Odontogenic keratocyst
An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life.[1] Odontogenic keratocysts make up around 19% of jaw cysts.[2]
| Odontogenic keratocyst | |
|---|---|
| Other names | Keratocystic odontogenic tumour (KCOT) |
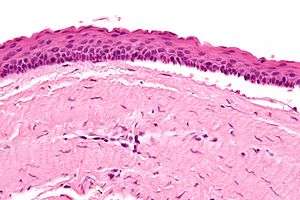 | |
| Micrograph of an odontogenic keratocyst. H&E stain. | |
In the WHO/IARC classification of head and neck pathology, this clinical entity had been known for years as the odontogenic keratocyst; it was reclassified as keratocystic odontogenic tumour (KCOT) from 2005 to 2017.[3][4] In 2017 it reverted to the earlier name, as the new WHO/IARC classification reclassified OKC back into the cystic category.[5] The WHO/IARC classification no longer considers it a neoplasm, because the evidence supporting that hypothesis (for example, clonality) is considered insufficient. However, this is an area of hot debate within the head and neck pathology community, and some pathologists still regard OKC as a neoplasm despite the reclassification.
Signs and symptoms
Peak incidence during second and third decades of life. At least 50% of odontogenic keratocysts are found in posterior part and lower ramus of the mandible.[6] Swelling is the most common presenting complaint; however, OKCs may be asymptomatic and found incidentally on dental radiographs.[7] Rarely symptoms can arise due to infection or expansion of the bone.[6][2]
Pathogenesis
Odontogenic keratocysts originate from the odontogenic epithelium (dental lamina) in the alveolus left from tooth development stages. They are mainly thought to arise from rests of Serres.[6]
Genetics
Sporadic (non-syndromic) and syndromic OKCs are associated with mutations in the gene PTCH found on chromosome 9q, which is part of the Hedgehog signaling pathway.[4][8] PTCH is a tumour suppressor gene. Loss of PTCH activity leads to a brake in the cell cycle. A third of OKCs show mutations in PTCH, resulting in the cyst epithelium undergoing highly proliferative activity. This leads to growth of the cyst wall and when removed favours recurrence if following incomplete removal of the epithelium.[6]
Nevoid basal-cell carcinoma syndrome
Multiple odontogenic keratocysts are a feature, and major diagnostic criteria, of nevoid basal cell carcinoma syndrome (NBCCS, also known as Gorlin-Goltz Syndrome). Almost all individuals with NBCCS have odontogenic keratocysts which require numerous treatments. Consideration of the syndrome needs to be taken into account if found in children or if multiple OKCs are present; diagnosis of multiple OKCs in a child necessitates referral for genetic evaluation. Histologically, the cysts are indistinguishable to non-syndromic cysts and over 80% will have PTCH mutations.[6]
Diagnosis

Diagnosis is usually radiological. However, definitive diagnosis is through biopsy. Aspirational biopsy of odontogenic keratocysts contains a greasy fluid which is pale in colour and contains keratotic squames.[9][2] Protein content of cyst fluid below 4g% is diagnostic of odontogenic keratocysts.[2] Smaller and unilocular lesions resembling other types of cysts may require a biopsy to confirm the diagnosis.[6] On a CT scan, the radiodensity of a keratocystic odontogenic tumour is about 30 Hounsfield units, which is about the same as ameloblastomas. However, ameloblastomas show more bone expansion and seldom show high density areas.[10]
Radiographs of odontogenic keratocysts show well-defined radiolucent areas with rounded or scalloped margins which are well demarcated.[9] These areas can be multilocular or unilocular. The growth pattern of the lesion is very characteristic from which a diagnosis can be made as there is growth and spread both forward and backward along the medullary cavity with little expansion. No resorption of teeth or inferior dental canal and minimal displacement of teeth is seen. Due to lack of expansion of the odontogenic keratocyst, the lesion can be very large when radiographically discovered.[6]
Differential diagnosis
Radiologically
- Odontogenic myxoma
- Ameloblastoma
- Central giant-cell granuloma
- Adenomatoid odontogenic tumor
- Dentigerous cyst (follicular cyst)
Histologically
- Orthokeratocyst
- Radicular cyst (particularly if the OKC is very inflamed)
- Ameloblastoma
Histology
Odontogenic keratocysts have a diagnostic histological appearance. Under the microscope, OKCs vaguely resemble keratinized squamous epithelium;[11] however, they lack rete ridges and often have an artifactual separation from their basement membrane.[2]
The fibrous wall of the cyst is usually thin and uninflamed. The epithelial lining is thin with even thickness and parakeratinised with columnar cells in the basal layer which have focal reverse polarisation (nuclei are on the opposite pole of the cell).[9] The basal cells are an indication of the odontogenic origin as they resemble pre-ameloblasts. The epithelium can separate from the wall, resulting in islands of epithelium. These can go on to form 'satellite' or 'daughter' cysts, leading to an overall multilocular cyst.[6] Presence of daughter cysts is particularly seen in those with NBCCS.[9] Inflamed cysts show hyperplastic epithelium which is no longer characteristic of OKCs and can have resemblance to radicular cysts instead. Due to areas of focal inflammation, a larger biopsy is required for correct diagnosis of odontogenic keratocysts.[6]
 Intermediate magnification of an odontogenic keratocyst showing a folded cyst.
