Atrial fibrillation
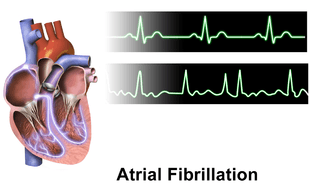
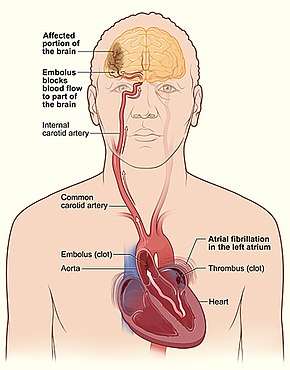
Atrial fibrillation (AF or A-fib) is an abnormal heart rhythm or arrhythmia characterized by rapid and irregular beating of the atrial chambers of the heart.[11] It often begins as short periods of abnormal beating which become longer or continuous over time.[4] It may also start as other forms of arrhythmia such as atrial flutter that then transform into AF.[12] Often episodes have no symptoms.[3] Occasionally there may be heart palpitations, fainting, lightheadedness, shortness of breath, or chest pain.[2] The disease is associated with an increased risk of heart failure, dementia, and stroke.[3] It is a type of supraventricular tachycardia.[13]
| Atrial fibrillation | |
|---|---|
| Other names | Auricular fibrillation[1] |
.jpg) | |
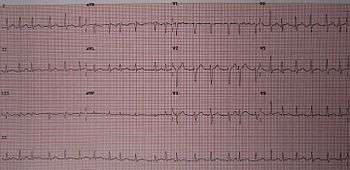
| Leads V4 and V5 of an electrocardiogram showing atrial fibrillation with somewhat irregular intervals between heart beats, no P waves, and a heart rate of about 150 BPM. | |
| Specialty | Cardiology |
| Symptoms | None, heart palpitations, fainting, shortness of breath, chest pain[2][3] |
| Complications | Heart failure, dementia, stroke[3] |
| Usual onset | > age 50[4] |
| Risk factors | High blood pressure, valvular heart disease, coronary artery disease, cardiomyopathy, congenital heart disease, COPD, obesity, smoking, sleep apnea[3][5][6][7] |
| Diagnostic method | Feeling the pulse, electrocardiogram[8] |
| Differential diagnosis | Irregular heartbeat[9] |
| Treatment | Rate control or rhythm control[5] |
| Frequency | 2.5% (developed world), 0.5% (developing world)[4] |
| Deaths | 193,300 with atrial flutter (2015)[10] |
High blood pressure and valvular heart disease are the most common alterable risk factors for AF.[5][6] Other heart-related risk factors include heart failure, coronary artery disease, cardiomyopathy, and congenital heart disease.[5] In the developing world valvular heart disease often occurs as a result of rheumatic fever.[14] Lung-related risk factors include COPD, obesity, and sleep apnea.[3] Other factors include excess alcohol intake, tobacco smoking, diabetes mellitus, and thyrotoxicosis.[3][7][14] However, half of cases are not associated with any of these risks.[3] A diagnosis is made by feeling the pulse and may be confirmed using an electrocardiogram (ECG).[8] A typical ECG in AF shows no P waves and an irregular ventricular rate.[8]
AF is often treated with medications to slow the heart rate to a near normal range (known as rate control) or to convert the rhythm to normal sinus rhythm (known as rhythm control).[5] Electrical cardioversion can also be used to convert AF to a normal sinus rhythm and is often used emergently if the person is unstable.[15] Ablation may prevent recurrence in some people.[16] For those at low risk of stroke, no specific treatment is typically required, though aspirin or an anti-clotting medication may occasionally be considered.[17] For those at more than low risk, an anti-clotting medication is typically recommended.[17] Anti-clotting medications include warfarin and direct oral anticoagulants.[17] Most people are at higher risk of stroke.[18] While these medications reduce stroke risk, they increase rates of major bleeding.[19]
Atrial fibrillation is the most common serious abnormal heart rhythm.[3] In Europe and North America, as of 2014, it affects about 2 to 3% of the population.[4] This is an increase from 0.4 to 1% of the population around 2005.[20] In the developing world, about 0.6% of males and 0.4% of females are affected.[4] The percentage of people with AF increases with age with 0.1% under 50 years old, 4% between 60 and 70 years old, and 14% over 80 years old being affected.[4] A-fib and atrial flutter resulted in 193,300 deaths in 2015, up from 29,000 in 1990.[10][21] The first known report of an irregular pulse was by Jean-Baptiste de Sénac in 1749.[3] This was first documented by ECG in 1909 by Thomas Lewis.[3]
Signs and symptoms
AF is usually accompanied by symptoms related to a rapid heart rate. Rapid and irregular heart rates may be perceived as the sensation of the heart beating too fast, irregularly, or skipping beats (palpitations) or exercise intolerance and occasionally may produce anginal chest pain (if the high heart rate causes the heart's demand for oxygen to increase beyond the supply of available oxygen (ischemia)). Other possible symptoms include congestive heart failure symptoms such as fatigue, shortness of breath, or swelling. The abnormal heart rhythm (arrhythmia) is sometimes only identified with the onset of a stroke or a transient ischemic attack (TIA). It is not uncommon for a person to first become aware of AF from a routine physical examination or ECG, as it often does not cause symptoms.[20]
Since most cases of AF are secondary to other medical problems, the presence of chest pain or angina, signs and symptoms of hyperthyroidism (an overactive thyroid gland) such as weight loss and diarrhea, and symptoms suggestive of lung disease can indicate an underlying cause. A history of stroke or TIA, as well as high blood pressure, diabetes, heart failure, or rheumatic fever may indicate whether someone with AF is at a higher risk of complications.[20] The risk of a blood clot forming in the left atrial chamber of the heart, breaking off, and then traveling in the bloodstream can be assessed using the CHADS2 score or CHA2DS2-VASc score.
Rapid heart rate
Presentation is similar to other forms of rapid heart rate and may be asymptomatic.[22] Palpitations and chest discomfort are common complaints.[22] The rapid uncoordinated heart rate may result in reduced output of blood pumped by the heart (cardiac output) resulting in inadequate blood flow and therefore oxygen delivery to the rest of the body. Common symptoms of uncontrolled atrial fibrillation may include shortness of breath,[22] shortness of breath when lying flat, dizziness, and sudden onset of shortness of breath during the night. This may progress to swelling of the lower extremities, a manifestation of congestive heart failure. Due to inadequate cardiac output, individuals with AF may also complain of light-headedness,[22] may feel like they are about to faint, or may actually lose consciousness.
AF can cause respiratory distress due to congestion in the lungs. By definition, the heart rate will be greater than 100 beats per minute. Blood pressure may be variable, and often difficult to measure as the beat-by-beat variability causes problems for most digital (oscillometric) non-invasive blood pressure monitors. For this reason, when determining heart rate in AF, direct cardiac auscultation is recommended. Low blood pressure is most concerning and a sign that immediate treatment is required. Many of the symptoms associated with uncontrolled atrial fibrillation are a manifestation of congestive heart failure due to the reduced cardiac output. Respiratory rate will be increased in the presence of respiratory distress. Pulse oximetry may confirm the presence of too little oxygen reaching the body's tissues related to any precipitating factors such as pneumonia. Examination of the jugular veins may reveal elevated pressure (jugular venous distention). Examination of the lungs may reveal crackles, which are suggestive of pulmonary edema. Examination of the heart will reveal a rapid irregular rhythm.
