Spermatic cord
The spermatic cord is the cord-like structure in males formed by the vas deferens (ductus deferens) and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum during its descent it carries along with it vas deferens, its vessels, nerves etc. There is one on each side.
| Spermatic cord | |
|---|---|
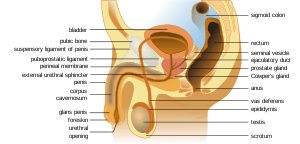 Anatomy of the human male reproductive system | |
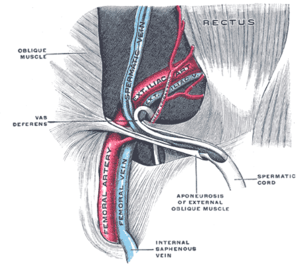 The spermatic cord in the inguinal canal (label for spermatic cord in lower right) | |
| Details | |
| Identifiers | |
| Latin | Funiculus spermaticus |
| MeSH | D013085 |
| FMA | 19937 |
| Anatomical terminology | |
Structure
The spermatic cord is ensheathed in three layers of tissue:
- external spermatic fascia, an extension of the innominate fascia that overlies the aponeurosis of the external oblique muscle
- cremasteric muscle and fascia, formed from a continuation of the internal oblique muscle and its fascia
- internal spermatic fascia, continuous with the transversalis fascia
The normal diameter of the spermatic cord is about 16 mm (range 11 to 22 mm).[1]
Function
Contents
- Arteries: testicular artery, Artery of the ductus deferens, cremasteric artery
- Nerves: nerve to cremaster (genital branch of the genitofemoral nerve) and testicular nerves (sympathetic nerves). It is worth noting that the ilio-inguinal nerve is not actually located inside the spermatic cord, but runs along the outside of it, in the inguinal canal.
- Vas deferens (ductus deferens)
- Pampiniform plexus
- Lymphatic vessels
- Tunica vaginalis (remains of the processus vaginalis)
The pampiniform plexus, testicular artery, cremasteric artery, artery of the ductus deferens, lymphatic vessels, testicular sympathetic nerves, and ductus deferens all run deep to the internal spermatic fascia.[2] The ilioinguinal nerve runs on the superficial surface of the external spermatic fascia.
Clinical significance
The spermatic cord is sensitive to torsion, in which the testicle rotates within its sac and blocks its own blood supply. Testicular torsion may result in irreversible damage to the testicle within hours. A collection of serous fluid in the spermatic cord is named 'funiculocele'.
The contents of the abdominal cavity may protrude into the inguinal canal, producing an indirect inguinal hernia.
Varicose veins of the spermatic cord are referred to as varicocele. Though often asymptomatic, about one in four people with varicocele have negatively affected fertility.[3]
Additional images
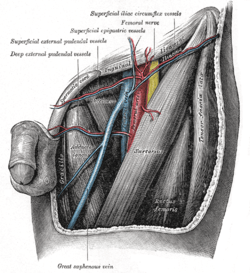 The left femoral triangle
The left femoral triangle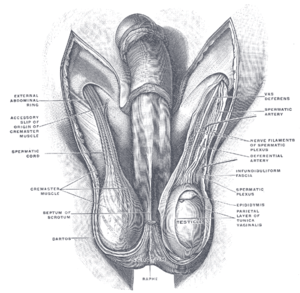 The scrotum.
The scrotum.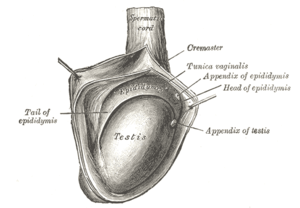 The right testis, exposed by laying open the tunica vaginalis
The right testis, exposed by laying open the tunica vaginalis Spermatic cord
Spermatic cord- Spermatic cord
- Superficial veins oflower limb.Superficial dissection.Anterior view.
References
- Firoozabadi R, Stafford P, Routt M (2015). "Risk of Spermatic Cord Injury During Anterior Pelvic Ring and Acetabular Surgery: An Anatomical Study". Arch Bone Jt Surg. 3 (4): 269–73. PMC 4628634. PMID 26550592.
- Shadbolt, Clair; Stefan B. J. Heinze; Rosalind B. Dietrich (2001). "Imaging of Groin Masses: Inguinal Anatomy and Pathologic Conditions Revisited". RadioGraphics. doi:10.1148/radiographics.21.suppl_1.g01oc17s261. Cite journal requires
|journal=(help) Figure 3. - "Learn About Varicocele Treatment". VARICOCELE HEALING. Archived from the original on 2 February 2014. Retrieved 25 April 2018.
External links
- Anatomy figure: 36:01-00 at Human Anatomy Online, SUNY Downstate Medical Center - "The inguinal canal and derivation of the layers of the spermatic cord."
- Anatomy image:7509 at the SUNY Downstate Medical Center
- Cross section image: pembody/body18b—Plastination Laboratory at the Medical University of Vienna
- Cross section image: pelvis/pelvis-e12-15—Plastination Laboratory at the Medical University of Vienna
- inguinalregion at The Anatomy Lesson by Wesley Norman (Georgetown University) (spermaticcord)