Intermediate magnification of an odontogenic keratocyst showing a folded cyst. Intermediate magnification of an odontogenic keratocyst
Intermediate magnification of an odontogenic keratocyst High magnification of an odontogenic keratocyst.
High magnification of an odontogenic keratocyst.
Treatment

As the condition is quite rare, opinions among experts about how to treat OKCs differ. A 2015 Cochrane review found that there is currently no high quality evidence to suggest the effectiveness of specific treatments for the treatment of odontogenic keratocysts.[12] Treatment depends on extent of multilocularity and cyst. Small multilocular and unilocular cysts can be treated more conservatively through enucleation and curretage.
- Wide (local) surgical excision to remove the whole cyst lining.
- Curettage involving simple excision and scraping-out of cavity.
- Carnoy's solution fixative (ethanol, chloroform and acetic acid) which is usually used in conjunction with excision and curretage. Cavity wall can be treated with the fixative either before enucleation to kill the lining of the wall or added after curretage to bony walls, killing any residual epithelial cells to a depth of 1-2mm. Used with care near mandibular canal and the neurovascular bundle within.
- Marsupialization which involves the surgical opening of the cyst cavity and a creation of a marsupial-like pouch. This allows the cavity to be in contact with the outside of the cyst for an extended period of time. Marsupialisation results in slow shrinkage of the cyst allowing later enucleation. However, resolution can take up to 20 months and patients are required to clean the open cavity and irrigate it.
- Peripheral ostectomy after curettage and/or enucleation. Extensive cysts may require a bone graft after bone resection and reconstruction of the area.
- Simple excision
- Enucleation and cryotherapy.[13] Decompression followed by enucleation has been shown to be most successful with lowest recurrence rates.[14]
Follow-up
Annual radiographic review has been recommended.[9] Long-term clinical follow-up is also recommended due to recurrences occurring many years after treatment.[2]
Recurrence and neoplastic nature
Malignant transformation to squamous cell carcinoma may occur, but is unusual.[15]
Recurrence is likely when treated by simple enucleation. Contributing causes include thin and fragile epithelium leading to incomplete removal, cyst extensions extending into cancellous bone, satellite cysts found in the wall, experience of the surgeon, formation of further new cysts from other remnants of the dental epithelium. With current treatment techniques the recurrence rate is around 2-3%. Recurrence is usually seen within 5 years of treatment. Early findings of recurrence can be easily treated with minor surgery and curretage.[6]
The neoplastic nature of odontogenic keratocysts has been debated. Due to high recurrence rate, late detection when the cyst has grown very large and causation by tumour suppressor gene inactivation, some have classified OKCs as benign neoplasms. The best evidence to suggest that this type of cyst is not a neoplasm is that it responds very well to marsupialisation.[6]
See also
References
- MacDonald-Jankowski, D S (2011). "Keratocystic odontogenic tumour: systematic review". Dentomaxillofacial Radiology. 40 (1): 1–23. doi:10.1259/dmfr/29949053. ISSN 0250-832X. PMC 3611466.