Causes
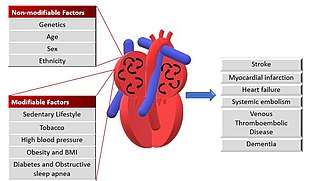
AF is linked to several forms of cardiovascular disease, but may occur in otherwise normal hearts. Cardiovascular factors known to be associated with the development of AF include high blood pressure, coronary artery disease, mitral valve stenosis (e.g., due to rheumatic heart disease or mitral valve prolapse), mitral regurgitation, left atrial enlargement, hypertrophic cardiomyopathy (HCM), pericarditis, congenital heart disease, and previous heart surgery. Additionally, lung diseases (such as pneumonia, lung cancer, pulmonary embolism, and sarcoidosis) are thought to play a role in certain people. Disorders of breathing during sleep such as obstructive sleep apnea (OSA) are also associated with AF.[23] Obesity is a risk factor for AF.[24] Hyperthyroidism and subclinical hyperthyroidism are associated with AF development.[25] Caffeine consumption does not appear to be associated with AF,[26] but excessive alcohol consumption ("binge drinking" or "holiday heart syndrome") is linked to AF.[27] Sepsis also increases the risk of developing new-onset atrial fibrillation.[28][29] Long-term endurance exercise (e.g., long-distance bicycling or marathon running) appears to be associated with a modest increase in the risk of atrial fibrillation in middle-aged and elderly people.[18][30][31] Tobacco smoking and secondhand tobacco smoke exposure are associated with an increased risk of developing atrial fibrillation.[7][32]
Genetics
A family history of AF may increase the risk of AF. A study of more than 2,200 people found an increased risk factor for AF of 1.85 for those that had at least one parent with AF.[33][34][35] Various genetic mutations may be responsible.[36][37]
Four types of genetic disorder are associated with atrial fibrillation:[38]
- Familial AF as a monogenic disease
- Familial AF presenting in the setting of another inherited cardiac disease (hypertrophic cardiomyopathy, dilated cardiomyopathy, familial amyloidosis)
- Inherited arrhythmic syndromes (congenital long QT syndrome, short QT syndrome, Brugada syndrome)
- Non-familial AF associated with genetic backgrounds (polymorphism in the ACE gene) that may predispose to atrial fibrillation
Family history in a first degree relative is associated with a 40% increase in risk of AF. This finding led to the mapping of different loci such as 10q22-24, 6q14-16 and 11p15-5.3 and discover mutations associated with the loci. Fifteen mutations of gain and loss of function have been found in the genes of K+ channels, including mutations in KCNE1-5, KCNH2, KCNJ5 or ABCC9 among others. Six variations in genes of Na+ channels that include SNC1-4B, SNC5A and SNC10A have also been found. All of these mutations affect the processes of polarization-depolarization of the myocardium, cellular hyper-excitability, shortening of effective refractory period favouring re-entries.[39] Other mutations in genes, such as GJA5, affect Gap junctions, generating a cellular uncoupling that promotes re-entries and a slow conduction velocity.[40] Using genome-wide association study, which screen the entire genome for single nucleotide polymorphism (SNP), three susceptibility loci have been found for AF (4q25, 1q21 and 16q22).[41] In these loci there are SNPs associated with a 30% increase in risk of recurrent atrial tachycardia after ablation. There is also SNPs associated with loss of function of the Pitx2c gene (involved in cellular development of pulmonary valves), responsible for re-entries. There are also SNPs close to ZFHX3 genes involved in the regulation of Ca2+.[39] A GWAS meta-analysis study conducted in 2018 revealed the discovery of 70 new loci associated with AF. Different variants have been identified. They are associated with genes that encode transcription factors, such as TBX3 and TBX5, NKX2-5 or PITX2, involved in the regulation of cardiac conduction, modulation of ion channels and in cardiac development. Have been also identified new genes involved in tachycardia (CASQ2) or associated with an alteration in cardiomyocyte communication (PKP2).[42]
Sedentary lifestyle
A sedentary lifestyle increases the risk factors associated with AF such as obesity, hypertension or diabetes mellitus. This favors remodeling processes of the atrium due to inflammation or alterations in the depolarization of cardiomyocytes by elevation of sympathetic nervous system activity.[39][43] A sedentary lifestyle is associated with an increased risk of AF compared to physical activity. In both men and women, the practice of moderate exercise reduces the risk of AF progressively,[44] but intense sports may increase the risk of developing AF, as seen in athletes.[45] It is due to a remodeling of cardiac tissue,[46] and an increase in vagal tone, which shortens the effective refractory period (ERP) favoring re-entries from the pulmonary veins.[44]
High blood pressure
According to the CHARGE Consortium both systolic and diastolic blood pressure are predictors of the risk of AF. Systolic blood pressure values close to normal limit the increase in the risk associated with AF. Diastolic dysfunction is also associated with AF, which increased pressure, left atrial volume, size, and left ventricular hypertrophy, characteristic of chronic hypertension. All atrial remodeling is related to a heterogeneous conduction and the formation of re-entrant electric conduction from the pulmonary veins.[39][47]
Tobacco
The rate of AF in smokers is 1.4 times higher than in non-smokers.[47] Tobacco use increases susceptibility to AF through different processes. Exposure to tobacco products increases the release of catecholamines (e.g., epinephrine or norepinephrine) and promotes narrowing of the coronary arteries, leading to inadequate blood flow and oxygen delivery to the heart. In addition, it accelerates atherosclerosis, due to its effect of oxidative stress on lipids and inflammation, which leads to the formation of blood clots. Finally, nicotine induces the formation of patterns of collagen type III in the atrium and has profibrotic effects. All this modifies the atrial tissue, favoring the re-entry.[48][49]
Other diseases
There is a relationship between risk factors such as obesity and hypertension, with the appearance of diseases such as diabetes mellitus and sleep apnea-hypopnea syndrome, specifically, obstructive sleep apnea (OSA). These diseases are associated with an increased risk of AF due to their remodeling effects on the left atrium.[39]
Pathophysiology
The normal electrical conduction system of the heart allows the impulse that is generated by the sinoatrial node (SA node) of the heart to be propagated to and stimulate the myocardium (muscular layer of the heart). When the myocardium is stimulated, it contracts. It is the ordered stimulation of the myocardium that allows efficient contraction of the heart, thereby allowing blood to be pumped to the body.
In AF, the normal regular electrical impulses generated by the sinoatrial node in the right atrium of the heart are overwhelmed by disorganized electrical impulses usually originating in the roots of the pulmonary veins. This leads to irregular conduction of ventricular impulses that generate the heartbeat.
Pathology
The primary pathologic change seen in atrial fibrillation is the progressive fibrosis of the atria. This fibrosis is due primarily to atrial dilation; however, genetic causes and inflammation may be factors in some individuals. Dilation of the atria can be due to almost any structural abnormality of the heart that can cause a rise in the pressure within the heart. This includes valvular heart disease (such as mitral stenosis, mitral regurgitation, and tricuspid regurgitation), hypertension, and congestive heart failure. Any inflammatory state that affects the heart can cause fibrosis of the atria. This is typically due to sarcoidosis but may also be due to autoimmune disorders that create autoantibodies against myosin heavy chains. Mutation of the lamin AC gene is also associated with fibrosis of the atria that can lead to atrial fibrillation.
Once dilation of the atria has occurred, this begins a chain of events that leads to the activation of the renin–angiotensin–aldosterone system (RAAS) and subsequent increase in matrix metalloproteinases and disintegrin, which leads to atrial remodeling and fibrosis, with loss of atrial muscle mass. This process occurs gradually, and experimental studies have revealed patchy atrial fibrosis may precede the occurrence of atrial fibrillation and may progress with prolonged durations of atrial fibrillation.
Fibrosis is not limited to the muscle mass of the atria and may occur in the sinus node (SA node) and atrioventricular node (AV node), correlating with sick sinus syndrome. Prolonged episodes of atrial fibrillation have been shown to correlate with prolongation of the sinus node recovery time,[20] suggesting that dysfunction of the SA node is progressive with prolonged episodes of atrial fibrillation.
Electrophysiology
| Conduction | ||
Sinus rhythm  |
Atrial fibrillation  | |
There are multiple theories about the cause of atrial fibrillation. An important theory is that, in atrial fibrillation, the regular impulses produced by the sinus node for a normal heartbeat are overwhelmed by rapid electrical discharges produced in the atria and adjacent parts of the pulmonary veins. Sources of these disturbances are either automatic foci, often localized at one of the pulmonary veins, or a small number of localized sources in the form of either a re-entrant leading circle, or electrical spiral waves (rotors); these localized sources may be found in the left atrium near the pulmonary veins or in a variety of other locations through both the left or right atrium. There are three fundamental components that favor the establishment of a leading circle or a rotor: slow conduction velocity of cardiac action potential, short refractory period, and small wavelength. Meanwhile, wavelength is the product of velocity and refractory period. If the action potential has fast conduction, with a long refractory period and/or conduction pathway shorter than the wavelength, an AF focus would not be established. In multiple wavelet theory, a wavefront will break into smaller daughter wavelets when encountering an obstacle, through a process called vortex shedding; but under proper conditions, such wavelets can reform and spin around a centre, forming an AF focus.[50]
In a heart with AF, the increased calcium release from sarcoplasmic reticulum and increased calcium sensitivity can lead to accumulation of intra-cellular calcium and causes down regulation of L-type calcium channels. This reduces the duration of action potential and refractory period, thus favorable for the conduction of re-entrant waves. Increased expression of inward-rectifier potassium ion channels can cause a reduced atrial refractory period and wavelength. The abnormal distribution of gap junction proteins such as GJA1 (also known as Connexin 43), and GJA5 (Connexin 40) causes non-uniformity of electrical conduction, thus causing arrhythmia.[51]
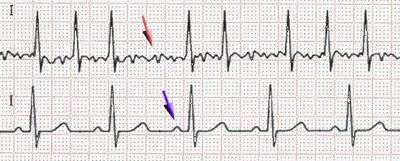
AF can be distinguished from atrial flutter (AFL), which appears as an organized electrical circuit usually in the right atrium. AFL produces characteristic saw-toothed F-waves of constant amplitude and frequency on an ECG whereas AF does not. In AFL, the discharges circulate rapidly at a rate of 300 beats per minute (bpm) around the atrium. In AF, there is no regularity of this kind, except at the sources where the local activation rate can exceed 500 bpm. Although AF and atrial flutter are distinct arrhythmias, atrial flutter may degenerate into AF and an individual may experience both arrhythmias at different times.[12]
Although the electrical impulses of AF occur at a high rate, most of them do not result in a heart beat. A heart beat results when an electrical impulse from the atria passes through the atrioventricular (AV) node to the ventricles and causes them to contract. During AF, if all of the impulses from the atria passed through the AV node, there would be severe ventricular tachycardia, resulting in a severe reduction of cardiac output. This dangerous situation is prevented by the AV node since its limited conduction velocity reduces the rate at which impulses reach the ventricles during AF.[52]
Diagnosis
The evaluation of atrial fibrillation involves a determination of the cause of the arrhythmia, and classification of the arrhythmia. Diagnostic investigation of AF typically includes a complete history and physical examination, ECG, transthoracic echocardiogram, complete blood count, and serum thyroid stimulating hormone level.[22]
Screening
The USPSTF found insufficient evidence to determine the usefulness of screening in 2018.[53] Limited studies have suggested that screening for atrial fibrillation in those 65 years and older increases the number of cases of atrial fibrillation detected.[54]
Minimal evaluation
In general, the minimal evaluation of atrial fibrillation should be performed in all individuals with AF. The goal of this evaluation is to determine the general treatment regimen for the individual. If results of the general evaluation warrant it, further studies may then be performed.
