Photoplethysmogram
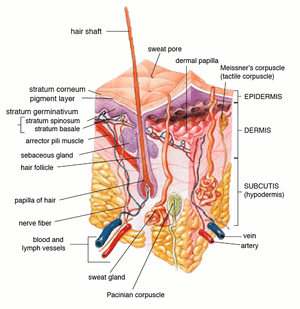
A photoplethysmogram (PPG) is an optically obtained plethysmogram that can be used to detect blood volume changes in the microvascular bed of tissue. A PPG is often obtained by using a pulse oximeter which illuminates the skin and measures changes in light absorption.[1] A conventional pulse oximeter monitors the perfusion of blood to the dermis and subcutaneous tissue of the skin.
| Photoplethysmography | |
|---|---|
| Medical diagnostics | |
Representative PPG taken from an ear pulse oximeter. Variation in amplitude are from Respiratory Induced Variation. | |
| MeSH | D017156 |
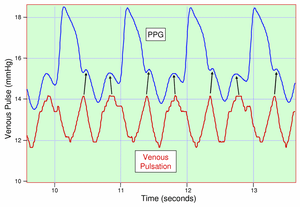
With each cardiac cycle the heart pumps blood to the periphery. Even though this pressure pulse is somewhat damped by the time it reaches the skin, it is enough to distend the arteries and arterioles in the subcutaneous tissue. If the pulse oximeter is attached without compressing the skin, a pressure pulse can also be seen from the venous plexus, as a small secondary peak.
The change in volume caused by the pressure pulse is detected by illuminating the skin with the light from a light-emitting diode (LED) and then measuring the amount of light either transmitted or reflected to a photodiode[2]. Each cardiac cycle appears as a peak, as seen in the figure. Because blood flow to the skin can be modulated by multiple other physiological systems, the PPG can also be used to monitor breathing, hypovolemia, and other circulatory conditions.[3] Additionally, the shape of the PPG waveform differs from subject to subject, and varies with the location and manner in which the pulse oximeter is attached.
Sites for measuring PPG

While pulse oximeters are a commonly used medical device, the PPG derived from them is rarely displayed and is nominally only processed to determine heart rate. PPGs can be obtained from transmissive absorption (as at the finger tip) or reflection (as on the forehead).
In outpatient settings, pulse oximeters are commonly worn on the finger. However, in cases of shock, hypothermia, etc. blood flow to the periphery can be reduced, resulting in a PPG without a discernible cardiac pulse.[4] In this case, a PPG can be obtained from a pulse oximeter on the head, with the most common sites being the ear, nasal septum, and forehead. PPG can also be configured as multi-site photoplethysmography (MPPG), e.g. making simultaneous measurements from the right and left ear lobes, index fingers and great toes, and offering further opportunities for the assessment of patients with suspected peripheral arterial disease, autonomic dysfunction, endothelial dysfunction, and arterial stiffness. MPPG also offers significant potential for data mining, e.g. using deep learning, as well as a range of other innovative pulse wave analysis techniques. [5][6][7]
PPGs can also be obtained from the following parts:
- the vagina (vaginal photoplethysmograph)
- the clitoris (clitoral photoplethysmograph)
- the esophagus
Motion artifacts have been shown to be a limiting factor preventing accurate readings during exercise and free living conditions.
Uses
Monitoring heart rate and cardiac cycle
Because the skin is so richly perfused, it is relatively easy to detect the pulsatile component of the cardiac cycle. The DC component of the signal is attributable to the bulk absorption of the skin tissue, while the AC component is directly attributable to variation in blood volume in the skin caused by the pressure pulse of the cardiac cycle.
