Scheuermann's disease
Scheuermann's disease is a self-limiting skeletal disorder of childhood. Scheuermann's disease describes a condition where the vertebrae grow unevenly with respect to the sagittal plane; that is, the posterior angle is often greater than the anterior. This uneven growth results in the signature "wedging" shape of the vertebrae, causing kyphosis. It is named after Danish surgeon Holger Scheuermann.[1][2][3]
| Scheuermann's disease | |
|---|---|
| Other names | Scheuermann's kyphosis, Calvé disease, idiopathic juvenile kyphosis of the spine |
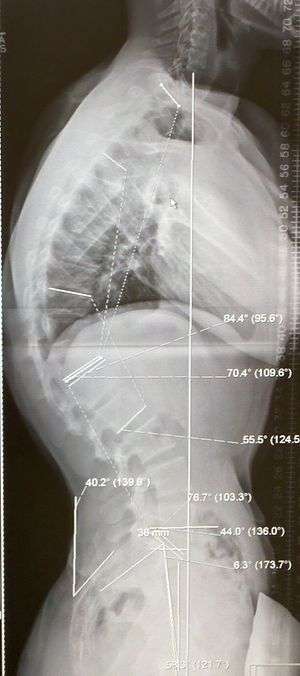 | |
| A 20-year-old male with Scheuermann's disease, showing various measurement of kyphotic/lordotic degrees and their supplementary angles. Notice the signature 'wedging' shape of the four vertebrae in the lower thoracic area. The other vertebral bodies are otherwise normal. The measured kyphosis for this patient is ~70°. | |
| Pronunciation |
|
Signs and symptoms
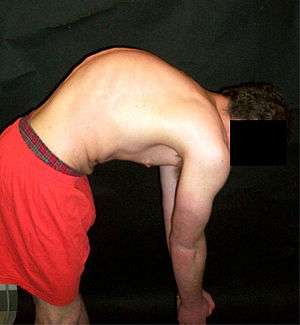
Scheuermann's disease is considered to be a form of juvenile osteochondrosis of the spine. It is found mostly in teenagers and presents a significantly worse deformity than postural kyphosis. Patients suffering with Scheuermann’s kyphosis cannot consciously correct their posture. The apex of their curve, located in the thoracic vertebrae, is quite rigid.
Scheuermann's disease is notorious for causing lower and mid-level back and neck pain, which can be severe and disabling. The sufferer may feel pain at the apex of the curve, which is aggravated by physical activity and by periods of standing or sitting; this can have a significantly detrimental effect to their lives as their level of activity is curbed by their disability. The sufferer may feel isolated or uneasy amongst their peers if they are children, depending on the level of deformity.
In addition to the pain associated with Scheuermann's disease, many sufferers of the disorder have loss of vertebral height, and depending on where the apex of the curve is, may have a visual 'hunchback' or 'roundback'. It has been reported that curves in the lower thoracic region cause more pain, whereas curves in the upper region present a more visual deformity. Nevertheless, it is typically pain or cosmetic reasons that prompt sufferers to seek help for their condition. In studies, kyphosis is better characterized for the thoracic spine than for the lumbar spine.[4][5]
The seventh and tenth thoracic vertebrae are most commonly affected. It causes backache and spinal curvature. In very serious cases it may cause internal problems and spinal cord damage, but these cases are extremely rare. The curvature of the back decreases height, thus putting pressure on internal organs, wearing them out more quickly than the natural aging process; surgical procedures are almost always recommended in this case.
Associated conditions
Many with Scheuermann's disease often have an excessive lordotic curve in the lumbar spine; this is the body's natural way to compensate for the kyphotic curve above. Many with Scheuermann's disease have very large lung capacities and males often have broad, barrel chests. Most people have forced vital capacity (FVC) scores above average. It has been proposed that this is the body's natural way to compensate for a loss of breathing depth.
Often patients have tight hamstrings, which, again, is related to the body compensating for excessive spinal curvature, though this is also debated (for example, some suggest the tightness of ligament is the initial cause of the growth abnormality). In addition to the common lordosis, it has been suggested that between 20–30% of patients with Scheuermann's Disease also have scoliosis, though most cases are negligible. In more serious cases, however, the combination is classified as a separate condition known as kyphoscoliosis.