History and physical examination
The history of the individual's atrial fibrillation episodes is probably the most important part of the evaluation. Distinctions should be made between those who are entirely asymptomatic when they are in AF (in which case the AF is found as an incidental finding on an ECG or physical examination) and those who have gross and obvious symptoms due to AF and can pinpoint whenever they go into AF or revert to sinus rhythm.
Routine bloodwork
While many cases of AF have no definite cause, it may be the result of various other problems. Hence, kidney function and electrolytes are routinely determined, as well as thyroid-stimulating hormone (commonly suppressed in hyperthyroidism and of relevance if amiodarone is administered for treatment) and a blood count.[20]
In acute-onset AF associated with chest pain, cardiac troponins or other markers of damage to the heart muscle may be ordered. Coagulation studies (INR/aPTT) are usually performed, as anticoagulant medication may be commenced.[20]
Electrocardiogram
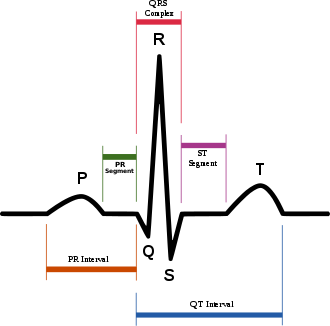
Atrial fibrillation is diagnosed on an electrocardiogram (ECG), an investigation performed routinely whenever an irregular heart beat is suspected. Characteristic findings are the absence of P waves, with disorganized electrical activity in their place, and irregular R–R intervals due to irregular conduction of impulses to the ventricles.[20] At very fast heart rates, atrial fibrillation may look more regular, which may make it more difficult to separate from other supraventricular tachycardias or ventricular tachycardia.[55]
QRS complexes should be narrow, signifying that they are initiated by normal conduction of atrial electrical activity through the intraventricular conduction system. Wide QRS complexes are worrisome for ventricular tachycardia, although, in cases where there is a disease of the conduction system, wide complexes may be present in A-fib with rapid ventricular response.
If paroxysmal AF is suspected but an ECG during an office visit shows only a regular rhythm, AF episodes may be detected and documented with the use of ambulatory Holter monitoring (e.g., for a day). If the episodes are too infrequent to be detected by Holter monitoring with reasonable probability, then the person can be monitored for longer periods (e.g., a month) with an ambulatory event monitor.[20]
Echocardiography
In general, a non-invasive transthoracic echocardiogram (TTE) is performed in newly diagnosed AF, as well as if there is a major change in the person's clinical state. This ultrasound-based scan of the heart may help identify valvular heart disease (which may greatly increase the risk of stroke and alter recommendations for the appropriate type of anticoagulation), left and right atrial size (which indicates likelihood that AF may become permanent), left ventricular size and function, peak right ventricular pressure (pulmonary hypertension), presence of left atrial thrombus (low sensitivity), presence of left ventricular hypertrophy and pericardial disease.[20]
Significant enlargement of both the left and right atria is associated with long-standing atrial fibrillation and, if noted at the initial presentation of atrial fibrillation, suggests that the atrial fibrillation is likely to be of a longer duration than the individual's symptoms.
Extended evaluation
In general, an extended evaluation is not necessary for most individuals with atrial fibrillation and is performed only if abnormalities are noted in the limited evaluation, if a reversible cause of the atrial fibrillation is suggested, or if further evaluation may change the treatment course.
Chest X-ray
In general, a chest X-ray is performed only if a pulmonary cause of atrial fibrillation is suggested, or if other cardiac conditions are suspected (in particular congestive heart failure.) This may reveal an underlying problem in the lungs or the blood vessels in the chest.[20] In particular, if an underlying pneumonia is suggested, then treatment of the pneumonia may cause the atrial fibrillation to terminate on its own.
Transesophageal echocardiogram
A regular echocardiogram (transthoracic echo/TTE) has a low sensitivity for identifying blood clots in the heart. If this is suspected (e.g., when planning urgent electrical cardioversion) a transesophageal echocardiogram/TEE (or TOE where British spelling is used) is preferred.[20]
The TEE has much better visualization of the left atrial appendage than transthoracic echocardiography.[56] This structure, located in the left atrium, is the place where a blood clot forms in more than 90% of cases in non-valvular (or non-rheumatic) atrial fibrillation.[57][58] TEE has a high sensitivity for locating thrombi in this area and can also detect sluggish bloodflow in this area that is suggestive of blood clot formation.[56]
If a blood clot is seen on TEE, then cardioversion is contraindicated due to the risk of stroke and anticoagulation is recommended.
Ambulatory Holter monitoring
A Holter monitor is a wearable ambulatory heart monitor that continuously monitors the heart rate and heart rhythm for a short duration, typically 24 hours. In individuals with symptoms of significant shortness of breath with exertion or palpitations on a regular basis, a Holter monitor may be of benefit to determine whether rapid heart rates (or unusually slow heart rates) during atrial fibrillation are the cause of the symptoms.
Exercise stress testing
Some individuals with atrial fibrillation do well with normal activity but develop shortness of breath with exertion. It may be unclear whether the shortness of breath is due to a blunted heart rate response to exertion caused by excessive atrioventricular node-blocking agents, a very rapid heart rate during exertion, or other underlying conditions such as chronic lung disease or coronary ischemia. An exercise stress test will evaluate the individual's heart rate response to exertion and determine if the AV node blocking agents are contributing to the symptoms.
Classification
| AF category | Defining characteristics |
|---|---|
| First detected | only one diagnosed episode |
| Paroxysmal | recurrent episodes that stop on their own in less than 7 days |
| Persistent | recurrent episodes that last more than 7 days |
| Permanent | an ongoing long-term episode |
The American College of Cardiology (ACC), American Heart Association (AHA), and the European Society of Cardiology (ESC) recommend in their guidelines the following classification system based on simplicity and clinical relevance.[20]
All people with AF are initially in the category called first detected AF. These people may or may not have had previous undetected episodes. If a first detected episode stops on its own in less than 7 days and then another episode begins, later on, the category changes to paroxysmal AF. Although people in this category have episodes lasting up to 7 days, in most cases of paroxysmal AF the episodes will stop in less than 24 hours. If the episode lasts for more than 7 days, it is unlikely to stop on its own, and is then known as persistent AF. In this case, cardioversion can be used to stop the episode. If cardioversion is unsuccessful or not attempted and the episode continues for a long time (e.g., a year or more), the person's AF is then known as permanent.[59]
Episodes that last less than 30 seconds are not considered in this classification system. Also, this system does not apply to cases where the AF is a secondary condition that occurs in the setting of a primary condition that may be the cause of the AF.
About half of people with AF have permanent AF, while a quarter have paroxysmal AF, and a quarter have persistent AF.[4]
In addition to the above four AF categories, which are mainly defined by episode timing and termination, the ACC/AHA/ESC guidelines describe additional AF categories in terms of other characteristics of the person.[20]
- Lone atrial fibrillation (LAF) – absence of clinical or echocardiographic findings of other cardiovascular disease (including hypertension), related pulmonary disease, or cardiac abnormalities such as enlargement of the left atrium, and age under 60 years
- Nonvalvular AF – absence of rheumatic mitral valve disease, a prosthetic heart valve, or mitral valve repair
- Secondary AF – occurs in the setting of a primary condition that may be the cause of the AF, such as acute myocardial infarction, cardiac surgery, pericarditis, myocarditis, hyperthyroidism, pulmonary embolism, pneumonia, or other acute pulmonary disease
Lastly, atrial fibrillation is also classified by whether or not it is caused by valvular heart disease. Valvular atrial fibrillation refers to atrial fibrillation attributable to moderate to severe mitral valve stenosis or atrial fibrillation in the presence of a mechanical artificial heart valve.[60] This distinction is necessary since it has implications on appropriate treatment including differing recommendations for anticoagulation.
