Pelvic congestion syndrome
Pelvic congestion syndrome, also known as pelvic vein incompetence, is a long term condition in women believed to be due to enlarged veins in the lower abdomen.[1][3] The condition may cause chronic pain, such as a constant dull ache, which can be worsened by standing or sex.[1] Pain in the legs or lower back may also occur.[1]
| Pelvic congestion syndrome | |
|---|---|
| Other names | Pelvic vein incompetence |
 | |
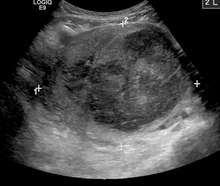
| A very large (9cm) fibroid of the uterus which is causing pelvic congestion syndrome as seen on X-ray computed tomography | |
| Specialty | Urology, gynecology |
| Symptoms | Chronic pelvic pain[1] |
| Diagnostic method | Ultrasound, CT scan, MRI, laparoscopy[1] |
| Medication | Medroxyprogesterone, nonsteroidal anti-inflammatory drugs (NSAIDs)[1] |
| Frequency | 15% of women[2] |
While the condition is believed to be due to blood flowing back into pelvic veins as a result of faulty valves in the veins, this hypothesis is not certain.[3] The condition may occur or worsen during pregnancy.[1] The presence of estrogen is believed to be involved in the mechanism.[1] Diagnosis may be supported by ultrasound, CT scan, MRI, or laparoscopy.[1]
Early treatment options include medroxyprogesterone or nonsteroidal anti-inflammatory drugs (NSAIDs).[1] Surgery to block the varicose veins may also be done.[1] About 15% of women of reproductive age are affected.[2] It is believed to be the cause of about a third of chronic pelvic pain cases.[2] While pelvic venous insufficiency was identified in the 1850s it was only linked with pelvic pain in the 1940s.[2]
Signs and symptoms
Women with this condition experience a constant pain that may be dull and aching, but is occasionally more acute. The pain is worse at the end of the day and after long periods of standing, and sufferers get relief when they lie down. The pain is worse during or after sexual intercourse, and can be worse just before the onset of the menstrual period.[4]
Women with pelvic congestion syndrome have a larger uterus and a thicker endometrium. 56% of women manifest cystic changes to the ovaries,[5] and many report other symptoms, such as dysmenorrhea, back pain, vaginal discharge, abdominal bloating, mood swings or depression, and fatigue.[4]
Causes
- Local pelvic hormonal melieu
- Venous outflow obstruction, such as May-Thurner syndrome, Nutcracker syndrome, Budd-Chiari syndrome, or left renal vein thrombosis
- External compression due to tumor (including fibroids, endometriosis), or scarring [6]
Diagnosis
Diagnosis can be made using ultrasound or laparoscopy testing. The condition can also be diagnosed with a venogram, CT scan, or an MRI. Ultrasound is the diagnostic tool most commonly used.[4] Some research has suggested that transvaginal duplex ultrasound is the best test for pelvic venous reflux.[7]
Treatment
Early treatment options include pain medication using nonsteroidal anti-inflammatory drugs,[4] and suppression of ovarian function.[5]
The surgical option involves stopping blood flow to the varicose veins using noninvasive surgical techniques such as a procedure called embolization. The procedure requires an overnight stay in hospital, and is done using local anesthetic.[8] Patients report an 80% success rate, as measured by the amount of pain reduction experienced.[8]
See also
References
- "Pelvic Congestion Syndrome - Women's Health Issues". Merck Manuals Consumer Version. Retrieved 27 September 2019.
- Brown, CL; Rizer, M; Alexander, R; Sharpe EE, 3rd; Rochon, PJ (March 2018). "Pelvic Congestion Syndrome: Systematic Review of Treatment Success". Seminars in interventional radiology. 35 (1): 35–40. doi:10.1055/s-0038-1636519. PMC 5886772. PMID 29628614.
- Champaneria, R; Shah, L; Moss, J; Gupta, JK; Birch, J; Middleton, LJ; Daniels, JP (January 2016). "The relationship between pelvic vein incompetence and chronic pelvic pain in women: systematic reviews of diagnosis and treatment effectiveness". Health technology assessment (Winchester, England). 20 (5): 1–108. doi:10.3310/hta20050. PMID 26789334.
- "Dysmenorrhea". Merck Online Medical Manual. December 2008. Retrieved December 23, 2010.
- Phillip Reginald, MD. "Pelvic Congestion" (PDF). The International Pelvic Pain Society. Retrieved December 23, 2010.
- Rutherford's vascular surgery references. [S.l.]: Elsevier Saunders. 2014. ISBN 0323243053.
- Whiteley M, Dos Santos S, Harrison C, Holdstock J, Lopez A (Oct 2014). "Transvaginal duplex ultrasonography appears to be the gold standard investigation for the haemodynamic evaluation of pelvic venous reflux in the ovarian and internal iliac veins in women". Phlebology. 30: 706–13. doi:10.1177/0268355514554638. PMID 25324278.
- "Pelvic Pain (Pelvic Congestion Syndrome)". Johns Hopkins. Retrieved December 23, 2010.