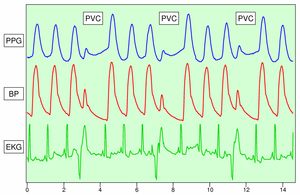
The height of AC component of the photoplethysmogram is proportional to the pulse pressure, the difference between the systolic and diastolic pressure in the arteries. As seen in the figure showing premature ventricular contractions (PVCs), the PPG pulse for the cardiac cycle with the PVC results in lower amplitude blood pressure and a PPG. Ventricular tachycardia and ventricular fibrillation can also be detected.[8]
Monitoring respiration
Respiration affects the cardiac cycle by varying the intrapleural pressure, the pressure between the thoracic wall and the lungs. Since the heart resides in the thoracic cavity between the lungs, the partial pressure of inhaling and exhaling greatly influence the pressure on the vena cava and the filling of the right atrium. This effect is often referred to as normal sinus arrhythmia.
During inspiration, intrapleural pressure decreases by up to 4 mm Hg, which distends the right atrium, allowing for faster filling from the vena cava, increasing ventricular preload, but decreasing stroke volume. Conversely during expiration, the heart is compressed, decreasing cardiac efficiency and increasing stroke volume. When the frequency and depth of respiration increases, the venous return increases, leading to increased cardiac output.[10]
Monitoring depth of anesthesia
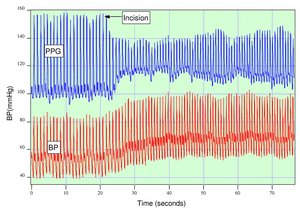
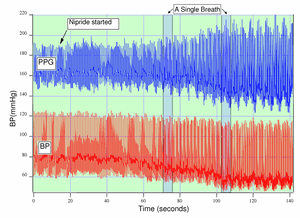
Anesthesiologists must often judge subjectively whether a patient is sufficiently anesthetized for surgery. As seen in the figure, if a patient is not sufficiently anesthetized, the sympathetic nervous system response to an incision can generate an immediate response in the amplitude of the PPG.[9]
Monitoring hypo- and hypervolemia
Shamir, Eidelman, et al. studied the interaction between inspiration and removal of 10% of a patient’s blood volume for blood banking before surgery.[11] They found that blood loss could be detected both from the photoplethysmogram from a pulse oximeter and an arterial catheter. Patients showed a decrease in the cardiac pulse amplitude caused by reduced cardiac preload during exhalation when the heart is being compressed.
Monitoring blood pressure
The FDA reportedly provided clearance to a photoplethysmography-based cuffless blood pressure monitor in August 2019.[12]
Remote photoplethysmography
Conventional imaging
While photoplethysmography commonly requires some form of contact with the human skin (e.g., ear, finger), remote photoplethysmography allows to determine physiological processes such as blood flow without skin contact. This is achieved by using face video to analyze subtle momentary changes in the subject's skin color which are not detectable to the human eye.[13][14] Such camera-based measurement of blood oxygen levels provides a contactless alternative to conventional photoplethysmography. For instance, it can be used to monitor the heart rate of newborn babies.[15]
Digital holography
Remote photoplethysmography can also be performed by digital holography, which is sensitive to the phase of light waves, and hence very sensitive to sub-micron out-of-plane motion[16]. A refinement of this technique, holographic laser Doppler imaging, enables non-invasive retinal and choroidal blood flow pulse wave monitoring [17].
See also
References
- K. Shelley and S. Shelley, Pulse Oximeter Waveform: Photoelectric Plethysmography, in Clinical Monitoring, Carol Lake, R. Hines, and C. Blitt, Eds.: W.B. Saunders Company, 2001, pp. 420-428.
- E. Aguilar Pelaez et al., "LED power reduction trade-offs for ambulatory pulse oximetry," 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, 2007, pp. 2296-2299. doi: 10.1109/IEMBS.2007.4352784, URL: http://ieeexplore.ieee.org/stamp/stamp.jsp?tp=&arnumber=4352784&isnumber=4352185
- Reisner A, Shaltis PA, McCombie D, Asada HH (May 2008). "Utility of the photoplethysmogram in circulatory monitoring". Anesthesiology. 108 (5): 950–8. doi:10.1097/ALN.0b013e31816c89e1. PMID 18431132.
