Postpartum bleeding
Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood within the first 24 hours following childbirth.[2] Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist.[6] Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breath rate.[1] As more blood is lost, the woman may feel cold, blood pressure may drop, and she may become restless or unconscious.[1] The condition can occur up to six weeks following delivery.[6]
| Postpartum bleeding | |
|---|---|
| Other names | Postpartum hemorrhage |
 | |
| A non-pneumatic anti-shock garment (NASG) | |
| Specialty | Obstetrics |
| Symptoms | Loss of lots of blood after childbirth, increased heart rate, feeling faint upon standing, increased breath rate[1][2] |
| Causes | Poor contraction of the uterus, not all the placenta removed, tear of the uterus, poor blood clotting[2] |
| Risk factors | Anemia, Asian ethnicity, more than one baby, obesity, age older than 40 years[2] |
| Prevention | Oxytocin, misoprostol[2] |
| Treatment | Intravenous fluids, non-pneumatic anti-shock garment, blood transfusions, ergotamine, tranexamic acid[2][3] |
| Prognosis | 3% risk of death (developing world)[2] |
| Frequency | 8.7 million (global)[4] / 1.2% of births (developing world)[2] |
| Deaths | 83,100 (2015)[5] |
The most common cause is poor contraction of the uterus following childbirth.[2] Not all of the placenta being delivered, a tear of the uterus, or poor blood clotting are other possible causes.[2] It occurs more commonly in those who: already have a low amount of red blood, are Asian, with bigger or more than one baby, are obese or are older than 40 years of age.[2] It also occurs more commonly following caesarean sections, those in whom medications are used to start labor, those requiring the use of a vacuum or forceps, and those who have an episiotomy.[2][7]
Prevention involves decreasing known risk factors including procedures associated with the condition, if possible, and giving the medication oxytocin to stimulate the uterus to contract shortly after the baby is born.[2] Misoprostol may be used instead of oxytocin in resource poor settings.[2] Treatments may include: intravenous fluids, blood transfusions, and the medication ergotamine to cause further uterine contraction.[2] Efforts to compress the uterus using the hands may be effective if other treatments do not work.[2] The aorta may also be compressed by pressing on the abdomen.[2] The World Health Organization has recommended non-pneumatic anti-shock garment to help until other measures such as surgery can be carried out.[2] A 2017 study found that tranexamic acid decreased a woman's risk of death.[3]
In the developing world about 1.2% of deliveries are associated with PPH and when PPH occurred about 3% of women died.[2] Globally it occurs about 8.7 million times and results in 44,000 to 86,000 deaths per year making it the leading cause of death during pregnancy.[4][2][8] About 0.4 women per 100,000 deliveries die from PPH in the United Kingdom while about 150 women per 100,000 deliveries die in sub-Saharan Africa.[2] Rates of death have decreased substantially since at least the late 1800s in the United Kingdom.[2]
Definition
Depending on the source, primary postpartum bleeding is defined as blood loss in excess of 500 ml following vaginal delivery or 1000 ml following caesarean section in the first 24 hours following birth.[2] Secondary postpartum bleeding is that which occurs after the first day and up to six weeks after childbirth.[7]
Signs and symptoms
Symptoms generally include heavy bleeding from the vagina that doesn't slow or stop over time.[9] Initially there may be an increased heart rate, feeling faint upon standing, and an increased respiratory rate.[1] As more blood is lost, the woman may feel cold, blood pressure may drop, and she may become unconscious.[1]
Signs and symptoms of circulatory shock may also include blurry vision, cold and clammy skin, confusion, and feeling sleepy or weak.[1][9]
Causes
| Cause | Incidence |
|---|---|
| Uterine atony | 70% |
| Trauma | 20% |
| Retained tissue | 10% |
| Coagulopathy | 1% |
Causes of postpartum hemorrhage are uterine atony, trauma, retained placenta or placental abnormalities, and coagulopathy, commonly referred to as the "four Ts":[10]
- Tone: uterine atony is the inability of the uterus to contract and may lead to continuous bleeding. Retained placental tissue and infection may contribute to uterine atony. Uterine atony is the most common cause of postpartum hemorrhage.[11]
- Trauma: Injury to the birth canal which includes the uterus, cervix, vagina and the perineum which can happen even if the delivery is monitored properly. The bleeding is substantial as all these organs become more vascular during pregnancy.
