Oral microbiology
Oral microbiology is the study of the microorganisms (microbiota) of the oral cavity and their interactions between oral microorganisms or with the host.[1] The environment present in the human mouth is suited to the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature.[2] Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.[2][3]

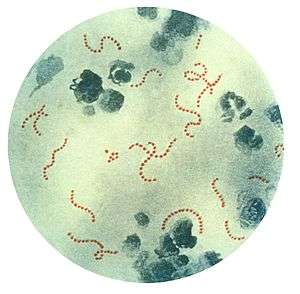
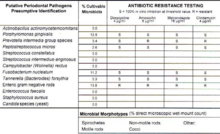
Anaerobic bacteria in the oral cavity include: Actinomyces, Arachnia, Bacteroides, Bifidobacterium, Eubacterium, Fusobacterium, Lactobacillus, Leptotrichia, Peptococcus, Peptostreptococcus, Propionibacterium, Selenomonas, Treponema, and Veillonella.[4] Genera of fungi that are frequently found in the mouth include Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium, and Cryptococcus, among others.[5] Bacteria accumulate on both the hard and soft oral tissues in biofilms. Bacterial adhesion is particularly important for oral bacteria.
Oral bacteria have evolved mechanisms to sense their environment and evade or modify the host. Bacteria occupy the ecological niche provided by both the tooth surface and gingival epithelium. However, a highly efficient innate host defense system constantly monitors the bacterial colonization and prevents bacterial invasion of local tissues. A dynamic equilibrium exists between dental plaque bacteria and the innate host defense system.[6] Of particular interest is the role of oral microorganisms in the two major dental diseases: dental caries and periodontal disease.[6] Additionally, research has correlated poor oral heath and the resulting ability of the oral microbiota to invade the body to affect cardiac health as well as cognitive function.[7]
Oral Microflora
The oral microbiome, mainly comprising bacteria which have developed resistance to the human immune system, has been known to impact the host for its own benefit, as seen with dental cavities. The environment present in the human mouth allows the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature.[2] Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.[2][3]
Anaerobic bacteria in the oral cavity include: Actinomyces, Arachnia, Bacteroides, Bifidobacterium, Eubacterium, Fusobacterium, Lactobacillus, Leptotrichia, Peptococcus, Peptostreptococcus, Propionibacterium, Selenomonas, Treponema, and Veillonella.[4] In addition, there are also a number of fungi found in the oral cavity, including: Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium, and Cryptococcus.[9] The oral cavity of a new-born baby does not contain bacteria but rapidly becomes colonized with bacteria such as Streptococcus salivarius. With the appearance of the teeth during the first year colonization by Streptococcus mutans and Streptococcus sanguinis occurs as these organisms colonise the dental surface and gingiva. Other strains of streptococci adhere strongly to the gums and cheeks but not to the teeth. The gingival crevice area (supporting structures of the teeth) provides a habitat for a variety of anaerobic species. Bacteroides and spirochetes colonize the mouth around puberty.[6] Of particular interest is the role of oral microorganisms in the two major dental diseases: dental caries and periodontal disease.[6]
Niche
The habitat of the oral microbiome is essentially the surfaces of the inside of the mouth. Saliva plays a considerable role in influencing the oral microbiome.[10] More than 800 species of bacteria colonize oral mucous, 1,300 species are found in the gingival crevice, and nearly 1,000 species comprise dental plaque. The mouth is a rich environment for hundreds of species of bacteria since saliva is mostly water and plenty of nutrients pass through the mouth each day. When kissing, it takes only 10 seconds for no less than 80 million bacteria to be exchanged by the passing of saliva. However, the effect is transitory, as each individual quickly returns to their own equilibrium.[11][12]
Thanks to progress in molecular biology techniques, scientific understanding of oral ecology is improving. Oral ecology is being more comprehensively mapped, including the tongue, the teeth, the gums, salivary glands, etc. which are home to these communities of different microorganisms.[13]
The host’s immune system controls the bacterial colonization of the mouth and prevents local infection of tissues. A dynamic equilibrium exists notably between the bacteria of dental plaque and the host’s immune system, enabling the plaque to stay behind in the mouth when other biofilms are washed away.[14]
In equilibrium, the bacterial biofilm produced by the fermentation of sugar in the mouth is quickly swept away by the saliva, except for dental plaque. In cases of imbalance in the equilibrium, oral microorganisms grow out of control and cause oral diseases such as tooth decay and periodontal disease. Several studies have also linked poor oral hygiene to infection by pathogenic bacteria.[15]
