Theralizumab
Theralizumab (also known as TGN1412, CD28-SuperMAB, and TAB08) is an immunomodulatory drug developed by Professor Thomas Hünig of the University of Würzburg.
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized (from mouse) |
| Target | CD28 |
| Clinical data | |
| Routes of administration | intravenous |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
| UNII | |
| (verify) | |
It was withdrawn from development after inducing severe inflammatory reactions in the first-in-human study by PAREXEL in London in March 2006.[1] The developing company, TeGenero Immuno Therapeutics, went bankrupt later that year.
The commercial rights were then acquired by a Russian startup, TheraMAB.[2] The drug was renamed TAB08. Phase I and II clinical trials have been completed for arthritis[3] and clinical trials have been initiated for cancer.
Originally intended for the treatment of B cell chronic lymphocytic leukemia (B-CLL) and rheumatoid arthritis,[4] TGN1412 is a humanised monoclonal antibody that not only binds to, but is a strong agonist for, the CD28 receptor of the immune system's T cells.[5] CD28 is the co-receptor for the T cell receptor; It binds to receptors on the interacting partner in the reaction through one of its ligands (B7 family).
In its first human clinical trials, it caused catastrophic systemic organ failures in the subjects, despite being administered at a supposed sub-clinical dose of 0.1 mg per kg; some 500 times lower than the dose found safe in animals.[6] Six volunteers were hospitalized on 13 March 2006, at least four of these suffering from multiple organ dysfunction. Tentative opinions from an as-yet uncompleted inquiry suggest that the problems resulted from "unforeseen biological action in humans", rather than breach of trial protocols, and the case therefore has had important ramifications for future trials of potentially powerful clinical agents.
Scientists in early 2007 put forth the theory that the drug acted in a different fashion in humans as compared with the laboratory animals in which the drug was first tried. The severe reactions in humans could have only occurred, they believe, in those with memory T lymphocytes. Animals raised in a sterile lab would presumably have no 'memory' of previous illnesses, thus would not exhibit the severe reactions that occurred in the human subjects.[7] However this is a misunderstanding of the research: the research says that lab animals studied have fewer memory T cells than humans, and that stimulation through the CD28 receptor alone in memory T cells causes them to infiltrate organs and also activates them.[8]
The drug, which was designated as an orphan medical product by the European Medicines Agency in March 2005, was developed by TeGenero Immuno Therapeutics, tested by Parexel and manufactured by Boehringer Ingelheim.[9][10] TeGenero announced the first elucidation of the molecular structure of CD28 almost exactly one year prior to commencement of the TGN1412 phase I clinical trial.
Description of the drug
Mice of the inbred strain BALB/c were immunized with recombinant human CD28-Fc fusion proteins and boosted with a B lymphoma cell line transfected to express human CD28. Hybridomas were obtained by fusing B cells with the hybridoma partner X63Ag8.653 and screened for reactivity with human CD28 and TCR-independent mitogenic activity. Two monoclonals called 5.11A1 and 9D7 were identified. The more active of the two, 5.11A1, is a mouse IgG1 immunoglobulin.
The complementarity determining regions of 5.11A1 were cloned into the framework of human IgG and combined with IgG1 (TGN1112) or IgG4 (TGN1412) constant regions. According to the company's Investigator Brochure, "TGN1412 is a humanised monoclonal antibody directed against the human CD28 antigen. The molecule was genetically engineered by transfer of the complementarity determining regions (CDRs) from heavy and light chain variable region sequences of a monoclonal mouse anti-humanC28 [sic] antibody (5.11A1, Luhder et al., 2003) into human heavy and light chain variable frameworks. Humanised variable regions were subsequently recombined with a human gene coding for the IgG4 gamma chain and with a human gene coding for a human kappa chain, respectively."[11]
The recombinant genes were transfected into Chinese hamster ovary cells and the recombinant antibody harvested from culture supernatant.