Management
The main goals of treatment are to prevent circulatory instability and stroke. Rate or rhythm control are used to achieve the former, whereas anticoagulation is used to decrease the risk of the latter.[61] If cardiovascularly unstable due to uncontrolled tachycardia, immediate cardioversion is indicated.[20] Regular, moderate-intensity exercise is beneficial for people with AF as is weight loss. A number of antiarrhythmics when used long term increase the risk of death without any meaningful benefit.[62]
Anticoagulants
Anticoagulation can be used to reduce the risk of stroke from AF. Anticoagulation is recommended in most people other than those at low risk of stroke[63] or those at high risk of bleeding. The risk of falls and consequent bleeding in frail elderly people should not be considered a barrier to initiating or continuing anticoagulation since the risk of fall-related brain bleeding is low and the benefit of stroke prevention often outweighs the risk of bleeding.[64][65] Oral anticoagulation is underused in atrial fibrillation while aspirin is overused in many who should be treated with a direct oral anticoagulants (DOACs) or warfarin.[66][67][68] In 2019, DOACs were often recommended over warfarin by the American Heart Association.[69]
The risk of stroke from non-valvular AF can be estimated using the CHA2DS2-VASc score. In the 2019 AHA/ACC/HRS guidelines anticoagulation is recommended in non-valvular AF if there is a score of 2 or more in men and 3 or more in women, and may be considered if there is a score of 1 in men or 2 in women, and not using anticoagulation is reasonable if there is a score of 0 in men or 1 in women.[69] Guidelines from the American College of Chest Physicians, Asia-Pacific Heart Rhythm Society, Canadian Cardiovascular Society, European Society of Cardiology, Japanese Circulation Society, Korean Heart Rhythm Society, and the National Institute for Health and Care Excellence recommend the use of novel oral anticoagulants or warfarin with a CHADS2VASC score of 1 over aspirin and some directly recommend against aspirin.[68][70][71][72][73][74][75][76] Experts generally advocate for most people with atrial fibrillation with CHA2DS2-VASc score scores of 1 or more receiving anticoagulation though aspirin is sometimes used for people with a score of 1 (moderate risk for stroke).[66] There is little evidence to support the idea that the use of aspirin significantly reduces the risk of stroke in people with atrial fibrillation.[66] Furthermore, aspirin's major bleeding risk (including bleeding in the brain) is similar to that of warfarin and DOACs despite its inferior efficacy.[67][74]
Anticoagulation can be achieved through a number of means including warfarin,[77] heparin, dabigatran, rivaroxaban,[78] edoxaban,[79] and apixaban.[80] A number of issues should be considered, including the cost of DOACs, risk of stroke, risk of falls, comorbidities (such as chronic liver or kidney disease), the presence of significant mitral stenosis or mechanical heart valves, compliance, and speed of desired onset of anticoagulation.[60][81]
For those with non-valvular atrial fibrillation, DOACs (rivaroxaban, dabigatran, apixaban) are at least as effective as warfarin for preventing strokes and blood clots embolizing to the systemic circulation (if not more so) and are generally preferred over warfarin.[60][82][83][84] DOACs carry a lower risk of bleeding in the brain compared to warfarin,[65] although dabigatran is associated with a higher risk of intestinal bleeding.[82][83] Dual antiplatelet therapy with aspirin and clopidogrel is inferior to warfarin for preventing strokes and has comparable bleeding risk in people with atrial fibrillation.[85] In those who are also on aspirin, however, DOACs appear to be better than warfarin.[86]
Warfarin is the recommended anticoagulant choice for persons with valvular atrial fibrillation (atrial fibrillation in the presence of a mechanical heart valve and/or moderate-severe mitral valve stenosis).[60] The exception to this recommendation is in people with valvular atrial fibrillation who are unable to maintain a therapeutic INR on warfarin therapy; in such cases, treatment with a DOAC is then recommended.[60]
Rate versus rhythm control
There are two ways to approach atrial fibrillation using medications: rate control and rhythm control. Both methods have similar outcomes.[87] Rate control lowers the heart rate closer to normal, usually 60 to 100 bpm, without trying to convert to a regular rhythm. Rhythm control tries to restore a normal heart rhythm in a process called cardioversion and maintains the normal rhythm with medications. Studies suggest that rhythm control is more important in the acute setting AF, whereas rate control is more important in the chronic phase.
The risk of stroke appears to be lower with rate control versus attempted rhythm control, at least in those with heart failure.[88] AF is associated with a reduced quality of life, and, while some studies indicate that rhythm control leads to a higher quality of life, some did not find a difference.[89]
Neither rate nor rhythm control is superior in people with heart failure when they are compared in various clinical trials. However, rate control is recommended as the first line treatment regimen for people with heart failure. On the other hand, rhythm control is only recommended when people experience persistent symptoms despite adequate rate control therapy.[90]
In those with a fast ventricular response, intravenous magnesium significantly increases the chances of successful rate and rhythm control in the urgent setting without major side-effects.[91] A person with poor vital signs, mental status changes, preexcitation, or chest pain often will go to immediate treatment with synchronized DC cardioversion.[20] Otherwise the decision of rate control versus rhythm control using drugs is made. This is based on a number of criteria that includes whether or not symptoms persist with rate control.
Rate control
Rate control to a target heart rate of less than 110 beats per minute is recommended in most people.[92] Lower heart rates may be recommended in those with left ventricular hypertrophy or reduced left ventricular function.[93] Rate control is achieved with medications that work by increasing the degree of block at the level of the AV node, decreasing the number of impulses that conduct into the ventricles. This can be done with:[20][94]
- Beta blockers (preferably the "cardioselective" beta blockers such as metoprolol, bisoprolol, or nebivolol)
- Non-dihydropyridine calcium channel blockers (e.g., diltiazem or verapamil)
- Cardiac glycosides (e.g., digoxin) – have less use, apart from in older people who are sedentary. They are not as effective as either beta blockers or calcium channel blockers.[5]
In those with chronic disease either beta blockers or calcium channel blockers are recommended.[92]
In addition to these agents, amiodarone has some AV node blocking effects (in particular when administered intravenously), and can be used in individuals when other agents are contraindicated or ineffective (particularly due to hypotension).
Cardioversion
Cardioversion is the attempt to switch an irregular heartbeat to a normal heartbeat using electrical or chemical means.[20]
- Electrical cardioversion involves the restoration of normal heart rhythm through the application of a DC electrical shock. Exact placement of the pads does not appear to be important.[95]
- Chemical cardioversion is performed with medications, such as amiodarone, dronedarone,[96] procainamide (especially in pre-excited atrial fibrillation), dofetilide, ibutilide, propafenone, or flecainide.
After successful cardioversion the heart may be in a stunned state, which means that there is a normal rhythm but restoration of normal atrial contraction has not yet occurred.[97]
Surgery
Ablation
In young people with little-to-no structural heart disease where rhythm control is desired and cannot be maintained by medication or cardioversion, then radiofrequency catheter ablation or cryoablation may be attempted and is preferred over years of drug therapy.[20][98] Although radiofrequency ablation is becoming an accepted intervention in selected younger people, there is currently a lack of evidence that ablation reduces all-cause mortality, stroke, or heart failure.[99] There are two ongoing clinical trials (CABANA [Catheter Ablation Versus Antiarrhythmic Drug Therapy for Atrial Fibrillation] and EAST [Early Therapy of Atrial Fibrillation for Stroke Prevention Trial]) that should provide new information for assessing whether AF catheter ablation is superior to more standard therapy.[100]
The Maze procedure, first performed in 1987, is an effective invasive surgical treatment that is designed to create electrical blocks or barriers in the atria of the heart, forcing electrical impulses that stimulate the heartbeat to travel down to the ventricles. The idea is to force abnormal electrical signals to move along one, uniform path to the lower chambers of the heart (ventricles), thus restoring the normal heart rhythm.[101] People with AF often undergo cardiac surgery for other underlying reasons and are frequently offered concomitant AF surgery to reduce the frequency of short- and long-term AF. Concomitant AF surgery are more likely to be free from atrial fibrillation and off medications three months after surgery, but these same people are more likely to need a pacemaker following the procedure.[102]
AF often occurs after cardiac surgery and is usually self-limiting. It is strongly associated with age, preoperative hypertension, and the number of vessels grafted. Measures should be taken to control hypertension preoperatively to reduce the risk of AF. Also, people with a higher risk of AF, e.g., people with pre-operative hypertension, more than 3 vessels grafted, or greater than 70 years of age, should be considered for prophylactic treatment. Postoperative pericardial effusion is also suspected to be the cause of atrial fibrillation. Prophylaxis may include prophylactic postoperative rate and rhythm management. Some authors perform posterior pericardiotomy to reduce the incidence of postoperative AF.[103] When AF occurs, management should primarily be rate and rhythm control. However, cardioversion may be employed if the person is hemodynamically unstable, highly symptomatic, or persists for 6 weeks after discharge. In persistent cases, anticoagulation should be used.
Left atrial appendage occlusion
There is tentative evidence that left atrial appendage occlusion therapy may reduce the risk of stroke in people with non-valvular AF as much as warfarin.[104]
After surgery
After catheter ablation, people are moved to a cardiac recovery unit, intensive care unit, or cardiovascular intensive care unit where they are not allowed to move for 4–6 hours. Minimizing movement helps prevent bleeding from the site of the catheter insertion. The length of time people stay in hospital varies from hours to days. This depends on the problem, the length of the operation and whether or not general anaesthetic was used. Additionally, people should not engage in strenuous physical activity – to maintain a low heart rate and low blood pressure – for around six weeks.[100]
Prognosis
Atrial fibrillation increases the risk of heart failure by 11 per 1000, kidney problems by 6 per 1000, death by 4 per 1000, stroke by 3 per 1000, and coronary heart disease by 1 per 1000.[105] Women have a worse outcome overall than men.[106] Evidence increasingly suggests that atrial fibrillation is independently associated with a higher risk of developing dementia.[107]
Blood clots
Prediction of embolism
Determining the risk of an embolism causing a stroke is important for guiding the use of anticoagulants. The most accurate clinical prediction rules are:[108]
Both the CHADS2 and the CHA2DS2-VASc score predict future stroke risk in people with A-fib with CHA2DS2-VASc being more accurate. Some that had a CHADS2 score of 0 had a CHA2DS2-VASc score of 3, with a 3.2% annual risk of stroke. Thus a CHA2DS2-VASc score of 0 is considered very low risk.[109]
Mechanism of thrombus formation
In atrial fibrillation, the lack of an organized atrial contraction can result in some stagnant blood in the left atrium (LA) or left atrial appendage (LAA). This lack of movement of blood can lead to thrombus formation (blood clotting). If the clot becomes mobile and is carried away by the blood circulation, it is called an embolus. An embolus proceeds through smaller and smaller arteries until it plugs one of them and prevents blood from flowing through the artery. This process results in end organ damage due to loss of nutrients, oxygen, and removal of cellular waste products. Emboli in the brain may result in an ischemic stroke or a transient ischemic attack (TIA).