- Tissue: retention of tissue from the placenta or fetus as well as placental abnormalities such as placenta accreta and percreta may lead to bleeding.
- Thrombin: a bleeding disorder occurs when there is a failure of clotting, such as with diseases known as coagulopathies.
Other risk factors include obesity, fever during pregnancy, bleeding before delivery, and heart disease.[7]
Prevention
Oxytocin is typically used right after the delivery of the baby to prevent PPH.[2] Misoprostol may be used in areas where oxytocin is not available.[2] Early clamping of the umbilical cord does not decrease risks and may cause anemia in the baby, thus is usually not recommended.[2]
Active management of the third stage is a method of shortening the stage between when the baby is born and when the placenta is delivered.[12] This stage is when the mother is at risk of having a PPH. Active management involves giving a drug which helps the uterus contract before delivering the placenta by a gentle but sustained pull on the umbilical cord whilst exerting upward pressure on the lower abdomen to support the uterus (controlled cord traction).[12]
Another method of active management which is not recommended now is fundal pressure during the delivery of the placenta. A review into this method found no research and advises controlled cord traction because fundal pressure can cause the mother unnecessary pain.[12] Allowing the cord to drain appears to shorten the third stage and reduce blood loss but evidence around this subject is not strong enough to draw solid conclusions.[13]
Nipple stimulation and breastfeeding triggers the release of natural oxytocin in the body, therefore it is thought that encouraging the baby to suckle soon after birth may reduce the risk of PPH for the mother.[14] A review looking into this did not find enough good research to say whether or not nipple stimulation did reduce PPH. More research is needed to answer this question.[14]
Management
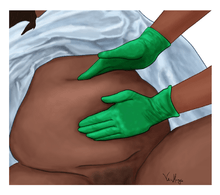
Uterine massage is a simple first line treatment as it helps the uterus to contract to reduce bleeding.[15] Although the evidence around the effectiveness of uterine massage is inconclusive, it is common practice after the delivery of the placenta.[15]
Medication
Intravenous oxytocin is the drug of choice for postpartum hemorrhage.[16] Ergotamine may also be used.[2]
Oxytocin helps the uterus to contract quickly and the contractions to last for longer.[17] It is the first line treatment for PPH when its cause is the uterus not contracting well.[18] A combination of syntocinon and ergometrine is commonly used as part of active management of the third stage of labour.[19] This is called syntometrine. Syntocinon alone lowers the risk of PPH.[20] Based on limited research available it is unclear whether syntocinon or syntometrine is most effective in preventing PPH but adverse effects are worse with syntometrine making syntocinon a more attractive option.[20] Ergometrine also has to be kept cool and in a dark place so that it is safe to use.[17] It does reduce the risk of PPH by improving the tone of the uterus when compared with no treatment however it has to be used with caution due to its effect raising blood pressure and causing worse after pains.[17]
More research would be useful in determining the best doses of ergometrine,[17] and syntocinon.[19]
Oxytocin requires refrigeration, which may not always be available, particularly in low-resourced settings.[21] When oxytocin is not available, misoprostol can be used.[18] Misoprostol does not need to be kept at a certain temperature and research into its effectiveness in reducing blood loss appears promising when compared with a placebo in a setting where it is not appropriate to use oxytocin.[21] Misoprostol can cause unpleasant side effects such as very high body temperatures and shivering.[22] Lower doses of misoprostol appear to be safer and cause less side effects.[22]
