Optic disc
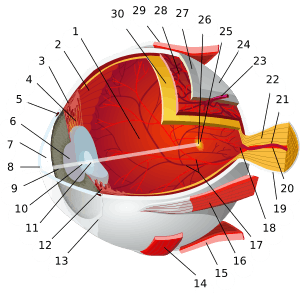
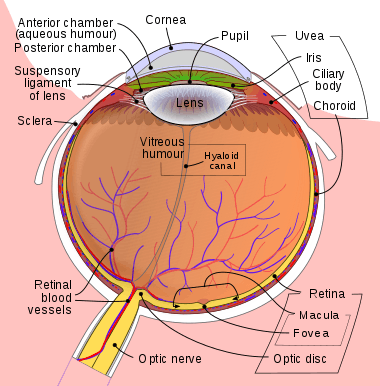
The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
| Optic disc | |
|---|---|
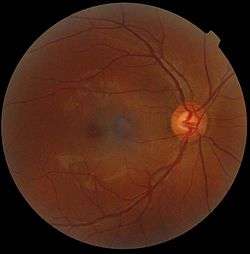 Ophthalmoscopy photograph showing the optic disc as a bright area on the right where blood vessels converge. | |
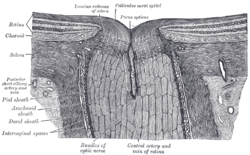 The terminal portion of the optic nerve and its entrance into the eyeball, in horizontal section. | |
| Details | |
| Identifiers | |
| Latin | Discus nervi optici |
| MeSH | D009898 |
| TA | A15.2.04.019 |
| FMA | 58634 |
| Anatomical terminology | |
The ganglion cell axons form the optic nerve after they leave the eye. The optic disc represents the beginning of the optic nerve and is the point where the axons of retinal ganglion cells come together. The optic disc is also the entry point for the major blood vessels that supply the retina.[1] The optic disc in a normal human eye carries 1–1.2 million afferent nerve fibers from the eye towards the brain.
Structure
The optic disc is placed 3 to 4 mm to the nasal side of the fovea. It is a vertical oval, with average dimensions of 1.76mm horizontally by 1.92mm vertically.[2] There is a central depression, of variable size, called the optic cup. This depression can be a variety of shapes from a shallow indentation to a bean pot—this shape can be significant for diagnosis of some retinal disease.
Function
The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
Clinical significance
The eye is unique because of the transparency of its optical media. Almost all eye structures can be examined with appropriate optical equipment and lenses. Using a modern direct ophthalmoscope gives a view of the optic disc using the principle of reversibility of light. A slit lamp biomicroscopic examination along with an appropriate aspheric focusing lens (+66D, +78D or +90D) is required for a detailed stereoscopic view of the optic disc and structures inside the eye.
A biomicroscopic exam can give an indication of the health of the optic nerve. In particular, the eye care physician notes the colour, cupping size (as a cup-to-disc ratio), sharpness of edge, swelling, hemorrhages, notching in the optic disc and any other unusual anomalies. It is useful for finding evidence corroborating the diagnosis of glaucoma and other optic neuropathies, optic neuritis, anterior ischemic optic neuropathy or papilledema (i.e. optic disc swelling produced by raised intracranial pressure), and optic disc drusen.
Women in advanced stage of pregnancy with pre-eclampsia should be screened by an ophthalmoscopic examination of the optic disc for early evidence of rise in intracranial pressure.
Pale disc
A normal optic disc is orange to pink in colour. A pale disc is an optic disc which varies in colour from a pale pink or orange colour to white. A pale disc is an indication of a disease condition.
Imaging
Traditional colour-film camera images are the reference standard in imaging, requiring an expert ophthalmic photographer, ophthalmic technician, optometrist or an ophthalmologist for taking standardised pictures of the optic disc. Stereoscopic images offer an excellent investigative tool for serial follow-up of suspected changes in the hands of an expert optometrist or ophthalmologist.
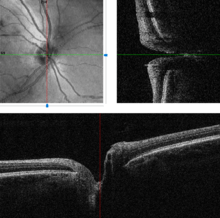
Automated techniques have also been developed to allow for more efficient and less expensive imaging. Heidelberg retinal tomography (HRT), scanning laser polarimetry and optical coherence tomography are computerised techniques for imaging various structures of the eyes, including the optic disc. They quantify the nerve fiber layer of disc and surrounding retina and statistically correlate the findings with a database of previously screened population of normals. They are useful for baseline and serial follow-up to monitor minute changes in optic disc morphology. Imaging will not provide conclusive evidence for clinical diagnosis however, and the evidence needs to be supplanted by serial physiological testing for functional changes. Such tests may include visual field charting and final clinical interpretation of the complete eye examination by an eye care physician. Ophthalmologists and optometrists are able to provide this service.
Blood flow in the retina and choroid in the optic disc region can be revealed non invasively by near-infrared laser Doppler imaging [3]. Laser Doppler imaging can enable mapping of the local arterial resistivity index, and the possibility to perform unambiguous identification of retinal arteries and veins on the basis of their systole-diastole variations, and reveal ocular hemodynamics in human eyes. [4]
A systematic review of 106 studies and 16,260 eyes compared the performance of the imaging techniques, and found that all three imaging tests performed very similarly when detecting for glaucoma.[5] The review found that in 1000 patients subjected to imaging tests, with 200 having manifest glaucoma, the best imaging tests would miss 60 cases out of the 200 patients with glaucoma, and incorrectly refer 50 out of 800 patients without glaucoma.[5]
 Blood flow in the optic disc revealed by laser Doppler imaging [3].
Blood flow in the optic disc revealed by laser Doppler imaging [3]. Three dimensional image of a healthy optic disc in a 24-year-old female.
Three dimensional image of a healthy optic disc in a 24-year-old female.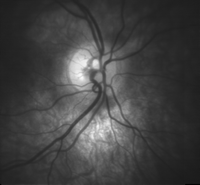 Optic disc showing microvasculature.
Optic disc showing microvasculature. Tilted optic disc in left eye of a 20-year-old male.
Tilted optic disc in left eye of a 20-year-old male. Optic disc edema and haemorrhage
Optic disc edema and haemorrhage
See also
References
- "blind spot". Encyclopædia Britannica. 2011. Retrieved June 21, 2017.
- Tasman, William; Jaeger, Edward A (2006). "Chapter 4: Anatomy of the Visual Sensory System". Duane's Ophthalmology. Philadelphia: Lippincott Williams & Wilkins. ISBN 9780781768559. OCLC 318288606.
- Puyo, L., M. Paques, M. Fink, J-A. Sahel, and M. Atlan. "In vivo laser Doppler holography of the human retina." Biomedical optics express 9, no. 9 (2018): 4113-4129.
- Puyo, Léo, Michel Paques, Mathias Fink, José-Alain Sahel, and Michael Atlan. "Waveform analysis of human retinal and choroidal blood flow with laser Doppler holography." Biomedical Optics Express 10, no. 10 (2019): 4942-4963.
- Michelessi M, Lucenteforte E, Oddone F, Brazzelli M, Parravano M, Franchi S, Ng SM, Virgili G (2015). "Optic nerve head and fibre layer imaging for diagnosing glaucoma". Cochrane Database Syst Rev (11): CD008803. doi:10.1002/14651858.CD008803.pub2. PMC 4732281. PMID 26618332.