Postpartum psychosis
Postpartum psychosis is a rare psychiatric emergency in which symptoms of high mood and racing thoughts (mania), depression, severe confusion, loss of inhibition, paranoia, hallucinations and delusions set in, beginning suddenly in the first two weeks after childbirth. The symptoms vary and can change quickly.[1] The most severe symptoms last from 2 to 12 weeks, and recovery takes 6 months to a year.[1]
| Postpartum psychosis | |
|---|---|
| Other names | puerperal psychosis |
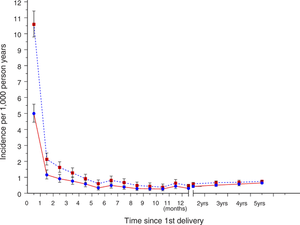 | |
| Rates of psychoses among Swedish first-time mothers | |
| Specialty | Psychiatry |
About half of women who experience it have no risk factors; but women with a prior history of mental illness, like bipolar disorder, a history of prior episodes of postpartum psychosis, or a family history are at a higher risk.[1] It is not a formal diagnosis, but is widely used to describe a condition that appears to occur in about 1 in 1000 pregnancies. It is different from postpartum depression and from maternity blues.[2]
Diagnosis of postpartum psychosis always requires hospitalization, where treatment is antipsychotic medication, mood stabilizers, and, in cases of strong risk for suicide, electroconvulsive therapy.[1] Women who have been hospitalized for a psychiatric condition immediately after delivery are at a much higher risk of suicide during the first year after delivery.[3]
There is a need for further research into the causes and prevention; the lack of a formal diagnostic category and the difficulty of conducting clinical trials in pregnancy hinder research.[1]
Signs and symptoms
Symptoms usually begin suddenly in the first two weeks after delivery,[2] sometimes in the first two to three days after giving birth.[4] Symptoms vary and can change quickly, and can include high mood and racing thoughts (mania), depression, severe confusion, losing inhibitions, paranoia, hallucinations and delusions.[2]
In contrast, about half of women have the maternity blues after birth, which is characterized by symptoms of mild mood swings, anxiety, and irritability that start about 3 to 4 days after delivery and last about a week. It is different from postpartum depression which is experienced in some form by roughly 20% of all women after birth and is similar to major depressive disorder.[2]
Risk factors
Women with a history of bipolar disorder, schizophrenia, prior episode of postpartum psychosis, or a family history of postpartum psychosis are at high risk; about 25-50% of women in this group will have postpartum psychosis.[2] around 37% of women with bipolar disorder have a severe postpartum episode.[5] Women with a prior episode of postpartum psychosis have about a 30% risk of having another episode in the next pregnancy.[5] For a woman with no history of mental illness who has a close relative (a mother or sister) who had postpartum psychosis, the risk is about 3%.[2] There may be a genetic component; while mutations in chromosome 16 and in specific genes involved in serotoninergic, hormonal, and inflammatory pathways have been identified, none had been confirmed as of 2014.[1]
Family history of affective psychosis, prenatal depression, and autoimmune thyroid dysfunction also increase the risk of postpartum psychosis.[6]
About half of women who experience postpartum psychosis had no risk factors.[1] Many other potential factors like pregnancy and delivery complications, caesarean section, sex of the baby, length of pregnancy, changes in psychiatric medication, and psychosocial factors have been researched and no clear association has been found; the only clear risk factor identified as of 2014 was that postpartum psychosis happens more often to women giving birth for the first time, than to women having second or subsequent deliveries, but the reason for that was not known.[1] There may be a role for hormonal changes that occur following delivery, in combination with other factors; there may be a role changes in the immune system as well.[1]
Diagnosis
Classification
Postpartum psychosis is a psychiatric emergency related to care of women after they give birth.[1][2] The first evaluation requires a complete history, physical examination, and laboratory investigations to disbar a biological cause for acute psychosis as well as a careful neurological assessment. [7] It is different from postpartum depression and from maternity blues.[2]
The condition is not recognized in the DSM-5 as a distinct disorder nor in the ICD-10 but it is widely used clinically.[1]
Prevention and screening