Role in Health
There are many factors of oral health which need to be preserved in order to prevent pathogenesis of the oral microbiome or diseases of the mouth. Dental plaque is the material that adheres to the teeth and consists of bacterial cells (mainly S. mutans and S. sanguis), salivary polymers and bacterial extracellular products. Plaque is a biofilm on the surfaces of the teeth. This accumulation of microorganisms subject the teeth and gingival tissues to high concentrations of bacterial metabolites which results in dental disease. If not taken care of, via brushing or flossing, the plaque can turn into tartar (its hardened form) and lead to gingivitis or periodontal disease. In the case of dental cavities, proteins involved in colonization of teeth by Streptococcus mutans can produce antibodies that inhibit the cariogenic process which can be used to create vaccines.[14] Bacteria species typically associated with the oral microbiota have been found to be present in women with bacterial vaginosis.[16] Genera of fungi that are frequently found in the mouth include Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium, and Cryptococcus, among others.[5] Additionally, research has correlated poor oral heath and the resulting ability of the oral microbiota to invade the body to affect cardiac health as well as cognitive function.[7] High levels of circulating antibodies to oral pathogens Campylobacter rectus, Veillonella parvula and Prevotella melaninogenica are associated with hypertension in human.[17]
Importance of Dental Hygiene
Maintaining a balanced oral microflora is important for total wellness. The best way to maintain this environment is with proper oral hygiene. Insufficient brushing and flossing can lead to gum and tooth disease, and eventually tooth loss.[18] In addition, poor dental hygiene has been linked to conditions such as osteoporosis, diabetes and cardiovascular diseases.[18] Some diseases and medications are known to limit salivary flow, making it easier for bacteria to overgrow in the mouth without being washed away. To prevent any possible side effects from poor oral hygiene, it is important to brush and floss every day, schedule regular cleanings, eat a healthy diet and use a recently-replaced toothbrush.[18]
Issues and Areas of Research
The oral environment (temperature, humidity, pH, nutrients, etc.) impacts the selection of adapted (and sometimes pathogenic) populations of microorganisms.[19] For a young person or an adult in good health and with a healthy diet, the microbes living in the mouth adhere to mucous, teeth and gums to resist removal by saliva. Eventually, they are mostly washed away and destroyed during their trip through the stomach.[19][20] Salivary flow and oral conditions vary person-to-person, and also relative to the time of day and whether or not an individual sleeps with their mouth open. From youth to old age, the entire mouth interacts with and affects the oral microbiome.[21] Via the larynx, numerous bacteria can travel through the respiratory tract to the lungs. There, mucous is charged with their removal. Pathogenic oral microflora have been linked to the production of factors which favor autoimmune diseases such as psoriasis and arthritis, as well as cancers of the colon, lungs and breasts.[22]
Intercellular Communication
Most of the bacterial species found in the mouth belong to microbial communities, called biofilms, a feature of which is inter-bacterial communication. Cell–cell contact is mediated by specific protein adhesins and often, as in the case of inter-species aggregation, by complementary polysaccharide receptors. Another method of communication involves cell–cell signalling molecules, which are of two classes: those used for intra-species and those used for inter-species signalling. An example of intra-species communication is quorum sensing. Oral bacteria have been shown to produce small peptides, such as competence stimulating peptides, which can help promote single-species biofilm formation. A common form of inter-species signalling is mediated by 4, 5-dihydroxy-2, 3-pentanedione (DPD), also known as autoinducer-2 (Al-2).[23]
See also
- Biofilms
- Dental plaque
- Environmental microbiology
- Human microbiota
- Human Microbiome Project
- Microbiology
- Theodor Rosebury
- List of bacterial vaginosis microbiota
References
- Schwiertz A (2016). Microbiota of the human body : implications in health and disease. Switzerland: Springer. p. 45. ISBN 978-3-319-31248-4.
- Sherwood L, Willey J, Woolverton C (2013). Prescott's Microbiology (9th ed.). New York: McGraw Hill. pp. 713–721. ISBN 9780073402406. OCLC 886600661.
- Wang ZK, Yang YS, Stefka AT, Sun G, Peng LH (April 2014). "Review article: fungal microbiota and digestive diseases". Alimentary Pharmacology & Therapeutics. 39 (8): 751–66. doi:10.1111/apt.12665. PMID 24612332.