Giving oxytocin in a solution of saline into the umbilical vein is a method of administering the drugs directly to the placental bed and uterus.[23] However quality of evidence around this technique is poor and it is not recommended for routine use in the management of the third stage.[23] More research is needed to ascertain whether this is an effective way of administering uterotonic drugs.[23] As a way of treating a retained placenta, this method is not harmful but has not been shown to be effective.[24]
Carbetocin compared with oxytocin produced a reduction in women who needed uterine massage and further uterotonic drugs for women having caesarean sections.[25] There was no difference in rates of PPH in women having caesarean sections or women having vaginal deliveries when given carbetocin.[25] Carbetocin appears to cause less adverse effects. More research is needed to find the cost effectiveness of using carbetocin.[25]
Tranexamic acid, a clot stabilizing medication, may also be used to reduce bleeding and blood transfusions in low-risk women,[26] however evidence as of 2015 was not strong.[2] A 2017 trial found that it decreased the risk of death from bleeding from 1.9% to 1.5% in women with postpartum bleeding.[3] The benefit was greater when the medication was given within three hours.[3]
In some countries, such as Japan, methylergometrine and other herbal remedies are given following the delivery of the placenta to prevent severe bleeding more than a day after the birth. However, there is not enough evidence to suggest that these methods are effective.[27]
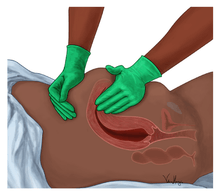
Surgery
Surgery may be used if medical management fails or in case of cervical lacerations or tear or uterine rupture. Methods used may include uterine artery ligation, ovarian artery ligation, internal iliac artery ligation, selective arterial embolization, B-lynch suture, and hysterectomy.[28][29][30][31] Bleeding caused by traumatic causes should be management by surgical repair. When there is bleeding due to uterine rupture a repair can be performed but most of the time a hysterectomy is needed.
Medical devices
The World Health Organization recommends the use of a device called the non-pneumatic anti-shock garment (NASG) for use in delivery activities outside of a hospital setting, the aim being to improve shock in a mother with obstetrical bleeding long enough to reach a hospital.[32] External aortic compression devices (EACD) may also be used.[33][34]
In the uterus, balloon tamponade can alleviate or stop postpartum hemorrhage. Inflating a Sengstaken–Blakemore tube in the uterus successfully treats atonic postpartum hemorrhage refractory to medical management in approximately 80% of cases.[35] Such procedure is relatively simple, inexpensive and has low surgical morbidity.[35] A Bakri balloon is a balloon tamponade specifically constructed for uterine postpartum hemorrhage.[36]
Protocol
Protocols to manage postpartum bleeding are recommended to ensure the rapid giving of blood products when needed.[37] A detailed stepwise management protocol has been introduced by the California Maternity Quality Care Collaborative.[38] It describes 4 stages of obstetrical hemorrhage after childbirth and its application reduces maternal mortality.[39]
- Stage 0: normal - treated with fundal massage and oxytocin.
- Stage 1: more than normal bleeding - establish large-bore intravenous access, assemble personnel, increase oxytocin, consider use of methergine, perform fundal massage, prepare 2 units of packed red blood cells.
- Stage 2: bleeding continues - check coagulation status, assemble response team, move to operating room, place intrauterine balloon, administer additional uterotonics (misoprostol, carboprost tromethamine), consider: uterine artery embolization, dilatation and curettage, and laparotomy with uterine compression stitches or hysterectomy.
- Stage 3: bleeding continues - activate massive transfusion protocol, mobilize additional personnel, recheck laboratory tests, perform laparotomy, consider hysterectomy.