Causes
The cause is not currently known, and the condition appears to be multifactorial.[6] Several candidate genes (such as FBN1, which has been associated with Marfan) have been proposed and excluded.[7]
Diagnosis
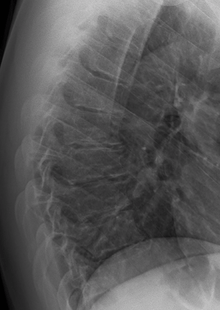

Diagnosis is typically by medical imaging. The degree of kyphosis can be measured by Cobb's angle and sagittal balance.
Treatment
Conservative
Scheuermann's disease is self-limiting after growth is complete, meaning that it generally runs its course and never presents further complication. Typically, however, once the patient is fully grown, the bones will maintain the deformity. For this reason, there are many treatment methods and options available that aim to correct the kyphosis while the spine is still growing, and especially aim to prevent it from worsening.
While there is no explanation for what causes Scheuermann's Disease, there are ways to treat it. For decades there has been a lot of controversy surrounding treatment options. For less extreme cases, manual medicine, physical therapy and/or back braces can help reverse or stop the kyphosis before it does become severe. Because the disease is often benign, and because back surgery includes many risks, surgery is usually considered a last resort for patients. In severe or extreme cases, patients may be treated through an extensive surgical procedure in an effort to prevent the disease from worsening or harming the body.
In Germany, a standard treatment for both Scheuermann's disease and lumbar kyphosis is the Schroth method, a system of specialized physical therapy for scoliosis and related spinal deformities.[8] The method has been shown to reduce pain and decrease kyphotic angle significantly during an inpatient treatment program.[9][10]
Surgery

Scheuermann's disease can be successfully corrected with surgical procedures, almost all of which include spinal fusion and hardware instrumentation, i.e., rods, pedicle screws, etc. While many patients are typically interested in getting surgery for their correction, it is important to realize the surgery aims to reduce pain, and not cosmetic defect. As always, surgical intervention should be used as a last resort once conservative treatment fails or the patient's health is in imminent danger as any surgical procedure is not without risk; however, the chances of complication are relatively low and the surgeries are often successful.
One of the largest debates surrounding Scheuermann's disease's correction is the use of very different correction procedures. There are different techniques to correct kyphosis; usually the differences being posterior/anterior entry or posterior entry (rear) only. The classic surgical procedure partially entails entering two titanium rods, each roughly one and a half feet long (depending on the size of the khyphosis), into the back on either side of the spine. Eight titanium screws and hardware are drilled through the bone and secure the rods onto either side of the spine. On the internal-facing side of the spine, ligaments (which can be too short, pulling the spine into the general shape of kyphosis) must be surgically cut or released, not only stopping part of the cause of the kyphosis, but also allowing the titanium rods to pull the spine into a more natural position. Normally, the damaged discs between the troubled vertebrae (wedged vertebrae) are removed and replaced with bone grafting from the hip or other parts of the vertebrae, which once healed or 'fused' will solidify. The titanium instrumentation holds everything in place during healing and is not necessary once fusion completes. Recovery begins in the hospital and depending on whether the operation is one- or two-stage the patient can expect to be in hospital for minimum of a week, possibly longer depending on recovery. They will then often be required to wear a brace for several months to ensure the spine heals correctly leaving the patient with the correct posture. The titanium instrumentation can stay in the body permanently, or be removed years later. Patients undergoing surgery for Scheuermann's disease often need physical therapy to manage pain and mobility, however their range of motion is generally not limited very much. Recovery from kyphosis correction surgery can be very long; typically patients are not allowed to lift anything above 5 or 10 pounds for 6 months to a year. Many are out of work for at least 6 months. However, once the fusion is solidified, most patients can return to their usual lifestyle within one to two years.
Prognosis
Spinal fusion for kyphosis and scoliosis is an extremely invasive surgery. The risk of complications is estimated to be about 10%. Possible complications may be inflammation of the soft tissue or deep inflammatory processes, breathing impairments, bleeding and nerve injuries, or infection. As early as five years after surgery around 5% require reoperation and long-term issues remain unclear.[11][12] Taking into account that some of the symptoms of the spinal deformity cannot be changed by surgical intervention, surgery remains a cosmetic indication,[11][13] though the cosmetic effects of surgery are not necessarily stable.[11]
Notable cases
References
- synd/3305 at Who Named It?