For women taking psychiatric medication, the decision as to whether continue during pregnancy and whether to take them while breast feeding is difficult in any case; there is no data to guide this decision with respect to preventing postpartum psychosis.[2] There is no data to guide a decision as to whether women at high risk for postpartum psychosis should take antipsychotic medicine to prevent it.[2] For women at risk of postpartum psychosis, informing medical care-givers, and monitoring by a psychiatrist during pregnancy, in the perinatal period, and for a few weeks following delivery, is recommended.[2]
For women with known bipolar disorder, taking medication during pregnancy roughly halves the risk of a severe postpartum episode, as does starting to take medication immediately after the birth.[5]
Management
In most cases hospital admission is necessary.[2] Antipsychotic drugs and mood stabilizing drugs such as lithium are typically administered[2] but is not clear if mood stabilizers can be titrated to a high enough level quickly enough to be effective.[1] Electroconvulsive therapy may be considered, especially if there is a high risk of suicide.[1]
Family support may be provided via a social worker.[2]
Outcomes
The most severe symptoms usually last from 2 to 12 weeks; it can take between six months and a year to recover.[2]
Women often experience low self-esteem and difficulties as they recover, but many women fully recover; many women also have a hard time bonding with their child as they recover, but end up with healthy relationships with their babies.[2]
About half of women who experience postpartum psychosis have further experiences of mental illness unrelated to childbirth; further pregnancies do not change that risk.[2]
Women hospitalized for a psychiatric illness shortly after giving birth have a 70 times greater risk of suicide in the first 12 months following delivery.[3]
Treatments
In the treatment of postpartum psychosis there are no official guidelines. Once tests are administered and all the proper medical causes have been excluded from the diagnosis then the proper treatment is given based on the symptoms.[8] Before the mother is released from the hospital, the team that administered treatment must work with the mother and her family to form a discharge plan that will strengthen her support, along with close follow-up, and prevent stressors that will risk the mother relapsing. Also, for future pregnancies, the mother's primary care provider is advised to work jointly with other specialists on her care team giving her care in thought of antimanic prophylaxis during pregnancy or after childbirth.[9]
History
Postpartum Psychosis is the most severe form of all the postpartum psychiatric disorders. It is a rare disease that only occurs within 1 out of 1,000 women after birthing a child. The symptoms occur within 48 to 72 hours after childbirth while showcasing dramatic effects. Some of the premature signs are restlessness, irritability, and insomnia[10]. Puerperal mania was clearly described by the German obstetrician Friedrich Benjamin Osiander in 1797,[11] and a literature of over 2,000 works has accumulated since then.
The French psychiatrist Louis-Victor Marcé (1862) suggested that the menstrual cycle is important and drew parallels with menstrual psychosis.[12]
Episodes of postpartum psychosis used to be explained by eclampsia, "delirium", thyroid disorders, or infection.[1]
Society and culture
Support
In the UK, a series of workshops called "Unravelling Eve" were held in 2011, where women who had experienced postpartum depression shared their stories.[13]
Notable cases
- Harriet Sarah, Lady Mordaunt (1848–1906), formerly Harriet Moncreiffe, was the Scottish wife of an English baronet and Member of Parliament, Sir Charles Mordaunt.[14] She was the defendant in a sensational divorce case in which the Prince of Wales (later King Edward VII) was embroiled; after a controversial trial lasting seven days, the jury determined that Lady Mordaunt was suffering from “puerperal mania” and her husband's petition for divorce was dismissed, while Lady Mordaunt was committed to an asylum.[15]:36–37
- Stacey Slater, a fictional character in the long-running BBC soap-opera EastEnders suffered from postpartum psychosis in 2016, and was one of the show's biggest storylines that year.
Legal status
Several nations including Canada, Great Britain, Australia, and Italy recognize postpartum mental illness as a mitigating factor in cases where mothers kill their children.[16] In the United States, such a legal distinction was not made as of 2009.[16] In the US, an insanity defense is not available in all states.[17] Britain has had the Infanticide Act since 1922.