Mechanism of action
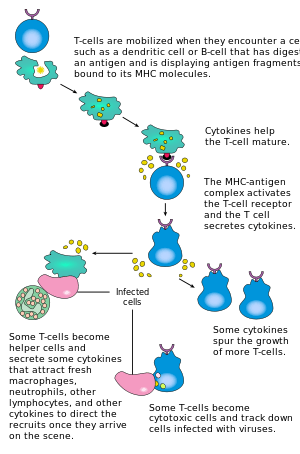
Activation of T cells normally requires both engagement of the antigen receptor (signal 1) and co-stimulation (signal 2). Studies of monoclonal antibodies specific for mouse, rat, or human CD28 identified so-called "superagonistic" antibodies that could stimulate T cells without concurrent antigen-receptor stimulation (signal 1). Whether this activity represents a stronger activity or a different activity is uncertain.
Two antibodies specific for human CD28 were identified. The more active of the two, TGN1112 (originally called 5.11A1), belonged to the IgG1 class of immunoglobulins. The other, TGN1412 (clone 9D7), belonged to the IgG4 class. The TCR-independent agonism of these antibodies involved binding to a specific part of the CD28 molecule called the C"D loop.[12] It was initially hypothesized that an antibody with this property could be therapeutically useful in stimulating the immune system in immunosuppressed patients. However, in vitro and in vivo data from animal studies later suggested that administration would lead to preferential activation of regulatory T cells, leading to a net effect of T-cell downregulation. On its website, the company wrote: "A pronounced T-cell activation and expansion mediated by CD28-SuperMAB in animal models is accompanied by the expression of anti-inflammatory cytokines, like IL-10, rather than by the severe cytokine release syndrome of pro-inflammatory mediators induced by other agents that address the TCR complex.".[4] As it turned out, the results of the first trial in humans indicate that this may not always be the case.
A new explanation for the trial mishap was suggested by the findings of a paper in Clinical Immunology. Pillai et al. found that all T cells that get activated using conventional TCR-mediated stimulation become regulatory for a brief time and express FOXP3. However, eventually most of these cells downregulate their regulatory capabilities and become effector cells. Thus, attempts to induce FOXP3+ T cells might also induce effector cells capable of causing tissue damage.[13]
Other cells activated by CD28 ligation in humans are eosinophil granulocytes. They can release IFN-γ, IL-2, IL-4, and IL-13.[14][15] However, most in vitro experiments are limited to the use of purified peripheral blood mononuclear cells (PBMN's) that do not contain those cells.
To function as an agonist, it has been suggested that TGN1412 needs to be a whole antibody, including the constant (Fc) region. According to a report by TeGenero, the F(ab)2 is not able to generate the required stimulation.[16] Unlike the related clone TGN1112, an IgG1, TGN1412 is of the subclass IgG4. This choice was made as TGN1112 showed antibody-dependent cellular cytotoxicity on CD28+ Jurkat cells. Thus the function of antibody binding via an Fcγ receptor seems to be a requirement for the immune regulation. However, cell opsonisation by antibody leads normally to phagocytosis of the labeled cells, as seen in the case of HIV.[17]
Clinical trials
The Phase I clinical trials were conducted by Parexel at an independent clinical trials unit in leased space on the premises of Northwick Park and St. Mark's Hospital, London, on 13 March 2006.[18][19] Parexel is a company that carries out drug trials on behalf of pharmaceutical and biotechnology companies. Healthy volunteers were recruited to the study with a £2,000 fee. The trial resulted in hospitalization of all six volunteers administered the drug, at least four of whom suffered multiple organ dysfunction.[20]The trial was a double-blind, randomized, placebo-controlled study, with two of the eight subjects receiving a placebo, and six receiving 1/500th of the highest dose used in previous experiments with cynomolgus macaques. All six of the trial subjects who received the drug were male, aged 19 to 34 (median 29.5); none had a notable medical history, and all were well in the 2 weeks before the trial.[19] The drug was given by intravenous infusion, starting at 8am, with an interval of around 10 minutes between patients, and each infusion lasting from 3 to 6 minutes.[19] Roughly five minutes after the last participant had received his dose, the participant who had received the first dose complained of headache, and soon afterwards fever and pain. He took his shirt off, complaining that he felt like he was burning. Shortly after, the remaining participants who received the actual drug also became ill, vomiting and complaining of severe pain. The first patient was transferred to the Northwick Park hospital's intensive care unit 12 hours after infusion, with the others following within the next 4 hours.[19] A severely affected volunteer, Mohammed Abdalla, a 28-year-old who said he had hoped to set his brother up in business in Egypt, was described as having suffered a ballooned head. This led to his description as being similar to the "Elephant Man". A volunteer also lost his fingers and toes as a result of being injected with the drug.[21]
All of the men were reported to have experienced severe cytokine release syndrome resulting in angioedema, swelling of skin and mucous membranes, akin to the effects of the complement cascade in severe allergic reaction. The patients were treated with corticosteroids to reduce inflammation, and plasma-exchange to attempt to remove TGN1412 from their circulation. Paradoxically, the men's white blood cells had vanished almost completely several hours after administration of TGN1412.[6]
According to a press release from 5 July 2006 on the North West London Hospitals NHS Trust website, where the men were treated, the patients continued to improve and "five of them went home within a month of the incident, while one patient remained in hospital until 26 June, when he also went home."[22] However, Head of pharmacology at University College London Trevor Smart has suggested that the men may never fully recover, and may suffer long-term disruption to their immune systems.