More than 90% of cases of thrombi associated with non-valvular atrial fibrillation evolve in the left atrial appendage.[57] However, the LAA lies in close relation to the free wall of the left ventricle and thus the LAA's emptying and filling, which determines its degree of blood stagnation, may be helped by the motion of the wall of the left ventricle, if there is good ventricular function.[110]
Dementia
Atrial fibrillation has been independently associated with a higher risk of dementia.[107] Several mechanisms for this association have been proposed including silent small blood clots (subclinical microthrombi) traveling to the brain resulting in small ischemic strokes without symptoms, altered blood flow to the brain, inflammation, and genetic factors.[107] Effective anticoagulation with direct oral anticoagulants or warfarin appears to be protective against AF-associated dementia and evidence of silent ischemic strokes on MRI.[107]
Epidemiology
Atrial fibrillation is the most common arrhythmia.[20] In Europe and North America, as of 2014, it affects about 2% to 3% of the population.[4] This is an increase from 0.4 to 1% of the population around 2005.[20] In the developing world, rates are about 0.6% for males and 0.4% for females.[4] The number of people diagnosed with AF has increased due to better detection of silent AF and increasing age and conditions that predispose to it.[18]
It also accounts for one-third of hospital admissions for cardiac rhythm disturbances,[20] and the rate of admissions for AF has risen in recent years.[111] Strokes from AF account for 20–30% of all ischemic strokes.[18] After a transient ischemic attack or stroke about 11% are found to have a new diagnosis of atrial fibrillation.[112] Between 3 and 11% of those with AF have structurally normal hearts.[113] Approximately 2.2 million individuals in the United States and 4.5 million in the European Union have AF.[20]
The number of new cases each year of atrial fibrillation increases with age. In individuals over the age of 80, it affects about 8%.[20] As of 2001 it was anticipated that in developed countries, the number of people with atrial fibrillation was likely to increase during the following 50 years, owing to the growing proportion of elderly individuals.[114]
Sex
It is more common in men than in women, in European and North American populations.[115] In Asian populations and in both developed and developing countries, there is also a higher rate in men than in women. The risk factors associated with AF are also distributed differently according to sex. In men, coronary disease is more frequent, while in women, high systolic blood pressure or valvular heart disease are more prevalent.[39]
Ethnicity
Rates of AF are lower in populations of African descent than in populations of European descent. The African descent is associated with a protective effect of AF, due to the low presence of SNPs with guanine alleles, in comparison with the European ancestry. European ancestry has more frequent mutations.[39] The variant rs4611994 for the gene PITX2 is associated with risk of AF in African and European populations.[39][42] Other studies reveal that Hispanic and Asian populations have a lower risk of AF compared to populations of European descent. In addition, they demonstrate that the risk of AF in non-European populations is associated with characteristic risk factors of these populations, such as hypertension.[116]
History
Because the diagnosis of atrial fibrillation requires measurement of the electrical activity of the heart, atrial fibrillation was not truly described until 1874, when Edmé Félix Alfred Vulpian observed the irregular atrial electrical behavior that he termed "fremissement fibrillaire" in dog hearts.[117] In the mid-eighteenth century, Jean-Baptiste de Sénac made note of dilated, irritated atria in people with mitral stenosis.[118] The irregular pulse associated with AF was first recorded in 1876 by Carl Wilhelm Hermann Nothnagel and termed "delirium cordis", stating that "[I]n this form of arrhythmia the heartbeats follow each other in complete irregularity. At the same time, the height and tension of the individual pulse waves are continuously changing".[119] Correlation of delirium cordis with the loss of atrial contraction as reflected in the loss of a waves in the jugular venous pulse was made by Sir James MacKenzie in 1904.[120] Willem Einthoven published the first ECG showing AF in 1906.[121] The connection between the anatomic and electrical manifestations of AF and the irregular pulse of delirium cordis was made in 1909 by Carl Julius Rothberger, Heinrich Winterberg, and Sir Thomas Lewis.[122][123][124]
References
- "Atrial fibrillation or flutter: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 28 May 2019.
- Gray, David (2010). Chamberlain's Symptoms and Signs in Clinical Medicine: An Introduction to Medical Diagnosis (13th ed.). London: Hodder Arnold. pp. 70–71. ISBN 9780340974254.
- Munger, TM; Wu, LQ; Shen, WK (January 2014). "Atrial fibrillation". Journal of Biomedical Research. 28 (1): 1–17. doi:10.7555/JBR.28.20130191. PMC 3904170. PMID 24474959.
- Zoni-Berisso, M; Lercari, F; Carazza, T; Domenicucci, S (2014). "Epidemiology of atrial fibrillation: European perspective". Clinical Epidemiology. 6: 213–20. doi:10.2147/CLEP.S47385. PMC 4064952. PMID 24966695.
- Anumonwo, JM; Kalifa, J (November 2014). "Risk Factors and Genetics of Atrial Fibrillation". Cardiology Clinics. 32 (4): 485–94. doi:10.1016/j.ccl.2014.07.007. PMID 25443231.
- Nguyen, TN; Hilmer, SN; Cumming, RG (10 September 2013). "Review of epidemiology and management of atrial fibrillation in developing countries". International Journal of Cardiology. 167 (6): 2412–20. doi:10.1016/j.ijcard.2013.01.184. PMID 23453870.
- Staerk, L; Sherer, JA; Ko, D; Benjamin, EJ; Helm, RH (April 2017). "Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes". Circulation Research (Review). 120 (9): 1501–17. doi:10.1161/CIRCRESAHA.117.309732. PMC 5500874. PMID 28450367.
- Ferguson C, Inglis SC, Newton PJ, Middleton S, Macdonald PS, Davidson PM (2013). "Atrial fibrillation: stroke prevention in focus". ACC. 27 (2): 92–98. doi:10.1016/j.aucc.2013.08.002. PMID 24054541.
- Hui, David; Leung, Alexander A.; Padwal, Raj (2015). Approach to Internal Medicine: A Resource Book for Clinical Practice. Springer. p. 45. ISBN 9783319118215. Archived from the original on 8 September 2017.
- GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- "Heart Disease Other Related Conditions". cdc.gov. 3 September 2014. Archived from the original on 14 February 2015. Retrieved 19 February 2015.
- Bun, Sok-Sithikun; Latcu, Decebal Gabriel; Marchlinski, Francis; Saoudi, Nadir (2 April 2015). "Atrial flutter: more than just one of a kind". European heart journal. Oxford University Press (OUP). 36 (35): 2356–2363. doi:10.1093/eurheartj/ehv118. ISSN 0195-668X. PMID 25838435.
- Richard D. Urman; Linda S. Aglio; Robert W. Lekowski, eds. (2015). Essential clinical anesthesia review : keywords, questions and answers for the boards. p. 480. ISBN 9781107681309. Archived from the original on 8 September 2017.
- Mischke, K; Knackstedt, C; Marx, N; Vollmann, D (April 2013). "Insights into atrial fibrillation". Minerva Medica. 104 (2): 119–30. PMID 23514988.
- Oishi, ML; Xing, S (February 2013). "Atrial fibrillation: management strategies in the emergency department". Emergency Medicine Practice. 15 (2): 1–26, quiz 27. PMID 23369365.
- Amerena, JV; Walters, TE; Mirzaee, S; Kalman, JM (4 November 2013). "Update on the management of atrial fibrillation". The Medical Journal of Australia. 199 (9): 592–97. doi:10.5694/mja13.10191. PMID 24182224.
- Freedman, B; Potpara, TS; Lip, GY (20 August 2016). "Stroke prevention in atrial fibrillation". Lancet. 388 (10046): 806–17. doi:10.1016/S0140-6736(16)31257-0. PMID 27560276.
- Kirchhof, Paulus; Benussi, Stefano (27 August 2016). "2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS". European Heart Journal. 37 (38): 2893–962. doi:10.1093/eurheartj/ehw210. PMID 27567408.
- Steinberg, BA; Piccini, JP (14 April 2014). "Anticoagulation in atrial fibrillation". BMJ (Clinical Research Ed.). 348: g2116. doi:10.1136/bmj.g2116. PMC 4688652. PMID 24733535.
- Fuster, Valentin (2006). "ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (7): e257–354. doi:10.1161/CIRCULATIONAHA.106.177292. PMID 16908781.
- GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- Gutierrez C, Blanchard DG (January 2011). "Atrial Fibrillation: Diagnosis and Treatment". Am Fam Physician (Review). 83 (1): 61–68. PMID 21888129. Archived from the original on 24 December 2013.
- Abed HS, Wittert GA (November 2013). "Obesity and atrial fibrillation". Obesity Reviews. 14 (11): 929–38. doi:10.1111/obr.12056. PMID 23879190.
- Magnani JW, Hylek EM, Apovian CM (23 July 2013). "Obesity begets atrial fibrillation: a contemporary summary". Circulation. 128 (4): 401–05. doi:10.1161/CIRCULATIONAHA.113.001840. PMC 3866045. PMID 23877062.
- Palmeiro C, Davila MI, Bhat M, Frishman WH, Weiss IA (December 2013). "Subclinical hyperthyroidism and cardiovascular risk: recommendations for treatment". Cardiology in Review. 21 (6): 300–08. doi:10.1097/CRD.0b013e318294f6f1. PMID 23563523.
- Cheng, M; Hu, Z; Lu, X; Huang, J; Gu, D (April 2014). "Caffeine intake and atrial fibrillation incidence: dose response meta-analysis of prospective cohort studies". The Canadian Journal of Cardiology. 30 (4): 448–54. doi:10.1016/j.cjca.2013.12.026. PMID 24680173.
- Tonelo D, Providência R, Gonçalves L (August 2013). "Holiday heart syndrome revisited after 34 years". Arquivos Brasileiros de Cardiologia. 101 (2): 183–89. doi:10.5935/abc.20130153. PMC 3998158. PMID 24030078.
- Kuipers, S; Klein Klouwenberg, PM; Cremer, OL (December 2014). "Incidence, risk factors and outcomes of new-onset atrial fibrillation in patients with sepsis: a systematic review". Critical Care (Systematic Review). 18 (6): 688. doi:10.1186/s13054-014-0688-5. PMC 4296551. PMID 25498795.