Research directions
The lack of a formal diagnosis in the DSM and ICD has hindered research.[1] The causes of postpartum depression are unknown and are under investigation.[1][2]
There is a need to better understand whether taking medication for prevention during pregnancy or immediately following birth, is useful.[5]
See also
- Psychiatric disorders of childbirth
- Charlotte Perkins Gilman
- Andrea Yates
- Menstrual psychosis
References
- Jones, I; Chandra, PS; Dazzan, P; Howard, LM (15 November 2014). "Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period". Lancet. 384 (9956): 1789–99. doi:10.1016/S0140-6736(14)61278-2. PMID 25455249.
- "Postpartum Psychosis". Royal College of Psychiatrists. 2014. Retrieved 27 October 2016.
- Orsolini, L; et al. (12 August 2016). "Suicide during Perinatal Period: Epidemiology, Risk Factors, and Clinical Correlates". Frontiers in Psychiatry. 7: 138. doi:10.3389/fpsyt.2016.00138. PMC 4981602. PMID 27570512.
- Sharma, Indira; Rai, Shashi; Pathak, Abhishek (2015). "Postpartum psychiatric disorders: Early diagnosis and management". Indian Journal of Psychiatry. 57 (6): 216–221. doi:10.4103/0019-5545.161481. PMC 4539865. PMID 26330638.
- Wesseloo, R; Kamperman, AM; Munk-Olsen, T; Pop, VJ; Kushner, SA; Bergink, V (1 February 2016). "Risk of Postpartum Relapse in Bipolar Disorder and Postpartum Psychosis: A Systematic Review and Meta-Analysis". American Journal of Psychiatry. 173 (2): 117–27. doi:10.1176/appi.ajp.2015.15010124. PMID 26514657.
- Essali, A.; Alabed, S.; Guul, A.; Essali, N. (20 May 2013). "Preventive Interventions for Postnatal Psychosis". Schizophrenia Bulletin. 39 (4): 748–750. doi:10.1093/schbul/sbt073. PMC 3686463. PMID 23690649.
- Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894. "National Center for Biotechnology Information". www.ncbi.nlm.nih.gov. Retrieved 2019-04-08.
- Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894. "National Center for Biotechnology Information". www.ncbi.nlm.nih.gov. Retrieved 2019-04-09.
- Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894. "National Center for Biotechnology Information". www.ncbi.nlm.nih.gov. Retrieved 2019-04-09.
- "Center for Women's Mental Health at MGH". MGH Center for Women's Mental Health. Retrieved 2019-04-09.
- Osiander, Friedrich Benjamin (1797). "Glücklich gehobenes hitziges Fieber einer Wöchnerin mit Wahnsinn" [Happy young mother with a violent fever upscale madness]. Neue Denkwuerdigkeiten fuer Aerzte und Geburtshelfer [New memoirs for physicians and obstetricians] (in German). 1. Goettingen: Rosenbusch. pp. 52–128.
- Marcé, L V (1862). Traité Pratique des Maladies Mentales [Practical Treatise on Mental Illness] (in French). Paris: Martinet. p. 146.
- Dolman, Clare (4 December 2011). "When having a baby can cause you to 'lose your mind'". BBC News.
- "Person Page: Harriett Sarah Moncreiffe". thepeerage.com. Retrieved 27 October 2016.
- Souhami, Diana (1996). Mrs. Keppel and her daughter (1st U.S. ed.). New York: St. Martin's Press. ISBN 978-0312155940. E-book ISBN 9781466883505
- Appel, Jacob M. (8 November 2009). "When Infanticide Isn't Murder". The Huffington Post.
- Rhodes, Ann M.; Segre, Lisa S. (6 June 2013). "Perinatal depression: a review of US legislation and law". Archives of Women's Mental Health. 16 (4): 259–270. doi:10.1007/s00737-013-0359-6. PMC 3725295. PMID 23740222.
Further reading
- Twomey, Teresa (2009). Understanding Postpartum Psychosis: A Temporary Madness. Westport, CT: Praeger. ISBN 978-0-313-35346-8.