TGN1412 had not previously been given to humans (although a single patient in Northampton had been given a similar drug and had a similar reaction, according to the report after the events); however, the trial was preceded by animal testing, including in non-human primates. The company claims that these did not indicate any safety issues. The US patent application states "it could be shown in a pilot study that an in vitro administration of anti-human CD28-SuperMAB induces in a rhesus monkey in vivo a profound activation of T cells, without clinically visible side effects" and goes on to say "This antibody—in spite of its strong T cell-stimulatory properties—is very well tolerated in vivo, in contrast to all other known T cell activating substances."[23]
TeGenero has apologized to the families involved, insists that these effects were completely unexpected, and said that all protocols have been followed. An investigation by the UK drug regulator reported that the reaction was not due to contamination of the dose, or an incorrect dose being administered, but suggested that the problem was due to "on target" effects of the drug. Criticism has been raised that six participants were given the drug in such a short time, which is against the recommendations of standard literature. Despite this, the Medicines and Healthcare products Regulatory Agency (MHRA) has confirmed that they had approved the trial, including the protocol of giving the dose to all men within a short time. It appears the MHRA approved a protocol involving the doses being administered between 8.00h-10.00h (i.e., 2 hours). One of the placebo-receiving participants has explained the doses were given with 2-minute intervals. Even though the participants were dosed with short intervals, this is not a deviation from the approved protocol.
The MHRA has further stated that the initial dose of TGN1412 was intended to be the first of a course of injections, with the dosage being ramped up over time. It has been reported that the initial dose was one five-hundredth of that which the animal studies indicated was a maximum safe dose.[24] Dr. David Glover, an industry consultant, has suggested that because the antibody was raised against human CD28, the safe dosage may have been lower in humans than in animals.[25] More concerningly, it has been shown that even using information available prior to the human first dose, it can be shown that the size of the initial dose was too high. Predictions showed that the 0.1 mg starting dose would bind to 86 to 91% of all CD28 receptors in the body,[26] which means that even at the minimum starting dose selected, the investigators would anticipate seeing the maximum effect of the drug.
Criticism and controversy
As of March 2006, there appear to have been two issues. There was the issue of the trial protocol of giving the drug to six participants within a short time. While the MHRA had approved a two-hour protocol, the drug was administered to all participants within just twenty minutes, based on the statement of a study participant. Neither the companies involved nor the authorities have commented on that point. Another issue was whether the company should have anticipated that the drug would provoke this reaction in humans. The comments on the company webpage and in the patent application indicated that the company knew that this type of drug could cause a severe cytokine release syndrome. An immunologist contacted by New Scientist and who wished to be anonymous has commented that "You don’t need to be a rocket scientist to work out what will happen if you non-specifically activate every T cell in the body."[27]
While the drug had appeared to be safe in animal models, researchers noted that there were reasons why these may not be indicative of the response in humans, particularly with respect to this type of drug.[28] The BBC reported that "two of 20 monkeys used in earlier tests suffered an increase in the size of lymph nodes," but that "this information was given to the men and submitted to the test regulators."[29] TeGenero said this was transient and was evidence of the extra T cells that the drug produces.[30] Experiments with another drug affecting the CD28 receptor (but to a lesser extent than TGN1412) had also shown side effects in human trials.[31] There have been criticisms that the risks taken and the design of the protocol were insufficiently justified by proper statistical evidence.[32]
Critics of animal testing have cited the case to argue that experiments on nonhuman animals, even in species closely related to humans, are not necessarily predictive of human responses, and cannot justify the harm inflicted on animals or the resultant risks to humans.[33]
Medicines and Healthcare products Regulatory Agency view
The Medicines and Healthcare products Regulatory Agency (MHRA) issued an interim report on the TGN1412 trial on 5 April 2006, followed by a final report on 25 May 2006.[34][35] It found no deficiencies in TeGenero's pre-clinical work and no evidence of undisclosed studies. Parexel's records and processes appeared in order, including dose measurement and administration, and no deficiencies were found that may have led to contamination or overdose. The MHRA felt that their actions did not contribute to the serious adverse events. German regulatory authorities inspected the production of the material by Boehringer Ingelheim, looking at the manufacture, testing, storage and distribution of the TGN1412, but found no deficiencies were identified which could have contributed to the serious adverse effects.