- Walkey, AJ; Hogarth, DK; Lip, GYH (October 2015). "Optimizing atrial fibrillation management: from ICU and beyond". Chest (Review). 148 (4): 859–64. doi:10.1378/chest.15-0358. PMC 4594627. PMID 25951122.
- Wilhelm, M (August 2014). "Atrial fibrillation in endurance athletes". European Journal of Preventive Cardiology. 21 (8): 1040–48. doi:10.1177/2047487313476414. PMID 23610454.
- Elliot, Adrian D; Mahajan, Rajiv (5 January 2016). "Exercise Training and Atrial Fibrillation Further Evidence for the Importance of Lifestyle Change". Circulation. 133 (5): 457–59. doi:10.1161/CIRCULATIONAHA.115.020800. PMID 26733608.
- Du, X; Dong, J; Ma, C (April 2017). "Is Atrial Fibrillation a Preventable Disease?". Journal of the American College of Cardiology (Review). 69 (15): 1968–82. doi:10.1016/j.jacc.2017.02.020. PMID 28408027.
- Fox CS, Parise H, D'Agostino RB, et al. (2004). "Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring". JAMA. 291 (23): 2851–55. doi:10.1001/jama.291.23.2851. PMID 15199036.
- Roberts JD, Gollob MH (2014). "A contemporary review on the genetic basis of atrial fibrillation". Methodist Debakey Cardiovasc J. 10 (1): 18–24. doi:10.14797/mdcj-10-1-18. PMC 4051329. PMID 24932358.
- Howlett PJ, Hatch FS, Alexeenko V, Jabr RI, Leatham EW, Fry CH (2015). "Diagnosing Paroxysmal Atrial Fibrillation: Are Biomarkers the Solution to This Elusive Arrhythmia?". Biomed Res Int. 2015: 910267. doi:10.1155/2015/910267. PMC 4502272. PMID 26229966.
- Saffitz JE (2006). "Connexins, conduction, and atrial fibrillation". N. Engl. J. Med. 354 (25): 2712–14. doi:10.1056/NEJMe068088. PMID 16790707.
- "OMIM Online Mendelian Inheritance of Man". The National Center for Biotechnology Information. Archived from the original on 16 June 2013. Retrieved 24 August 2010.
- Shimizu W (2013). "Atrial fibrillation and genetic abnormalities". Nihon Rinsho. 71 (1): 161–66.
- Staerk L, Sherer J, Ko D, Benjamin E (2017). "Atrial Fibrillation. Epidemiology, Pathophysiology, and Clinical Outcomes". Circulation Research. 120 (9): 1501–1517. doi:10.1161/CIRCRESAHA.117.309732. PMC 5500874. PMID 28450367.
- Gollob MH, Jones DL, Krahn AD (2006). "Somatic mutations in the connexin 40 gene (GJA5) in atrial fibrillation". New England Journal of Medicine. 354 (25): 2677–2688. doi:10.1056/NEJMoa052800. PMID 16790700.
- Shoemaker MB, Bollman A, Lubitz SA (2015). "Common genetic variants and response to atrial fibrillation ablation". Circulation: Arrhythmia and Electrophysiology. 8 (2): 296–302. doi:10.1161/CIRCEP.114.001909. PMC 4731871. PMID 25684755.
- Roselli C, Chafin M, Weng L (2018). "Multi-ethnic genome-wide association study for atrial fibrillation". Nature Genetics. 50 (9): 1225–1233. doi:10.1038/s41588-018-0133-9. PMC 6136836. PMID 29892015.
- Thorp AA, Owen N, Neuhaus M, Dunstan DW (2011). "Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011". American Journal of Preventive Medicine. 41 (2): 207–2015. doi:10.1016/j.amepre.2011.05.004. PMID 21767729.
- Mohanty S, Mohanty P, Tamaki M (2016). "Differential association of exercise intensity with risk of atrial fibrillation in men and women: evidence from a meta-analysis". Journal of Cardiovascular Electrophysiology. 27 (9): 1021–1029. doi:10.1111/jce.13023. PMID 27245609.
- Abdulla J, Nielsen JR (2009). "Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis". Europace. 11 (9): 1156–1159. doi:10.1093/europace/eup197. PMID 19633305.
- D'Andrea A, Riegler L, Cocchia R (2010). "Left atrial volume index in highly trained athletes". American Heart Journal. 159 (6): 1155–1161. doi:10.1016/j.ahj.2010.03.036. PMID 20569734.
- Alonso A, Krijthe BP, Aspelund T (2013). "Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium". Journal of the American Heart Association. 2 (2): 102. doi:10.1161/JAHA.112.000102. PMC 3647274. PMID 23537808.
- Levitzky YS, Guo CY, Rong J (2008). "Relation of smoking status to a panel of inflammatory markers: the framingham offspring". Journal of the American Heart Association. 201 (1): 217–224. doi:10.1016/j.atherosclerosis.2007.12.058. PMC 2783981. PMID 18289552.
- Goette A, Lendeckel U, Kuchenbecker A (2007). "Cigarette smoking induces atrial fibrosis in humans via nicotine". Heart. 93 (9): 1056–1063. doi:10.1136/hrt.2005.087171. PMC 1955003. PMID 17395670.
- Waks, Jonathan W; Josephson, Mark E (August 2015). "Mechanisms of Atrial Fibrillation – Reentry, Rotors and Reality". Arrythmia and Electrophysiology Review. 3 (2): 90–100. doi:10.15420/aer.2014.3.2.90. PMC 4711504. PMID 26835073.
- Pellman, J; Sheikh, F (April 2015). "Atrial fibrillation: mechanisms, therapeutics, and future directions". Comprehensive Physiology. 5 (2): 649–65. doi:10.1002/cphy.c140047. PMC 5240842. PMID 25880508.
- Klabunde, Richard (2005). Cardiovascular Physiology Concepts. Lippincott Williams & Wilkins. pp. 25, 28. ISBN 9780781750301.
- US Preventive Services Task, Force.; Curry, SJ; Krist, AH; Owens, DK; Barry, MJ; Caughey, AB; Davidson, KW; Doubeni, CA; Epling JW, Jr; Kemper, AR; Kubik, M; Landefeld, CS; Mangione, CM; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (7 August 2018). "Screening for Atrial Fibrillation With Electrocardiography: US Preventive Services Task Force Recommendation Statement". JAMA. 320 (5): 478–484. doi:10.1001/jama.2018.10321. PMID 30088016.
- Moran, PS; Teljeur, C; Ryan, M; Smith, SM (June 2016). "Systematic screening for the detection of atrial fibrillation". The Cochrane Database of Systematic Reviews. 6 (6): CD009586. doi:10.1002/14651858.CD009586.pub3. PMID 27258214.
- Issa ZF, Miller JM, Zipes DP (2009). Clinical arrhythmology and electrophysiology : a companion to Braunwald's heart disease. Philadelphia: Saunders. p. 221. ISBN 9781416059981. Archived from the original on 8 September 2017.
- Romero, J; Cao, JJ; Garcia, MJ; Taub, CC (August 2014). "Cardiac imaging for assessment of left atrial appendage stasis and thrombosis". Nature Reviews. Cardiology. 11 (8): 470–80. doi:10.1038/nrcardio.2014.77. PMID 24913058.
- Blackshear JL, Odell JA (February 1996). "Appendage ligation to reduce stroke in cardiac surgical patients with atrial fibrillation". Ann. Thorac. Surg. 61 (2): 755–59. doi:10.1016/0003-4975(95)00887-X. PMID 8572814.
- Ramlawi, B; Abu Saleh, WK; Edgerton, J (2015). "The Left Atrial Appendage: Target for Stroke Reduction in Atrial Fibrillation". Methodist DeBakey Cardiovascular Journal. 11 (2): 100–03. doi:10.14797/mdcj-11-2-100. PMC 4547664. PMID 26306127.
- Levy S (2000). "Classification system of atrial fibrillation". Current Opinion in Cardiology. 15 (1): 54–57. doi:10.1097/00001573-200001000-00007. PMID 10666661.
- January, CT; Wann, LS; Calkins, H; Field, ME; Chen, LY; Furie, KL; Cigarroa, JE; Heidenreich, PA; Cleveland, JC Jr; Murray, KT; Ellinor, PT; Shea, JB; Ezekowitz, MD; Tracy, CM; Yancy, CW (January 2019). "2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Heart Rhythm (Review). S1547-5271 (19): 30037–2. doi:10.1016/j.hrthm.2019.01.024. PMID 30703530.
- Prystowsky, Eric N; Padanilam, Benzy J; Fogel, MD, Richard I (21 July 2015). "Treatment of Atrial Fibrillation". JAMA. 314 (3): 278–88. doi:10.1001/jama.2015.7505. PMID 26197188.
- Valembois, L; Audureau, E; Takeda, A; Jarzebowski, W; Belmin, J; Lafuente-Lafuente, C (4 September 2019). "Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation". The Cochrane Database of Systematic Reviews. 9: CD005049. doi:10.1002/14651858.CD005049.pub5. PMC 6738133. PMID 31483500.
- Lip, GY; Lane, DA (19 May 2015). "Stroke prevention in atrial fibrillation: a systematic review". JAMA. 313 (19): 1950–62. doi:10.1001/jama.2015.4369. PMID 25988464.
- Zarraga, IG; Kron, J (January 2013). "Oral anticoagulation in elderly adults with atrial fibrillation: integrating new options with old concepts". Journal of the American Geriatrics Society. 61 (1): 143–50. doi:10.1111/jgs.12042. PMID 23252345.