In addition, GI fungal infection is reported even among those patients with normal immune status. Digestive system-related fungal infections may be induced by both commensal opportunistic fungi and exogenous pathogenic fungi. ... Candida sp. is also the most frequently identified species among patients with gastric IFI. ... It was once believed that gastric acid could kill microbes entering the stomach and that the unique ecological environment of the stomach was not suitable for microbial colonisation or infection. However, several studies using culture-independent methods confirmed that large numbers of acid-resistant bacteria belonging to eight phyla and up to 120 species exist in the stomach, such as Streptococcus sp., Neisseria sp. and Lactobacillus sp. etc.26, 27 Furthermore, Candida albicans can grow well in highly acidic environments,28 and some genotypes may increase the severity of gastric mucosal lesions.29
- Sutter VL (1984). "Anaerobes as normal oral flora". Reviews of Infectious Diseases. 6 Suppl 1: S62–6. doi:10.1093/clinids/6.Supplement_1.S62. PMID 6372039.
- Cui L, Morris A, Ghedin E (July 2013). "The human mycobiome in health and disease". Genome Medicine. 5 (7): 63. doi:10.1186/gm467. PMC 3978422. PMID 23899327.
Figure 2: Distribution of fungal genera in different body sites
- Rogers A H (editor). (2008). Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
- Noble JM, Scarmeas N, Papapanou PN (October 2013). "Poor oral health as a chronic, potentially modifiable dementia risk factor: review of the literature". Current Neurology and Neuroscience Reports. 13 (10): 384. doi:10.1007/s11910-013-0384-x. PMC 6526728. PMID 23963608.
- Dorfman J, The Center for Special Dentistry.
- Cui L, Morris A, Ghedin E (2013). "The human mycobiome in health and disease". Genome Medicine. 5 (7): 63. doi:10.1186/gm467. PMC 3978422. PMID 23899327.
- Marsh PD, Do T, Beighton D, Devine DA (February 2016). "Influence of saliva on the oral microbiota". Periodontology 2000. 70 (1): 80–92. doi:10.1111/prd.12098. PMID 26662484.
- Bertrand M (2009-11-26). "DUHL Olga Anna (dir.), Amour, sexualité et médecine aux XVe et XVIe siècles, Dijon, Editions Universitaires de Dijon, 2009". Genre, Sexualité & Société (n°2). doi:10.4000/gss.1001. ISSN 2104-3736.
- Kort R, Caspers M, van de Graaf A, van Egmond W, Keijser B, Roeselers G (December 2014). "Shaping the oral microbiota through intimate kissing". Microbiome. 2 (1): 41. doi:10.1186/2049-2618-2-41. PMC 4233210. PMID 25408893.
- Attar N (March 2016). "Microbial ecology: FISHing in the oral microbiota". Nature Reviews. Microbiology. 14 (3): 132–3. doi:10.1038/nrmicro.2016.21. PMID 26853115.
- Molecular oral microbiology. Rogers, Anthony (Anthony H.). Norfolk, UK: Caister Academic Press. 2008. ISBN 9781904455240. OCLC 170922278.CS1 maint: others (link)
- Noble JM, Scarmeas N, Papapanou PN (October 2013). "Poor oral health as a chronic, potentially modifiable dementia risk factor: review of the literature". Current Neurology and Neuroscience Reports. 13 (10): 384. doi:10.1007/s11910-013-0384-x. PMID 23963608.
- Africa CW, Nel J, Stemmet M (July 2014). "Anaerobes and bacterial vaginosis in pregnancy: virulence factors contributing to vaginal colonisation". International Journal of Environmental Research and Public Health. 11 (7): 6979–7000. doi:10.3390/ijerph110706979. PMC 4113856. PMID 25014248.
- Pietropaoli, Davide; Del Pinto, Rita; Ferri, Claudio; Ortu, Eleonora; Monaco, Annalisa (August 2019). "Definition of hypertension-associated oral pathogens in NHANES". Journal of Periodontology. 90 (8): 866–876. doi:10.1002/JPER.19-0046. ISSN 1943-3670. PMID 31090063.
- "Oral health: A window to your overall health". Mayo Clinic. Retrieved 2019-04-16.
- Linda Sherwood, Joanne Willey and Christopher Woolverton, , New York, McGraw Hill, 2013, 9th ed., p. 713–721
- Wang ZK, Yang YS, Stefka AT, Sun G, Peng LH (April 2014). "Review article: fungal microbiota and digestive diseases". Alimentary Pharmacology & Therapeutics. 39 (8): 751–66. doi:10.1111/apt.12665. PMID 24612332.
- Kerr WJ, Kelly J & Geddes DA (1991) The areas of various surfaces in the human mouth from nine years to adulthood. J Dent Res. 1991 Dec; 70(12):1528-30
- ↑ Fleming, C. J. (2016). Microbiota activated CD103+ DCS stemming from oral microbiota adaptation specifically drive γδT17 proliferation and activation.
- Rickard A H (2008). "Cell-cell Communication in Oral Microbial Communities". Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
External links
| Wikispecies has information related to Microbiota |