The MHRA concluded that the most likely cause of the reaction in trial subjects was an unpredicted biological action of the drug in humans. The UK Secretary of State for Health agreed to establish a group of leading international experts to consider those issues and to provide a report on the future authorisation of such trials with an interim report at three months, with Gordon Duff, Professor of Molecular Medicine at Sheffield University, as Chair of the group. Until the expert group report, all further clinical trial applications involving first-in-humans trials of any monoclonal antibody or other novel molecules targeting the immune system were not to be authorised in the UK.[36]
In December 2006, the final report of the Expert Group on Phase One Clinical Trials was published.[37] It found that the trial had not considered what constituted a safe dose in humans, and that then-current law had not required it. It made 22 recommendations, including the need for independent expert advice before a high-risk study was allowed, testing only one volunteer at a time (sequential inclusion of participants) in case there were rapid ill effects, and administering drugs slowly by infusion rather than as an injection.[38]
Follow up publications
The trial has become subject of several academic publications:
In 2007, immunologists from the Paul Ehrlich Institute, the German Federal Agency for Sera and Vaccines, reviewed Germany's regulatory requirements in the aftermath of the TGN1412 trial. They suggested that the predictive value of pre-clinical animal models required reevaluation, dose fixing needed refinement or redesign, and criteria for high-risk antibodies needed to be established. Additionally, they suggested that pre-Phase I studies were needed to calculate a dose with a pre-clinical "No effect" level, rather than a No-observed-adverse-effect level.[39]
In 2009, the UK National Institute for Biological Standards and Control wrote that a near-maximum immuno-stimulatory dose had been given, because a safe starting dose in man had been calculated "based upon results from pre-clinical safety testing in a non-responsive species" (Macaca fascicularis). It reported that the European guidelines for first-in-man phase-I clinical trials of biologics had been revised.[40]
In 2010, the failure to predict a severe cytokine release syndrome in humans was explained. In vitro data revealed that the CD4+ effector memory T-cells of Macaca fascicularis, the species of primate used for pre-clinical safety testing of TGN1412, lack CD28 expression. Since CD28 is the target of the TGN1412 antibody, M. fascicularis effector T-cells could not be stimulated by the drug.[41]
In 2013, it was described that standard pro-inflammatory markers TNFα and IL-8 are not predictive of the unusual pro-inflammatory response to TGN1412, and gave a false negative result. IL-2 release and lymphoproliferation are more helpful predictors of the response.[42]
See also
References
- Goldacre, Ben. Bad Pharma. Fourth Estate, 2012, pp. 8–10, 104–105.
- "Exclusive: Drug that caused 'elephant man' side effect makes". Reuters. 24 March 2015.
- https://clinicaltrials.gov/ct2/show/study/NCT01990157
- TeGenero (20 February 2006). "Drug Development". TeGenero. Archived from the original on 12 April 2006. Retrieved 16 March 2006.
- Lin CH, Kerkau T, Guntermann C, Trischler M, Beyersdorf N, Scheuring Y, Tony HP, Kneitz C, Wilhelm M, Mueller P, Huenig T (16 November 2004). "Superagonistic Anti-CD28 Antibody TGN1412 as a Potential Immunotherapeutic for the Treatment of B Cell Chronic Lymphocytic Leukemia". Blood (ASH Annual Meeting Abstracts). 104 (11): Abstract 2519.
- Andy Coghlan (14 August 2006). "Mystery over drug trial debacle deepens". New Scientist. Retrieved 14 August 2006.