- Kundu, A; Sardar, P; Chatterjee, S; Aronow, WS; Owan, T; Ryan, JJ (July 2016). "Minimizing the Risk of Bleeding with NOACs in the Elderly". Drugs & Aging. 33 (7): 491–500. doi:10.1007/s40266-016-0376-z. PMID 27174293.
- Morin, DP; Bernard, ML; Madias, C; Rogers, PA; Thihalolipavan, S; Estes 3rd, NA (December 2016). "The State of the Art: Atrial Fibrillation Epidemiology, Prevention, and Treatment". Mayo Clinic Proceedings. 91 (12): 1778–810. doi:10.1016/j.mayocp.2016.08.022. PMID 27825618.
- Freedman, B; Potpara, TS; Lip, GY (August 2016). "Stroke prevention in atrial fibrillation". The Lancet (Review). 388 (10046): 806–17. doi:10.1016/S0140-6736(16)31257-0. PMID 27560276.
- Andrade, JG; Macle, L; Nattel, S; Verma, A; Cairns, J (August 2017). "Contemporary Atrial Fibrillation Management: A Comparison of the Current AHA/ACC/HRS, CCS, and ESC Guidelines". The Canadian Journal of Cardiology (Review). 33 (8): 965–76. doi:10.1016/j.cjca.2017.06.002. PMID 28754397.
- January, CT; Wann, LS; Calkins, H; Chen, LY; Cigarroa, JE; Cleveland JC, Jr; Ellinor, PT; Ezekowitz, MD; Field, ME; Furie, KL; Heidenreich, PA; Murray, KT; Shea, JB; Tracy, CM; Yancy, CW (28 January 2019). "2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation". Circulation. 140 (2): e125–e151. doi:10.1161/CIR.0000000000000665. PMID 30686041.
- JCS Joint Working Group; Inoue, H; Atarashi, H; Kamakura, S; Koretsune, Y (August 2014). "Guidelines for Pharmacotherapy of Atrial Fibrillation (JCS 2013)". Circulation Journal (Review). 78 (8): 1997–2021. doi:10.1253/circj.cj-66-0092. PMID 24965079.
- Jung, BC; Kim, NH; Nam, GB; Park, HW; On, YK (January 2015). "The Korean Heart Rhythm Society's 2014 Statement on Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation: Korean Heart Rhythm Society". Korean Circulation Journal (Review). 45 (1): 9–19. doi:10.4070/kcj.2015.45.1.9. PMC 4310986. PMID 25653698.
- You, JJ; Singer, DE; Howard, PA; Lane, DA; Eckman, MH (February 2012). "Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest (Review). 141 (Supplement 2): e531S–75S. doi:10.1378/chest.11-2304. PMC 3278056. PMID 22315271.
- Chiang, CE; Okumura, K; Zhang, S; Chao, TF; Siu, CW (August 2017). "2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation". Journal of Arrhythmia (Review). 33 (4): 345–67. doi:10.1016/j.joa.2017.05.004. PMC 5529598. PMID 28765771.
- Kirchhof, P; Benussi, S; Kotecha, D; Ahlsson, A; Atar, D (October 2016). "2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS". European Heart Journal (Review). 37 (38): 2893–962. doi:10.1093/eurheartj/ehw210. PMID 27567408.
- Macle, L; Cairns, J; Leblanc, K; Tsang, T; Skanes, A (October 2016). "2016 Focused Update of the Canadian Cardiovascular Society Guidelines for the Management of Atrial Fibrillation". The Canadian Journal of Cardiology. 32 (10): 1170–85. doi:10.1016/j.cjca.2016.07.591. PMID 27609430.
- National Institute of Health Care and Excellence. "Atrial fibrillation: management".
- Ciervo CA, Granger CB, Schaller FA (September 2012). "Stroke prevention in patients with atrial fibrillation: disease burden and unmet medical needs". J Am Osteopath Assoc (Review). 112 (9 (Suppl 2)): eS2–8. PMID 23014814. Archived from the original on 5 March 2016.
- "FDA approves Xarelto to prevent stroke in people with common type of abnormal heart rhythm". FDA. Archived from the original on 5 November 2011. Retrieved 4 November 2011.
- "FDA approves anti-clotting drug Savaysa". FDA. 8 January 2015. Archived from the original on 19 June 2016. Retrieved 23 June 2016.
- "FDA approves Eliquis to reduce the risk of stroke, blood clots in patients with non-valvular atrial fibrillation". FDA. Archived from the original on 31 December 2012. Retrieved 30 December 2012.
- Singer DE, Albers GW, Dalen JE, Go AS, Halperin JL, Manning WJ (September 2004). "Antithrombotic Therapy in Atrial Fibrillation : The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy". Chest. 126 (3_suppl): 429S–56S. doi:10.1378/chest.126.3_suppl.429S. PMID 15383480. Retrieved 2 October 2012.
- Sharma, M; Cornelius, VR; Patel, JP; Davies, JG; Molokhia, M (20 May 2015). "Efficacy and Harms of Direct Oral Anticoagulants in the Elderly for Stroke Prevention in Atrial Fibrillation and Secondary Prevention of Venous Thromboembolism: Systematic Review and Meta-Analysis". Circulation. 132 (3): 194–204. doi:10.1161/CIRCULATIONAHA.114.013267. PMC 4765082. PMID 25995317.
- Gómez-Outes, A; Terleira-Fernández, AI; Calvo-Rojas, G; Suárez-Gea, ML; Vargas-Castrillón, E (2013). "Dabigatran, Rivaroxaban, or Apixaban versus Warfarin in Patients with Nonvalvular Atrial Fibrillation: A Systematic Review and Meta-Analysis of Subgroups". Thrombosis. 2013: 640723. doi:10.1155/2013/640723. PMC 3885278. PMID 24455237.
- Sanders, Gillian D.; Lowenstern, Angela; Borre, Ethan; Chatterjee, Ranee; Goode, Adam; Sharan, Lauren; LaPointe, Nancy M. Allen; Raitz, Giselle; Shah, Bimal (30 October 2018). "Stroke Prevention in Patients With Atrial Fibrillation: A Systematic Review Update". doi:10.23970/ahrqepccer214. Cite journal requires
|journal=(help) - Carroll, John D.; Webb, John G. (2012). Structural Heart Disease Interventions. Lippincott Williams & Wilkins. p. PT379. ISBN 9781451153965.
- Bennaghmouch, N; de Veer, AJWM; Bode, K; Mahmoodi, BK; Dewilde, WJM; Lip, GYH; Brueckmann, M; Kleine, E; Ten Berg, JM (13 March 2018). "Efficacy and Safety of the Use of Non-Vitamin K Antagonist Oral Anticoagulants in Patients With Nonvalvular Atrial Fibrillation and Concomitant Aspirin Therapy: A Meta-Analysis of Randomized Trials". Circulation. 137 (11): 1117–1129. doi:10.1161/CIRCULATIONAHA.117.028513. PMID 29101289.
- Al-Khatib, Sana M. (3 June 2014). "Rate- and rhythm-control therapies in patients with atrial fibrillation: a systematic review". Annals of Internal Medicine. 160 (11): 760–73. doi:10.7326/M13-1467. PMID 24887617.
- Frankel, Grace; Kamrul, Rejina; Kosar, Lynette; Jensen, Brent (14 March 2017). "Rate versus rhythm control in atrial fibrillation". Canadian Family Physician. 59 (2): 161–68. ISSN 0008-350X. PMC 3576947. PMID 23418244.
- Thrall G, Lane D, Carroll D, Lip GY (2006). "Quality of life in patients with atrial fibrillation: a systematic review". Am. J. Med. 119 (5): 448.e1–19. doi:10.1016/j.amjmed.2005.10.057. PMID 16651058.
- Trulock, Kevin M; Narayan, Sanjiv M (19 August 2014). "Rhythm Control in Heart Failure Patients With Atrial Fibrillation: Contemporary Challenges Including the Role of Ablation". Journal of the American College of Cardiology. 64 (7): 710–21. doi:10.1016/j.jacc.2014.06.1169. PMID 25125304.
Multiple studies have compared pharmacological rate and rhythm strategies but have failed to identify a superior therapy, a finding that extends to patients with HF. ... Antiarrhythmic drug therapy is indicated as first-line therapy for AF that remains symptomatic despite adequate rate control.
- Onalan O, Crystal E, Daoulah A, Lau C, Crystal A, Lashevsky I (2007). "Meta-analysis of magnesium therapy for the acute management of rapid atrial fibrillation". Am. J. Cardiol. 99 (12): 1726–32. doi:10.1016/j.amjcard.2007.01.057. PMID 17560883.
- Anderson, JL; Halperin, JL; Albert, NM; Bozkurt, B; Brindis, RG; Curtis, LH; DeMets, D; Guyton, RA; Hochman, JS; Kovacs, RJ; Ohman, EM; Pressler, SJ; Sellke, FW; Shen, WK; Wann, LS; Curtis, AB; Ellenbogen, KA; Estes NA, 3rd; Ezekowitz, MD; Jackman, WM; January, CT; Lowe, JE; Page, RL; Slotwiner, DJ; Stevenson, WG; Tracy, CM; Fuster, V; Rydén, LE; Cannom, DS; Crijns, HJ; Curtis, AB; Ellenbogen, KA; Le Heuzey, JY; Kay, GN; Olsson, SB; Prystowsky, EN; Tamargo, JL; Wann, S (7 May 2013). "Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Journal of the American College of Cardiology. 61 (18): 1935–44. doi:10.1016/j.jacc.2013.02.001. PMID 23558044.