- Scheuermann, H. W. (1920). "Kyphosis dorsalis juvenilis". Ugeskrift for Læger (in Danish). 82: 385–93. Republished as: Scheuermann, H. W. (1977). "The classic: Kyphosis dorsalis juvenilis". Clinical Orthopaedics and Related Research. 128 (128): 5–7. PMID 340099.
- "Scheuermann's disease". Medcyclopaedia. GE. Archived from the original on 2012-05-24.
- Summers, B N; Singh, J P; Manns, R A (2008). "The radiological reporting of lumbar Scheuermann's disease: An unnecessary source of confusion amongst clinicians and patients". The British Journal of Radiology. 81 (965): 383–5. doi:10.1259/bjr/69495299. PMID 18440942.
- Blumenthal, Scott L.; Roach, James; Herring, J. A. (1987). "Lumbar Scheuermannʼs". Spine. 12 (9): 929–32. doi:10.1097/00007632-198711000-00015. PMID 3441839.
- Fotiadis, E.; Kenanidis, E.; Samoladas, E.; Christodoulou, A.; Akritopoulos, P.; Akritopoulou, K. (2008). "Scheuermann's disease: Focus on weight and height role". European Spine Journal. 17 (5): 673–8. doi:10.1007/s00586-008-0641-x. PMC 2367416. PMID 18301929.
- McKenzie, L; Sillence, D (1992). "Familial Scheuermann disease: A genetic and linkage study". Journal of Medical Genetics. 29 (1): 41–5. doi:10.1136/jmg.29.1.41. PMC 1015820. PMID 1552543.
- Lehnert-Schroth, Christa (2007). Three-Dimensional Treatment for Scoliosis: A Physiotherapeutic Method for Deformities of the Spine. Palo Alto, CA: The Martindale Press. pp. 185–187, 211–17, and passim. ISBN 978-3-8334-8138-3.
- Weiss HR, Dieckmann J, Gerner HJ (2002). "Effect of intensive rehabilitation on pain in patients with Scheuermann's disease". Stud Health Technol Inform. 88: 254–7. PMID 15456045.
- Weiss HR, Dieckmann J, Gerner HJ (2002). "Outcome of in-patient rehabilitation in patients with M. Scheuermann evaluated by surface topography". Stud Health Technol Inform. 88: 246–9. PMID 15456043.
- Hawes, Martha (2006). "Impact of spine surgery on signs and symptoms of spinal deformity". Developmental Neurorehabilitation. 9 (4): 318–39. doi:10.1080/13638490500402264. PMID 17111548.
- Weiss, Hans-Rudolf; Goodall, Deborah (2008). "Rate of complications in scoliosis surgery – a systematic review of the Pub Med literature". Scoliosis. 3: 9. doi:10.1186/1748-7161-3-9. PMC 2525632. PMID 18681956.
- Hawes, Martha C.; O'Brien, Joseph P. (2008). "A century of spine surgery: What can patients expect?". Disability & Rehabilitation. 30 (10): 808–17. doi:10.1080/09638280801889972. PMID 18432439.
- Shinzawa, Fluto (2007-10-18). "Bruins rookie Lucic punches up résumé – The Boston Globe". Boston.com. Retrieved 2010-08-31.
- Rosenthal, Ken (12 October 2014). "There's a good reason why Hunter Pence throws like that". Fox Sports. Retrieved 13 October 2014.
- "One Year On George Sampson". The Times. London. 2009-05-17. Retrieved 2010-05-23.
- Telekom Electronic Beats (3 July 2013). "MARCEL DETTMANN In the car with EB.TV" – via YouTube.
- Robinson, Georgina (17 March 2018). "The secret life of referees featuring Australian Angus Gardner". Sydney Morning Herald. Retrieved 2 April 2018.
External links
| Classification | |
|---|---|
| External resources |
| Wikimedia Commons has media related to Scheuermann's disease. |