifestation, and fetal hemoglobin through cordocentesis is often equivalent in the twin pair even in severe TTTS.[11]
In art

A painting known as the De Wikkelkinderen (The Swaddled Children), from 1617, is thought to represent a depiction of TTTS.[12] The drawing shows twins that appear to be identical, but one is pale (possibly anemic), while the other is red (possibly polycythemic). Analysis of the family histories of the owners of the painting suggests that the twins did not survive to adulthood, although whether that is due to TTTS is uncertain.
References
- Zach T, Ford SP. "Twin-to-Twin Transfusion Syndrome". EMedicine. Retrieved July 22, 2006.
- Chiossi, Giuseppe (2008). "Nutritional Supplementation in Monochorionic Diamniotic Twin Pregnancies: Impact on Twin-Twin Transfusion Syndrome". American Journal of Perinatology. American Journal of Perinatology. 25 (10): 667–72. doi:10.1055/s-0028-1091400. PMID 18942043. Retrieved August 7, 2012.
- "Understanding the Stages of TTTS". UC San Diego. Archived from the original on April 10, 2012. Retrieved April 23, 2012.
- Cristina, Rossi (2009). "The Efficacy of Quintero Staging System to Assess Severity of Twin-Twin Transfusion Syndrome Treated with Laser Therapy: A Systematic Review with Meta-Analysis". American Journal of Perinatology. Thieme Medical Publishers. p. 537. doi:10.1055/s-0029-1215430. Retrieved August 7, 2012.
- Benoit RM, Baschat AA. (2014) Twin-to-twin transfusion syndrome: prenatal diagnosis and treatment. American J of Perinatology
- Robyr R, Lewi L, Salomon LJ, Yamamoto M, Bernard JP, Deprest J et al. Prevalence and management of late fetal complications following successful selective laser coagulation of chorionic plate anastomoses in twin-to-twin transfusion syndrome. Am J Obstet Gynecol 2006; 194(3):796-803.
- Habli M, Bombrys A, Lewis D, Lim FY, Polzin W, Maxwell R et al. Incidence of complications in twin-twin transfusion syndrome after selective fetoscopic laser photocoagulation: a single-center experience. Am J Obstet Gynecol 2009; 201(4):417.
- Lopriore E, Deprest J, Slaghekke F, Oepkes D, Middeldorp JM, Vandenbussche FP et al. Placental characteristics in monochorionic twins with and without twin anemia-polycythemia sequence. Obstet Gynecol 2008; 112(4):753-758.
- Slaghekke F, Kist WJ, Oepkes D, Pasman SA, Middeldorp JM, Klumper FJ et al. Twin anemia-polycythemia sequence: diagnostic criteria, classification, perinatal management and outcome. Fetal Diagn Ther 2010; 27(4):181-190.
- Roberts D, Neilson JP, Kilby M, Gates S. (2014) Interventions for the treatment of twin–twin transfusion syndrome. Cochrane Database Syst Rev
- Johnson, A.; Moise, K. J. "Improving Survival in Twin-Twin Transfusion Syndrome. Contemporary OB/GYN December 2006" (PDF). Archived from the original (PDF) on January 9, 2009.
- Berger H, de Waard F, Molenaar Y (2000). "A case of twin-to-twin transfusion in 1617". Lancet. 356 (9232): 847–8. doi:10.1016/S0140-6736(00)02665-9. PMID 11022944.
External links
| Classification | |
|---|---|
| External resources |
|