A Cochrane review suggests that active management (use of uterotonic drugs, cord clamping and controlled cord traction) during the third stage of labour may reduce severe bleeding and anemia.[40] However, the review also found that active management increased the mother's blood pressure, nausea, vomiting, and pain. In the active management group more women returned to hospital with bleeding after discharge, and there was also a reduction in birthweight due to infants having a lower blood volume. The effects on the baby of early cord clamping was discussed in another review which found that delayed cord clamping improved iron stores longer term in the infants.[41] Although they were more likely to need phototherapy (light therapy) to treat jaundice, the improved iron stores are expected to be worth increasing the practice of delayed cord clamping in healthy term babies.[41] For preterm babies (babies born before 37 weeks) a review of the research found that delaying cord clamping by 30–45 seconds increased the amount of blood flow to the baby.[42] This is important as increased blood volume in the baby made them less likely to develop some serious complications.[42] Much of the research around this subject is poor quality so further, larger research projects are likely to produce more reliable results.[42]
Another Cochrane review looking at the timing of the giving oxytocin as part of the active management found similar benefits with giving it before or after the expulsion of the placenta.[43]
There is no good quality evidence on how best to treat a secondary PPH (PPH occurring 24 hrs or more after the birth).[44]
Epidemiology
Methods of measuring blood loss associated with childbirth vary, complicating comparison of prevalence rates.[45] A systematic review reported the highest rates of PPH in Africa (27.5%), and the lowest in Oceania (7.2%), with an overall rate globally of 10.8%.[45] The rate in both Europe and North America was around 13%.[45] The rate is higher for multiple pregnancies (32.4% compared with 10.6% for singletons), and for first-time mothers (12.9% compared with 10.0% for women in subsequent pregnancies).[45] The overall rate of severe PPH (>1000 ml) was much lower at an overall rate of 2.8%, again with the highest rate in Africa (5.1%).[45]
References
- Lynch, Christopher B- (2006). A textbook of postpartum hemorrhage : a comprehensive guide to evaluation, management and surgical intervention. Duncow: Sapiens Publishing. pp. 14–15. ISBN 9780955228230. Archived from the original on 2016-08-15.
- Weeks, A (January 2015). "The prevention and treatment of postpartum haemorrhage: what do we know, and where do we go to next?". BJOG : An International Journal of Obstetrics and Gynaecology. 122 (2): 202–10. doi:10.1111/1471-0528.13098. PMID 25289730.
- Shakur, Haleema; Roberts, Ian; Fawole, Bukola (April 2017). "Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial". The Lancet. 389 (10084): 2105–2116. doi:10.1016/S0140-6736(17)30638-4. PMC 5446563. PMID 28456509.
- GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Gibbs, Ronald S (2008). Danforth's obstetrics and gynecology (10th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 453. ISBN 9780781769372. Archived from the original on 2016-06-05.
- Lockhart, E (2015). "Postpartum hemorrhage: a continuing challenge". Hematology. American Society of Hematology. Education Program. 2015: 132–7. doi:10.1182/asheducation-2015.1.132. PMID 26637712.
- GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- "Postpartum hemorrhage". www.marchofdimes.org. Retrieved 2019-08-02.
- Anderson JM, Etches D (March 2007). "Prevention and management of postpartum hemorrhage". American Family Physician. 75 (6): 875–82. PMID 17390600.
- "Overview of postpartum hemorrhage". Archived from the original on 2015-01-15.
- Peña-Martí, G; Comunián-Carrasco, G (17 October 2007). "Fundal pressure versus controlled cord traction as part of the active management of the third stage of labour". The Cochrane Database of Systematic Reviews (4): CD005462. doi:10.1002/14651858.CD005462.pub2. PMID 17943858.
- Soltani, H; Poulose, TA; Hutchon, DR (7 September 2011). "Placental cord drainage after vaginal delivery as part of the management of the third stage of labour". The Cochrane Database of Systematic Reviews (9): CD004665. doi:10.1002/14651858.CD004665.pub3. PMID 21901693.
- Abedi, P; Jahanfar, S; Namvar, F; Lee, J (27 January 2016). "Breastfeeding or nipple stimulation for reducing postpartum haemorrhage in the third stage of labour". The Cochrane Database of Systematic Reviews. 1 (1): CD010845. doi:10.1002/14651858.CD010845.pub2. PMC 6718231. PMID 26816300.
- Hofmeyr, GJ; Abdel-Aleem, H; Abdel-Aleem, MA (1 July 2013). "Uterine massage for preventing postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 7 (7): CD006431. doi:10.1002/14651858.CD006431.pub3. PMID 23818022.
- WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization. 2012. ISBN 9789241548502.