- Budidha, K; Kyriacou, PA (August 2015). "Investigation of photoplethysmography and arterial blood oxygen saturation from the ear-canal and the finger under conditions of artificially induced hypothermia" (PDF). Conference Proceedings : ... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2015: 7954–7. doi:10.1109/EMBC.2015.7320237. ISBN 978-1-4244-9271-8. PMID 26738137.
- Allen, John; Overbeck, Klaus; Nath, Alexander F.; Murray, Alan; Stansby, Gerard (Apr 2008). "A prospective comparison of bilateral photoplethysmography versus the ankle-brachial pressure index for detecting and quantifying lower limb peripheral arterial disease". J Vasc Surg. 47 (4): 794–802. doi:10.1016/j.jvs.2007.11.057. PMID 18381141.
- McKay, N. D.; Griffiths, B.; Di Maria, C.; Hedley, S.; Murray, A.; Allen, J. (Oct 2014). "Novel photoplethysmography cardiovascular assessments in patients with Raynaud's phenomenon and systemic sclerosis: a pilot study". Rheumatology (Oxford). 53 (10): 1855–63. doi:10.1093/rheumatology/keu196. PMID 24850874.
- Mizeva, Irina; Di Maria, Costanzo; Frick, Peter; Podtaev, Sergey; Allen, John (Mar 2015). "Quantifying the correlation between photoplethysmography and laser Doppler flowmetry microvascular low-frequency oscillations". J Biomed Optics. 20 (3): 037007. Bibcode:2015JBO....20c7007M. doi:10.1117/1.JBO.20.3.037007. PMID 25764202.
- Alian, AA; Shelley, KH (December 2014). "Photoplethysmography". Best Practice & Research. Clinical Anaesthesiology. 28 (4): 395–406. doi:10.1016/j.bpa.2014.08.006. PMID 25480769.
- Shelley, KH (December 2007). "Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate". Anesthesia and Analgesia. 105 (6 Suppl): S31–6, tables of contents. doi:10.1213/01.ane.0000269512.82836.c9. PMID 18048895.
- Shelley, KH; Jablonka, DH; Awad, AA; Stout, RG; Rezkanna, H; Silverman, DG (August 2006). "What is the best site for measuring the effect of ventilation on the pulse oximeter waveform?". Anesthesia and Analgesia. 103 (2): 372–7, table of contents. doi:10.1213/01.ane.0000222477.67637.17. PMID 16861419.
- M. Shamir, L. A. Eidelman, Y. Floman, L. Kaplan, and R. Pi-zov, Pulse Oximetry Plethysmographic Waveform During Changes in Blood Volume, Br. J. Anaesth., vol. 82, pp. 178-181, 1999.
- Wendling, Patrice (28 August 2019). "FDA Okays Biobeat's Cuffless Blood Pressure Monitor". Medscape. Retrieved 5 September 2019.
- Verkruysse, W.; Svaasand, L.O.; Nelson, J.S. (2008). "Remote plethysmographic imaging using ambient light". Optics Express. 16 (26): 21434–21445. Bibcode:2008OExpr..1621434V. doi:10.1364/OE.16.021434. PMC 2717852. PMID 19104573.
- Rouast, P.V.; Adam, M.T.P.; Chiong, R.; Cornforth, D.; Lux, E. (2018). "Remote heart rate measurement using low-cost RGB face video: A technical literature review". Frontiers of Computer Science. 12 (5): 858–872. doi:10.1007/s11704-016-6243-6.
- https://www.youtube.com/watch?v=7Nq73-jYbpY
- Bencteux, Jeffrey (2015). "Holographic laser Doppler imaging of pulsatile blood flow". Journal of Biomedical Optics. 20 (6): 066006. arXiv:1501.05776. doi:10.1117/1.JBO.20.6.066006.
- Puyo, L., M. Paques, M. Fink, J-A. Sahel, and M. Atlan. "In vivo laser Doppler holography of the human retina." Biomedical optics express 9, no. 9 (2018): 4113-4129.