Sialoblastoma
A sialoblastoma is a low-grade salivary gland neoplasm that recapitulates primitive salivary gland anlage. It has previously been referred to as congenital basal cell adenoma, embryoma, or basaloid adenocarcinoma. It is an extremely rare tumor, with less than 100 cases reported worldwide.[1][2][3][4]
Signs and symptoms
The majority of the tumors are identified in the parotid salivary gland, although the submandibular gland can also be affected. The symptoms are non-specific, but include a mass, frequently rapidly expanding, or ulceration of the skin overlying the mass.[5] In very rare instances, association with other tumors, such as nevus sebaceus and hepatoblastoma are documented.[6] Ultrasound can be used to screen the mass, a technique which can even be performed prenatally. MRI can also be used, but the findings are non-specific.[1][7]
Pathology Findings
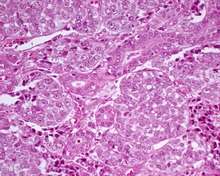
The tumors are multinodular or lobular, sometimes showing areas of necrosis or hemorrhage. They range in size from 2–7 cm. As would be expected, the histologic features under the microscope are similar to what would be seen in embryologic development at about the third month. There are two major patterns.
- Favorable pattern: partially encapsulated with bland basaloid cells and intervening stroma.
- Unfavorable pattern: Infiltrating borders with perineural or perivascular invasion.
Both patterns have basaloid cells arranged in solid nests, nodules or trabecula, with focal peripheral palisading. The nuclei are round to oval with delicate chromatin and a usually single nucleolus. Ductules can sometimes be seen. The background stroma is loose, immature and sometimes myxoid. Necrosis can be present. Mitotic figures are often easy to find.[2][5][8][9] Tumor cells can be tested by immunohistochemistry which shows: Ductal cells: positive with keratins, CK7 and CK19. Basaloid or myoepithelial cells: positive with S100 protein, muscle specific actin, calponin and p63.[2][5][8] The proliferation marker, Ki-67, may show increased labelling, and when it does, it is associated with an unfavorable outcome.[10]
Diagnosis
It is important that other tumors such as pleomorphic adenoma, basal cell adenoma, adenoid cystic carcinoma, and teratoma be excluded before treatment is started.[6][9][11]
Management
Treatment includes complete surgical excision. If the tumor cannot be completely removed, then chemotherapy can be considered. However, chemotherapy may have long term adverse outcomes for patients who are usually very young.[12][13][14]
Epidemiology
Most patients are younger than two years, with the majority presenting during the neonatal period. Boys are affected slightly more often than girls (1.2:1).[8]
References
- Som PM, Brandwein M, Silvers AR, Rothschild MA (1997). "Sialoblastoma (embryoma): MR findings of a rare pediatric salivary gland tumor". AJNR Am J Neuroradiol. 18 (5): 847–50. PMID 9159361.
- Dehner LP, Valbuena L, Perez-Atayde A, Reddick RL, Askin FB, Rosai J (Jan 1994). "Salivary gland anlage tumor ("congenital pleomorphic adenoma"). A clinicopathologic, immunohistochemical and ultrastructural study of nine cases". Am J Surg Pathol. 18 (1): 25–36. doi:10.1097/00000478-199401000-00003. PMID 8279626.
- Batsakis JG, Frankenthaler R (Nov 1992). "Embryoma (sialoblastoma) of salivary glands". Ann Otol Rhinol Laryngol. 101 (11): 958–60. doi:10.1177/000348949210101115. PMID 1444105.
- Taylor, G. P. (1988). "Congenital epithelial tumor of the parotid-sialoblastoma". Pediatric Pathology. 8 (4): 447–452. doi:10.3109/15513818809041583. PMID 3211816.
- Brandwein M, Al-Naeif NS, Manwani D, Som P, Goldfeder L, Rothschild M, Granowetter L (Mar 1999). "Sialoblastoma: clinicopathological/immunohistochemical study". Am J Surg Pathol. 23 (3): 342–8. doi:10.1097/00000478-199903000-00015. PMID 10078927.
- Seifert, G.; Donath, K. (1997). "The congenital basal cell adenoma of salivary glands. Contribution to the differential diagnosis of congenital salivary gland tumours". Virchows Archiv. 430 (4): 311–319. doi:10.1007/bf01092754. PMID 9134042.
- Yekeler, E.; Dursun, M.; Gun, F.; Kilincaslan, H.; Ucar, A.; Genchellac, H.; Acunas, G. (2004). "Sialoblastoma: MRI findings". Pediatric Radiology. 34 (12): 1005–1007. doi:10.1007/s00247-004-1286-5. PMID 15278323.
- Williams SB, Ellis GL, Warnock GR (Dec 2006). "Sialoblastoma: a clinicopathologic and immunohistochemical study of 7 cases". Ann Diagn Pathol. 10 (6): 320–6. doi:10.1016/j.anndiagpath.2006.02.008. PMID 17126248.
- Herrmann BW, Dehner LP, Lieu JE (Feb 2005). "Congenital salivary gland anlage tumor: a case series and review of the literature". Int J Pediatr Otorhinolaryngol. 69 (2): 149–56. doi:10.1016/j.ijporl.2004.08.014. PMID 15656947.
- Patil, D. T.; Chou, P. M. (2010). "Sialoblastoma: Utility of Ki-67 and p53 as a Prognostic Tool and Review of Literature". Pediatric and Developmental Pathology. 13 (1): 32–38. doi:10.2350/09-05-0650-OA.1. PMID 20001735.
- Dardick, I.; Daley, T. D.; McComb, R. J. (2010). "Sialoblastoma in adults: Distinction from adenoid cystic carcinoma". Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 109 (1): 109–116. doi:10.1016/j.tripleo.2009.07.049. PMID 19880331.
- Mertens, F.; Wahlberg, P.; Domanski, H. A. (2009). "Clonal chromosome aberrations in a sialoblastoma". Cancer Genetics and Cytogenetics. 189 (1): 68–69. doi:10.1016/j.cancergencyto.2008.10.005. PMID 19167616.
- Scott, J. X.; Krishnan, S.; Bourne, A. J.; Williams, M. P.; Agzarian, M.; Revesz, T. (2008). "Treatment of metastatic sialoblastoma with chemotherapy and surgery". Pediatric Blood & Cancer. 50 (1): 134–137. doi:10.1002/pbc.20788. PMID 16514617.
- Mostafapour, S. P.; Folz, B.; Barlow, D.; Manning, S. (2000). "Sialoblastoma of the submandibular gland: Report of a case and review of the literature". International Journal of Pediatric Otorhinolaryngology. 53 (2): 157–161. doi:10.1016/s0165-5876(00)00311-6. PMID 10906522.
Further reading
Lester D. R. Thompson; Bruce M Wenig (2011). Diagnostic Pathology: Head and Neck: Published by Amirsys. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 5:152–155. ISBN 978-1-931884-61-7.