- Liabsuetrakul, T; Choobun, T; Peeyananjarassri, K; Islam, QM (18 April 2007). "Prophylactic use of ergot alkaloids in the third stage of labour". The Cochrane Database of Systematic Reviews (2): CD005456. doi:10.1002/14651858.CD005456.pub2. PMID 17443592.
- Mousa, HA; Blum, J; Abou El Senoun, G; Shakur, H; Alfirevic, Z (13 February 2014). "Treatment for primary postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 2 (2): CD003249. doi:10.1002/14651858.CD003249.pub3. PMC 6483801. PMID 24523225.
- McDonald, S; Abbott, JM; Higgins, SP (2004). "Prophylactic ergometrine-oxytocin versus oxytocin for the third stage of labour". The Cochrane Database of Systematic Reviews (1): CD000201. doi:10.1002/14651858.CD000201.pub2. PMC 6491201. PMID 14973949.
- Salati, JA; Leathersich, SJ; Williams, MJ; Cuthbert, A; Tolosa, JE (29 April 2019). "Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 4: CD001808. doi:10.1002/14651858.CD001808.pub3. PMC 6487388. PMID 31032882.
- Tunçalp, Ö; Hofmeyr, GJ; Gülmezoglu, AM (15 August 2012). "Prostaglandins for preventing postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 8 (8): CD000494. doi:10.1002/14651858.CD000494.pub4. PMID 22895917.
- Hofmeyr, GJ; Gülmezoglu, AM; Novikova, N; Lawrie, TA (15 July 2013). "Postpartum misoprostol for preventing maternal mortality and morbidity". The Cochrane Database of Systematic Reviews. 7 (7): CD008982. doi:10.1002/14651858.CD008982.pub2. PMID 23857523.
- Mori, R; Nardin, JM; Yamamoto, N; Carroli, G; Weeks, A (14 March 2012). "Umbilical vein injection for the routine management of third stage of labour". The Cochrane Database of Systematic Reviews. 3 (3): CD006176. doi:10.1002/14651858.CD006176.pub2. PMID 22419311.
- Nardin, JM; Weeks, A; Carroli, G (11 May 2011). "Umbilical vein injection for management of retained placenta". The Cochrane Database of Systematic Reviews (5): CD001337. doi:10.1002/14651858.CD001337.pub2. PMID 21563129.
- Su, LL; Chong, YS; Samuel, M (18 April 2012). "Carbetocin for preventing postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 4 (4): CD005457. doi:10.1002/14651858.CD005457.pub4. PMID 22513931.
- Novikova, N; Hofmeyr, GJ; Cluver, C (16 June 2015). "Tranexamic acid for preventing postpartum haemorrhage". The Cochrane Database of Systematic Reviews. 6 (6): CD007872. doi:10.1002/14651858.CD007872.pub3. hdl:10019.1/104305. PMID 26079202.
- Yaju, Y; Kataoka, Y; Eto, H; Horiuchi, S; Mori, R (26 November 2013). "Prophylactic interventions after delivery of placenta for reducing bleeding during the postnatal period". The Cochrane Database of Systematic Reviews. 11 (11): CD009328. doi:10.1002/14651858.CD009328.pub2. PMID 24277681.
- O'Leary JA (March 1995). "Uterine artery ligation in the control of postcesarean hemorrhage". The Journal of Reproductive Medicine. 40 (3): 189–93. PMID 7776302.
- Vedantham S, Goodwin SC, McLucas B, Mohr G (April 1997). "Uterine artery embolization: an underused method of controlling pelvic hemorrhage". American Journal of Obstetrics and Gynecology. 176 (4): 938–48. doi:10.1016/S0002-9378(97)70624-0. PMID 9125624.
- Price N, B-Lynch C (2005). "Technical description of the B-Lynch brace suture for treatment of massive postpartum hemorrhage and review of published cases". International Journal of Fertility and Women's Medicine. 50 (4): 148–63. PMID 16405100.
- Plauche, WC (1992). Peripartal Hysterectomy. Philadelphia, Pa: WB Saunders. pp. 447–65.