- Badheka, AO; Shah, N; Grover, PM; Patel, NJ; Chothani, A; Mehta, K; Singh, V; Deshmukh, A; Savani, GT; Rathod, A; Panaich, SS; Patel, N; Arora, S; Bhalara, V; Coffey, JO; Mitrani, RD; Halperin, JL; Viles-Gonzalez, JF (1 April 2014). "Outcomes in atrial fibrillation patients with and without left ventricular hypertrophy when treated with a lenient rate-control or rhythm-control strategy". The American Journal of Cardiology. 113 (7): 1159–65. doi:10.1016/j.amjcard.2013.12.021. PMID 24507168.
- "Atrial fibrillation: national clinical guideline for management in primary and secondary care" (PDF). National Collaborating Centre for Chronic Conditions. London: Royal College of Physicians. 2006.
- Kirkland, S; Stiell, I; AlShawabkeh, T; Campbell, S; Dickinson, G; Rowe, BH (July 2014). "The efficacy of pad placement for electrical cardioversion of atrial fibrillation/flutter: a systematic review". Academic Emergency Medicine. 21 (7): 717–26. doi:10.1111/acem.12407. PMID 25117151.
- Bramah N. Singh (2007). "Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter". N. Engl. J. Med. 357 (10): 987–99. doi:10.1056/NEJMoa054686. PMID 17804843.
- Watson T, Shantsila E, Lip GY (10 January 2009). "Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited". Lancet. 373 (9658): 155–66. doi:10.1016/S0140-6736(09)60040-4. PMID 19135613.
- Leong-Sit P, Zado E, Callans DJ, et al. (2010). "Efficacy and risk of atrial fibrillation ablation before 45 years of age". Circ Arrhythmia Electrophysiol. 3 (5): 452–57. doi:10.1161/circep.110.938860. PMID 20858861.
- Agency for Healthcare Research and Quality. Research Protocol: Treatment of Atrial Fibrillation. December 2012
- January, CT; Wann, LS; Alpert, JS; Calkins, H; Cigarroa, JE; Cleveland, JC Jr; Conti, JB; Ellinor, PT; Ezekowitz, MD; Field, ME; Murray, KT; Sacco, RL; Stevenson, WG; Tchou, PJ; Tracy, CM; Yancy, CW (28 March 2014). "2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society". Circulation. 130 (23): e199–e267. doi:10.1161/CIR.0000000000000041. PMC 4676081. PMID 24682347. Executive summary: PMID 24682348
- Northwestern Surgery for Atrial Fibrillation. Atrial Fibrillation Surgery Archived 19 April 2012 at the Wayback Machine
- Huffman, Mark D; Karmali, Kunal N; Berendsen, Mark A; Andrei, Adin-Cristian; Kruse, Jane; McCarthy, Patrick M; Malaisrie, S C (22 August 2016). Cochrane Heart Group (ed.). "Concomitant atrial fibrillation surgery for people undergoing cardiac surgery". Cochrane Database of Systematic Reviews (8): CD011814. doi:10.1002/14651858.CD011814.pub2. PMC 5046840. PMID 27551927.
- Kaleda VI, McCormack DJ, Shipolini AR (April 2012). "Does posterior pericardiotomy reduce the incidence of atrial fibrillation after coronary artery bypass grafting surgery?". Interact. Cardiovasc. Thorac. Surg. 14 (4): 384–89. doi:10.1093/icvts/ivr099. PMC 3309809. PMID 22235005.
- Zhou, X; Zhang, W; Lv, W; Zhou, Q; Li, Y; Zhang, L; Lu, Y; Zhang, J; Xing, Q; Wang, H; Tang, B (15 January 2016). "Left atrial appendage occlusion in atrial fibrillation for stroke prevention: A systemic review". International Journal of Cardiology. 203: 55–59. doi:10.1016/j.ijcard.2015.10.011. PMID 26492310.
- Odutayo, Ayodele; Wong, Christopher X; Hsiao, Allan J; Hopewell, Sally; Altman, Douglas G; Emdin, Connor A (6 September 2016). "Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis" (PDF). BMJ. 354: i4482. doi:10.1136/bmj.i4482. PMID 27599725.
- Emdin, CA; Wong, CX; Hsiao, AJ; Altman, DG; Peters, SA; Woodward, M; Odutayo, AA (19 January 2016). "Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies". BMJ (Clinical Research Ed.). 532: h7013. doi:10.1136/bmj.h7013. PMC 5482349. PMID 26786546.
- Rivard, L; Khairy, P (December 2017). "Mechanisms, Clinical Significance, and Prevention of Cognitive Impairment in Patients With Atrial Fibrillation". Canadian Journal of Cardiology (Review). 33 (12): 1556–64. doi:10.1016/j.cjca.2017.09.024. PMID 29173598.
- Lopes RD, Crowley MJ, Shah BR, et al. Stroke Prevention in Atrial Fibrillation. Comparative Effectiveness Review No. 123. AHRQ Publication No. 13-EHC113-EF. Rockville, MD: Agency for Healthcare Research and Quality; August 2013. www.effectivehealthcare.ahrq.gov/ reports/final.cfm.
- Olesen, JB; Torp-Pedersen, C; Hansen, ML; Lip, GY (2012). "The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study". Thromb. Haemost. 107 (6): 1172–79. doi:10.1160/th12-03-0175. PMID 22473219.
- Al-Saady, N. M.; O. A. Abel; A. J. Camm (1999). "Left atrial appendage: structure, function, and role in thromboembolism". Heart. 82 (5): 547–55. doi:10.1136/hrt.82.5.547. PMC 1760793. PMID 10525506.
- Friberg J, Buch P, Scharling H, Gadsbphioll N, Jensen GB (2003). "Rising rates of hospital admissions for atrial fibrillation". Epidemiology. 14 (6): 666–72. doi:10.1097/01.ede.0000091649.26364.c0. PMID 14569181.
- Kishore, A; Vail, A; Majid, A; Dawson, J; Lees, KR; Tyrrell, PJ; Smith, CJ (February 2014). "Detection of atrial fibrillation after ischemic stroke or transient ischemic attack: a systematic review and meta-analysis". Stroke: A Journal of Cerebral Circulation. 45 (2): 520–26. doi:10.1161/STROKEAHA.113.003433. PMID 24385275.
- Sanfilippo AJ, Abascal VM, Sheehan M, Oertel LB, Harrigan P, Hughes RA, Weyman AE (1990). "Atrial enlargement as a consequence of atrial fibrillation A prospective echocardiographic study". Circulation. 82 (3): 792–97. doi:10.1161/01.CIR.82.3.792. PMID 2144217. Archived from the original on 1 December 2009. Retrieved 2 December 2009.
- Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE (May 2001). "Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study". primary source. JAMA. 285 (18): 2370–75. doi:10.1001/jama.285.18.2370. PMID 11343485.
- Schnabel RB, Yin X, Gona P (2015). "50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study". Lancet. 386 (9989): 154–162. doi:10.1016/S0140-6736(14)61774-8. PMC 4553037. PMID 25960110.
- Dewland TA, Olgin JE, Vittinghoff E (2013). "Incident atrial fibrillation among Asians, Hispanics, blacks, and whites". Circulation. 128 (23): 2470–2477. doi:10.1161/CIRCULATIONAHA.113.002449. PMID 24103419.
- Vulpian A (1874). "Note sur les effets de la faradisation directe des ventricules du coeur chez le chien". Archives de Physiologie Normale et Pathologique. 6: 975.
- McMichael J (1982). "History of atrial fibrillation 1628–1819 Harvey – de Senac – Laënnec". Br Heart J. 48 (3): 193–97. doi:10.1136/hrt.48.3.193. PMC 481228. PMID 7049202.
- Nothnagel H (1876). "Ueber arythmische Herzthatigkeit". Deutsches Archiv für Klinische Medizin. 17: 190–220.
- MacKenzie J (1904). "Observations on the Inception of the Rhythm of the Heart by the Ventricle: As the cause of Continuous Irregularity of the Heart". Br Med J. 1 (2253): 529–36. doi:10.1136/bmj.1.2253.529. PMC 2353402. PMID 20761393.
- Einthoven W (1906). "Le telecardiogramme". Archives Internationales de Physiologie. 4: 132–64.
- Rothberger CJ, Winterberg H (1909). "Vorhofflimmern und Arhythmia perpetua". Wiener Klinische Wochenschrift. 22: 839–44.
- Lewis T (1909). "Auricular fibrillation: a common clinical condition". Br Med J. 2 (2552): 1528. doi:10.1136/bmj.2.2552.1528. PMC 2321318. PMID 20764769.
- Flegel KM (1995). "From delirium cordis to atrial fibrillation: historical development of a disease concept". Ann. Intern. Med. 122 (11): 867–73. doi:10.7326/0003-4819-122-11-199506010-00010. PMID 7741373.
External links
| Classification | |
|---|---|
| External resources |
| Wikimedia Commons has media related to Atrial fibrillation. |
- Atrial fibrillation at Curlie
- Wann LS; Curtis AB; Ellenbogen KA; Estes NA; Ezekowitz MD; Jackman WM; January CT; Lowe JE; Page RL; Slotwiner DJ; Stevenson WG; Tracy CM; Fuster V; Rydén LE; Cannom DS; Crijns HJ; Curtis AB; Ellenbogen KA; Halperin JL; Le Heuzey J; Kay GN; Lowe JE; Olsson SB; Prystowsky EN; Tamargo JL (7 May 2013). "Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines". Circulation. 127 (18): 1916–26. doi:10.1161/CIR.0b013e318290826d. PMID 23545139.
- Atrial fibrillation toolkit – American College of Cardiology