Opicapone
Opicapone is a drug which is a catechol-O-methyltransferase (COMT) inhibitor. It is administered together with levodopa in patients with Parkinson's disease. In June 2016 it was authorised for sale – under the trade name Ongentys – in the European Union.[1] In February 2017, its developer Bial sold exclusive marketing rights for the United States and Canada to Neurocrine Biosciences for an initial payment of $30 million.[2]
 | |
| Clinical data | |
|---|---|
| Trade names | Ongentys |
| Other names | BIA 9-1067 |
| AHFS/Drugs.com | UK Drug Information |
| License data | |
| Routes of administration | By mouth (capsules) |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ~20% |
| Protein binding | 99.9% |
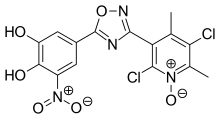
| Metabolism | Mainly sulfation, also reduction, glucuronidation, methylation |
| Elimination half-life | 0.7 to 3.2 hours |
| Duration of action | >24 hours |
| Excretion | Faeces (67%), urine (13%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C15H10Cl2N4O6 |
| Molar mass | 413.17 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Medical uses
The COMT inhibitor opicapone is used as an additive to a combination of levodopa and a DOPA decarboxylase inhibitor to treat patients with Parkinson's disease experiencing end-of-dose motor fluctuations, if they cannot be stabilised with this drug combination.[3]
Contraindications
This drug is contraindicated in people with cancers that secrete catecholamines (for example epinephrine), such as phaeochromocytoma or paraganglioma, because as a COMT inhibitor it blocks catecholamine degradation. Other contraindications are a history of neuroleptic malignant syndrome (NMS) or non-traumatic rhabdomyolysis, and combination with monoamine oxidase inhibitors that are not used as antiparkinsonians, because of possible drug interactions.[3]
NMS and associated rhabdomyolysis have been rarely observed under the older COMT inhibitors tolcapone and entacapone. This typically occurs shortly after the beginning of a COMT inhibitor add-on therapy when the levodopa dose has been reduced, or after discontinuation of a COMT inhibitor.[4]
Side effects
People taking opicapone very commonly (18%) experience dyskinesia. Other common side effects (in 1 to 10% of patients) include dizziness, strange dreams, hallucinations, constipation, dry mouth, orthostatic hypotension (low blood pressure), and muscle spasms.[3] Apart from spasms, these side effects are also known from tolcapone and entacapone.[4]
As with entacapone, no relevant liver toxicity has been found in studies. This is in contrast to the first COMT inhibitor tolcapone, which could cause – in some cases lethal – liver insufficiency.[4][5]
Overdose
No specific antidote is known.[3]
Interactions
Monoamine oxidase inhibitors (MAO inhibitors) are another class of drugs blocking catecholamine degradation. Therefore, their combination with opicapone can result in increased catecholamine concentrations in the body and corresponding adverse effects. Combining the antiparkinson MAO inhibitors selegiline or rasagiline with opicapone is considered safe. Potentially, there are also interactions with drugs being metabolised by COMT (for example isoprenaline, epinephrine, dopamine, or dobutamine), tricyclic antidepressants and antidepressants of the norepinephrine reuptake inhibitor type. Possible pharmacokinetic interactions are with substrates of the liver enzyme CYP2C8, such as repaglinide, and the transporter protein SLCO1B1, such as simvastatin.[3]
Pharmacology
Mechanism of action
Opicapone blocks the enzyme catechol-O-methyltransferase (COMT) effectively (>90% at therapeutic doses), selectively and reversibly, and only outside the central nervous system. It dissociates slowly from COMT, resulting in a duration of action longer than 24 hours despite its short blood plasma half-life.[3][5] As COMT and DOPA decarboxylase are the main enzymes for degrading levodopa, blocking the two effectively increases its concentrations in the bloodstream. More levodopa reaches the brain, where it is activated to dopamine.[6]
Pharmacokinetics
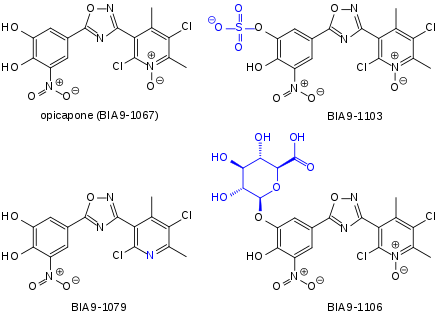
The substance is quickly absorbed from the gut, but only to about 20% of the applied dose. Highest blood plasma concentrations are reached after 1 to 2.5 hours. When in the bloodstream, it is almost completely (99.9%) bound to plasma proteins, but apparently to different binding sites than warfarin, digoxin and other drugs with high plasma protein affinity. It is mainly metabolised to the sulfate, which accounts for 67% of the circulating drug after a single dose, and a methylated derivative, which accounts for 21%. Minor metabolites are a reduced derivative (<10%) and a glucuronide. All of these metabolites are inactive except the reduced derivative. Opicapone is eliminated with a terminal half-life of 0.7 to 3.2 hours. It is mainly excreted via the faeces (67%), and in form of the glucuronide also via the kidney (13%). The sulfate has a much longer half-life of 94 to 122 hours.[3][5][7]
Opicapone sulfate is transported by SLCO1B1; the possibility that it blocks this transporter has not been excluded. Opicapone itself and the sulfate are also transported by a number of other proteins, but given the low concentrations of the free substances in the blood plasma, this is very unlikely to give rise to drug interactions. Opicapone is a weak inhibitor of the liver enzymes CYP1A2, CYP2B6, CYP2C8, and CYP2C9. The only CYP interaction found in studies that is somewhat likely to be relevant is that with repaglinide, which is metabolised by CYP2C8. The metabolism of warfarin, a CYP2C9 substrate, is not measurably affected.[3]
References
- Neurocrine Nabs BIAL's PD Therapy Opicapone for North America. Genetic Engineering & Biotechnology News. Accessed April 2017.
- [s.n.] (9 February 2017). Brief: Neurocrine and Bial reports exclusive North American licensing agreement for opicapone. Reuters. Accessed April 2017.
- "Ongentys: EPAR – Product Information" (PDF). European Medicines Agency. 2 February 2017.
- Haberfeld, H, ed. (2017). Austria-Codex (in German). Vienna: Österreichischer Apothekerverlag. Comtan, Tasmar.
- Annus, Á; Vécsei, L (2017). "Spotlight on opicapone as an adjunct to levodopa in Parkinson's disease: design, development and potential place in therapy". Drug Des Devel Ther. 11: 143–151. doi:10.2147/DDDT.S104227. PMC 5234693. PMID 28123288.
- Mutschler, Ernst; Schäfer-Korting, Monika (2001). Arzneimittelwirkungen (in German) (8 ed.). Stuttgart: Wissenschaftliche Verlagsgesellschaft. p. 315. ISBN 3-8047-1763-2.
- Rocha, JF (2013). "Opicapone: a short lived and very long acting novel catechol-O-methyltransferase inhibitor following multiple dose administration in healthy subjects". Br J Clin Pharmacol. 76 (5): 763–775. doi:10.1111/bcp.12081. PMC 3853535. PMID 23336248.