- Craig, Elise (December 2013). "A Life Preserver For New Moms". Alpha. WIRED. p. 52.
- Soltan MH, Faragallah MF, Mosabah MH, Al-Adawy AR (June 2009). "External aortic compression device: the first aid for postpartum hemorrhage control". The Journal of Obstetrics and Gynaecology Research. 35 (3): 453–8. doi:10.1111/j.1447-0756.2008.00975.x. PMID 19527382.
- Soltan MH, Sadek RR (November 2011). "Experience managing postpartum hemorrhage at Minia University Maternity Hospital, Egypt: no mortality using external aortic compression". The Journal of Obstetrics and Gynaecology Research. 37 (11): 1557–63. doi:10.1111/j.1447-0756.2011.01574.x. PMID 21676082.
- Doumouchtsis, S. K.; Papageorghiou, A. T.; Vernier, C.; Arulkumaran, S. (2008). "Management of postpartum hemorrhage by uterine balloon tamponade: Prospective evaluation of effectiveness". Acta Obstetricia et Gynecologica Scandinavica. 87 (8): 849–855. doi:10.1080/00016340802179822. PMID 18704777.
- Chapter 89 - Balloon tamponade and uterine packing for major PPH from South Australia, Department of Health. 2005
- Ducloy-Bouthors, Anne-Sophie; Susen, Sophie; Wong, Cynthia A.; Butwick, Alex; Vallet, Benoit; Lockhart, Evelyn (November 2014). "Medical advances in the treatment of postpartum hemorrhage". Anesthesia and Analgesia. 119 (5): 1140–1147. doi:10.1213/ANE.0000000000000450. ISSN 1526-7598. PMID 25329026.
- Sheikh L, Zuberi NF, Rizvi JH. "Massive primary postpartum haemorrhage: setting up standards of care". CMQCC. Retrieved 2009-12-22. CMQCC guidelines, accessed August 10, 2009
- Barbieri RL (2009). "Planning reduces the risk of maternal death. This tool helps". OBG Management. 21 (8): 8–10.
- Begley, CM; Gyte, GM; Devane, D; McGuire, W; Weeks, A; Biesty, LM (13 February 2019). "Active versus expectant management for women in the third stage of labour". Cochrane Database of Systematic Reviews. 2: CD007412. doi:10.1002/14651858.CD007412.pub5. PMC 6372362. PMID 30754073.
- McDonald, SJ; Middleton, P; Dowswell, T; Morris, PS (11 July 2013). "Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes". The Cochrane Database of Systematic Reviews. 7 (7): CD004074. doi:10.1002/14651858.CD004074.pub3. PMC 6544813. PMID 23843134.
- Rabe, H; Diaz-Rossello, JL; Duley, L; Dowswell, T (15 August 2012). "Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes". The Cochrane Database of Systematic Reviews. 8 (8): CD003248. doi:10.1002/14651858.CD003248.pub3. PMID 22895933.
- Soltani H, Hutchon DR, Poulose TA (August 2010). "Timing of prophylactic uterotonics for the third stage of labour after vaginal birth". The Cochrane Database of Systematic Reviews (8): CD006173. doi:10.1002/14651858.CD006173.pub2. PMID 20687079.
- Alexander, J; Thomas, P; Sanghera, J (2002). "Treatments for secondary postpartum haemorrhage". The Cochrane Database of Systematic Reviews (1): CD002867. doi:10.1002/14651858.CD002867. PMID 11869640.
- Calvert, C; Thomas, SL; Ronsmans, C; Wagner, KS; Adler, AJ; Filippi, V (2012). "Identifying regional variation in the prevalence of postpartum haemorrhage: a systematic review and meta-analysis". PLOS ONE. 7 (7): e41114. Bibcode:2012PLoSO...741114C. doi:10.1371/journal.pone.0041114. PMC 3402540. PMID 22844432.
External links
| Classification | |
|---|---|
| External resources |
- WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization. 2012. ISBN 9789241548502.
- Postpartum hemorrhage and the B-Lynch technique