- Fleming, Nic (12 April 2008). "Study claims to solve drug trial mystery". The Daily Telegraph. London. Retrieved 25 May 2010.
- Mirenda V, Jarmin SJ, David R, Dyson J, Scott D, Gu Y, et al. (April 2007). "Physiologic and aberrant regulation of memory T-cell trafficking by the costimulatory molecule CD28". Blood. 109 (7): 2968–77. doi:10.1182/blood-2006-10-050724. PMID 17119120.
- "TeGenero AG receives EU-orphan drug designation for Humanized Agonistic Anti-CD28 Monoclonal Antibody TGN1412 for the treatment of B-cell Chronic Lymphocytic Leukaemia, B-CLL" (PDF) (Press release). TeGenero. 13 March 2005. Archived from the original (PDF) on 19 March 2006.
- "Boehringer Ingelheim and TeGenero sign agreement to develop and manufacture CD28-SuperMAB" (PDF) (Press release). TeGenero. 17 November 2003. Archived from the original (PDF) on 18 March 2006.
- Investigator's Brochure, Circare.org, 19 December 2005
- Lühder F, Huang Y, Dennehy KM, Guntermann C, Müller I, Winkler E, et al. (April 2003). "Topological requirements and signaling properties of T cell-activating, anti-CD28 antibody superagonists". The Journal of Experimental Medicine. 197 (8): 955–66. doi:10.1084/jem.20021024. PMC 2193880. PMID 12707299.
- Pillai V, Ortega SB, Wang CK, Karandikar NJ (April 2007). "Transient regulatory T-cells: a state attained by all activated human T-cells". Clinical Immunology. 123 (1): 18–29. doi:10.1016/j.clim.2006.10.014. PMC 1868523. PMID 17185041.
- Woerly G, Roger N, Loiseau S, Dombrowicz D, Capron A, Capron M (August 1999). "Expression of CD28 and CD86 by human eosinophils and role in the secretion of type 1 cytokines (interleukin 2 and interferon gamma): inhibition by immunoglobulin a complexes". The Journal of Experimental Medicine. 190 (4): 487–95. doi:10.1084/jem.190.4.487. PMC 2195599. PMID 10449520.
- Woerly G, Lacy P, Younes AB, Roger N, Loiseau S, Moqbel R, Capron M (October 2002). "Human eosinophils express and release IL-13 following CD28-dependent activation". Journal of Leukocyte Biology. 72 (4): 769–79. doi:10.1189/jlb.72.4.769 (inactive 6 December 2019). PMID 12377947.
- "Investigations into adverse incidents during clinical trials of TGN1412". MHRA. Archived from the original on 21 August 2007.
- Daniel V, Melk A, Süsal C, Weimer R, Zimmermann R, Huth-Kühne A, Opelz G (March 1999). "CD4 depletion in HIV-infected haemophilia patients is associated with rapid clearance of immune complex-coated CD4+ lymphocytes". Clinical and Experimental Immunology. 115 (3): 477–84. doi:10.1046/j.1365-2249.1999.00848.x. PMC 1905242. PMID 10193421.
- "Media Advisory: PAREXEL International Statement Regarding TeGenero AG Phase I Trial at Northwick Park Hospital, UK" (Press release). PAREXEL. 13 March 2006.
- Suntharalingam G, Perry MR, Ward S, et al., Cytokine Storm in a Phase 1 Trial of the Anti-CD28 Monoclonal Antibody TGN1412, New England Journal of Medicine 7 September 2006, vol.355, p.1018–1028.
- "Drugs trial men 'are improving'". BBC News. 18 March 2006. Retrieved 18 March 2006.
- Palmer, Kate (15 October 2014). "Would you accept £3,750 to trial one drug?".
- Press releases by North West London Hospitals NHS Trust, 5 July 2006
- United States patent application US20060009382 filed by Thomas Hanke, Chia-Huey Lin
- Lisa Urquhart; Andrew Jack (16 March 2006). "Data for botched drugs trial show 'nothing' amiss". Financial Times. Retrieved 17 March 2006.
- Patricia Reaney (19 March 2006). "Protein differences may explain drug reaction". Reuters. Archived from the original on 31 December 2005. Retrieved 19 March 2006.