- Crispian., Scully, (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. ISBN 9780443068188. OCLC 123962943.CS1 maint: extra punctuation (link)
- Barnes, L; Eveson, JW; Reichart, P; Sidransky, D, eds. (2005), World Health Organization Classification of Tumours: Pathology and Genetics of Head and Neck Tumours (PDF), World Health Organization Classification of Tumours (2005 ed.), Lyon, France: IARC Press, ISBN 978-92-832-2417-4, Archived from the original on 2015-09-24.CS1 maint: BOT: original-url status unknown (link)
- Madras, J; Lapointe, H (2008). "Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour". J Can Dent Assoc. 74 (2): 165–165h. PMID 18353202.
- El-Naggar, Adel K; Chan, John KC; Grandis, Jennifer R; Takata, Takashi; Slootweg, Pieter J, eds. (2017), WHO Classification of Head and Neck Tumours, WHO/IARC Classification of Tumours, 9 (4th ed.), Lyon, France: IARC Press, ISBN 978-92-832-2438-9.
- W.,, Odell, E. Cawson's essentials of oral pathology and oral medicine. Preceded by (work): Cawson, R. A. (Ninth ed.). [Edinburgh]. ISBN 9780702049828. OCLC 960030340.CS1 maint: extra punctuation (link)
- Habibi A, Saghravanian N, Habibi M, Mellati E, Habibi M (September 2007). "Keratocystic odontogenic tumor: a 10-year retrospective study of 83 cases in an Iranian population". J Oral Sci. 49 (3): 229–35. doi:10.2334/josnusd.49.229. PMID 17928730. Archived from the original on 2012-07-16.
- PATCHED, DROSOPHILA, HOMOLOG OF, 1; PTCH1. OMIM. URL: https://www.ncbi.nlm.nih.gov/omim/?term=601309. Accessed on: December 25, 2008.
- Paul,, Coulthard,. Master dentistry. Volume 1, Oral and maxillofacial surgery, radiology, pathology and oral medicine. Horner, Keith, 1958-, Sloan, Phil (Dentist),, Theaker, Elizabeth D., (Third ed.). Edinburgh. ISBN 9780702046001. OCLC 826658944.CS1 maint: extra punctuation (link)
- Ariji, Y; Morita, M; Katsumata, A; Sugita, Y; Naitoh, M; Goto, M; Izumi, M; Kise, Y; Shimozato, K; Kurita, K; Maeda, H; Ariji, E (2011). "Imaging features contributing to the diagnosis of ameloblastomas and keratocystic odontogenic tumours: logistic regression analysis". Dentomaxillofacial Radiology. 40 (3): 133–140. doi:10.1259/dmfr/24726112. ISSN 0250-832X. PMC 3611454.
- Thompson LDR. Head and neck pathology - (Foundations in diagnostic pathology). Goldblum JR, Ed.. Churchill Livingstone. 2006. ISBN 0-443-06960-3.
- Sharif, Fyeza N. J.; Oliver, Richard; Sweet, Christopher; Sharif, Mohammad O. (2015-11-05). "Interventions for the treatment of keratocystic odontogenic tumours". The Cochrane Database of Systematic Reviews (11): CD008464. doi:10.1002/14651858.CD008464.pub3. ISSN 1469-493X. PMID 26545201.
- Schmidt BL, Pogrel MA (2001). "The use of enucleation and liquid nitrogen cryotherapy in the management of odontogenic keratocysts". J Oral Maxillofac Surg. 59 (7): 720–727. doi:10.1053/joms.2001.24278. PMID 11429726.
- de Castro, Mayara Santos; Caixeta, Clenivaldo Alves; de Carli, Marina Lara; Ribeiro Júnior, Noé Vital; Miyazawa, Marta; Pereira, Alessandro Antônio Costa; Sperandio, Felipe Fornias; Hanemann, João Adolfo Costa (June 2018). "Conservative surgical treatments for nonsyndromic odontogenic keratocysts: a systematic review and meta-analysis". Clinical Oral Investigations. 22 (5): 2089–2101. doi:10.1007/s00784-017-2315-8. ISSN 1436-3771. PMID 29264656.
- Piloni MJ, Keszler A, Itoiz ME (2005). "Agnor as a marker of malignant transformation in odontogenic keratocysts". Acta Odontol Latinoam. 18 (1): 37–42. PMID 16302459.