- Waibler Z, Sender LY, Kamp C, Müller-Berghaus J, Liedert B, Schneider CK, et al. (November 2008). "Toward experimental assessment of receptor occupancy: TGN1412 revisited". The Journal of Allergy and Clinical Immunology. 122 (5): 890–2. doi:10.1016/j.jaci.2008.07.049. PMID 18805577.
- Shaoni Bhattacharya; Andy Coghlan (17 March 2006). "Catastrophic immune response may have caused drug trial horror". New Scientist. Retrieved 19 March 2006.
- Celia Hall (17 March 2006). "Antibody 'puts immune system in overdrive'". Telegraph. London. Retrieved 19 March 2006.
- "Trial drug affected animal glands". BBC News. 20 March 2006. Retrieved 20 March 2006.
- "Update to frequently asked questions regarding TGN1412". TeGenero. 19 March 2006. Archived from the original on 21 May 2006. Retrieved 20 March 2006.
- Helen Pearson (17 March 2006). "Tragic drug trial spotlights potent molecule". Nature. Retrieved 19 March 2006.
- Working Party on Statistical Issues in First-in-Man Studies (2007). "Statistical issues in first-in-man studies". Journal of the Royal Statistical Society. 170A: 517–579. Archived from the original on 5 January 2012.
- Akhtar A (October 2015). "The flaws and human harms of animal experimentation". Cambridge Quarterly of Healthcare Ethics. 24 (4): 407–19. doi:10.1017/S0963180115000079. PMC 4594046. PMID 26364776.
- MHRA (5 April 2006). "Press release: Latest findings on clinical trial suspension". Press Release. Archived from the original on 5 December 2014. Retrieved 4 June 2010.
- Medicines and Healthcare Products Regulatory Agency (MHRA) (25 May 2006). "Clinical trial final report". webarchive.nationalarchives.gov.uk. Archived from the original on 6 December 2014. Retrieved 29 November 2017.CS1 maint: BOT: original-url status unknown (link)
- INVESTIGATIONS INTO ADVERSE INCIDENTS DURING CLINICAL TRIALS OF TGN1412 Medicines and Healthcare products Regulatory Agency (MHRA), 6pp, 5 April 2006.
- Expert Group on Phase One Clinical Trials: Final report TSO (The Stationery Office)7 December 2006.
- Aboulghar MA, Mansour RT, Serour GI (October 1990). "Transvaginal injection of potassium chloride and methotrexate for the treatment of tubal pregnancy with a live fetus". Human Reproduction. 5 (7): 887–8. doi:10.1136/bmj.39062.336157.DB. PMC 1702450.
- Liedert B, Bassus S, Schneider CK, Kalinke U, Löwer J (January 2007). "Safety of phase I clinical trials with monoclonal antibodies in Germany--the regulatory requirements viewed in the aftermath of the TGN1412 disaster". International Journal of Clinical Pharmacology and Therapeutics. 45 (1): 1–9. doi:10.5414/CPP45001. PMID 17256444.
- Stebbings R, Poole S, Thorpe R (December 2009). "Safety of biologics, lessons learnt from TGN1412". Current Opinion in Biotechnology. 20 (6): 673–7. doi:10.1016/j.copbio.2009.10.002. PMID 19892543.
- Eastwood D, Findlay L, Poole S, Bird C, Wadhwa M, Moore M, et al. (October 2010). "Monoclonal antibody TGN1412 trial failure explained by species differences in CD28 expression on CD4+ effector memory T-cells". British Journal of Pharmacology. 161 (3): 512–26. doi:10.1111/j.1476-5381.2010.00922.x. PMC 2990151. PMID 20880392.
- Stebbings R, Eastwood D, Poole S, Thorpe R (2013). "After TGN1412: recent developments in cytokine release assays". Journal of Immunotoxicology. 10 (1): 75–82. doi:10.3109/1547691X.2012.711783. PMC 3541671. PMID 22967038.
External links
- Report in Nature on TGN1412
- BBC News: Drug trial man 'may lose fingers'
- BBC News: Regulators slam drug trial firm
- Channel 4: The Drug Trial That Went Wrong
- Nature news: Animal tests may have missed danger because monkeys 'too clean'
- crisis communications case study of Tegenero clinical trial
- Further lessons from the TGN1412 tragedy