Obliterative bronchiolitis
Obliterative bronchiolitis (OB), also known as constrictive bronchiolitis and popcorn lung, is a disease that results in obstruction of the smallest airways of the lungs (bronchioles) due to inflammation.[1][6] Symptoms include a dry cough, shortness of breath, wheezing and feeling tired.[1] These symptoms generally get worse over weeks to months.[4] It is not related to cryptogenic organizing pneumonia, previously known as bronchiolitis obliterans organizing pneumonia.[4]
| Obliterative bronchiolitis (OB)[1] | |
|---|---|
| Other names | Bronchiolitis obliterans constrictive bronchiolitis (CB),[2] bronchiolitis obliterans syndrome (BOS), popcorn lung |
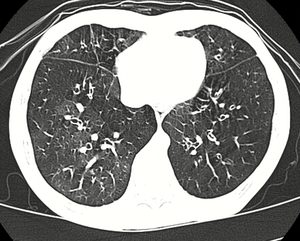 | |
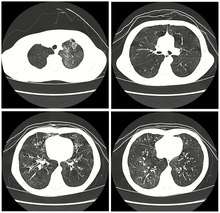
| High resolution CT scan showing bronchiolitis obliterans with mosaic attentuation, bronchiectasis, air trapping and bronchial thickening[3] | |
| Specialty | Pulmonology |
| Symptoms | Dry cough, shortness of breath, wheezing, feeling tired[1] |
| Usual onset | Worsens over weeks to months[4] |
| Causes | Toxic fumes, respiratory infections, connective tissue disorder, following a bone marrow or heart-lung transplant[1] |
| Diagnostic method | CT scan, pulmonary function tests, lung biopsy[1] |
| Differential diagnosis | Asthma[5] |
| Treatment | Corticosteroids, immunosuppressive medication, lung transplant[1][4] |
| Prognosis | Often poor[4] |
| Frequency | Rare[4] |
Causes include breathing in toxic fumes, respiratory infections, connective tissue disorder or complications following a bone marrow or heart-lung transplant.[1] Symptoms may not occur until two to eight weeks following toxic exposure or infection.[1] The underlying mechanism involves inflammation that results in scar tissue formation.[1] Diagnosis is by CT scan, pulmonary function tests or lung biopsy.[1] A chest X-ray is often normal.[4]
While the disease is not reversible, treatments can slow further worsening.[1] This may include the use of corticosteroids or immunosuppressive medication.[1] A lung transplant may be offered.[4] Outcomes are often poor, with most people dying in months to years.[4]
Obliterative bronchiolitis is rare in the general population.[4] It, however, affects about 75% of people by ten years following a lung transplant and up to 10% of people who have received a bone marrow transplant from someone else.[4] The condition was first clearly described in 1981.[4] Prior descriptions occurred as early as 1956, with the term "bronchiolitis obliterans" used first by Reynaud in 1835.[7][8]
Signs and symptoms
Obliterative bronchiolitis results in worsening shortness of breath, wheezing, and a dry cough. The symptoms can start gradually, or severe symptoms can occur suddenly.[9][10] These symptoms represent an obstructive pattern that is non-reversible with bronchodilator therapy, and need to be related to various lung insults.[11] These insults include inhalation damage, post transplant auto-immune injury, post-infectious disease, drug reactions, and several auto-immune diseases.[6]
Cause
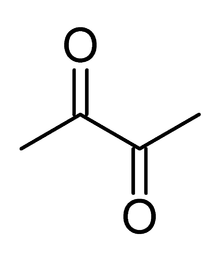
Obliterative bronchiolitis has many possible causes, including collagen vascular disease, transplant rejection in organ transplant patients, viral infection (adenovirus, respiratory syncytial virus, influenza, HIV, cytomegalovirus), Stevens-Johnson syndrome, Pneumocystis pneumonia, drug reaction, aspiration and complications of prematurity (bronchopulmonary dysplasia), and exposure to toxic fumes, including diacetyl, sulfur dioxide, nitrogen dioxide, ammonia, chlorine, thionyl chloride, methyl isocyanate, hydrogen fluoride, hydrogen bromide, hydrogen chloride, hydrogen sulfide, phosgene, polyamide-amine dyes, mustard gas and ozone.[4][6][12] It can also be present in patients with IBD, systemic lupus erythematosus, juvenile idiopathic arthritis, rheumatoid arthritis, GERD, IgA nephropathy, and ataxia telangiectasia.[13][14][6] Activated charcoal, have been known to cause it when aspirated.[15] The ingestion of large doses of papaverine in the vegetable Sauropus androgynus has caused it.[16] Additionally, the disorder may be idiopathic (without known cause).[17][18][19]
Lung transplant
Obliterative bronchiolitis is a common complication in lung transplant, because transplanted lungs are at greater risk of alloimmunization as compared to healthy lungs. The disease is often termed bronchiolitis obliterans syndrome (BOS) in the setting of post lung transplantation and hematopoietic stem cell transplant (HSCT).[6] Patients who develop BOS post lung transplant vary in time frame and disease severity.[6] Patients often initially have normal lung function on pulmonary function testing and have normal chest radiographs.[6] As the disease progresses they begin to have symptoms of shortness of breath, cough, and wheezing as their lung function declines. The Journal of Heart and Lung Transplantation published updated guidelines in 2001 for grading the severity of BOS.[20] The original guidelines and classification system were published in 1993 by the International Society for Heart and Lung Transplantation.[20] Their scoring system is based on the changes in FEV1 in patients from their baseline.[20] When patients are first diagnosed with BOS they have their baseline lung function established by doing pulmonary function testing at the time of diagnosis.[20] The BOS scoring system is as follows:
BOS 0: FEV1 > 90% of baseline and FEF25-75 > 75% of baseline
BOS 0-p: FEV1 81-89% of baseline and/or FEF25-75 <= 75% of baseline
BOS 1: FEV1 66-80% of baseline
BOS 2: FEV1 51-65% of baseline
BOS 3: FEV1 50% or less of baseline
The scoring system shows an increased severity of the disease as the BOS number increases.[20]
Hematopoietic stem cell transplant
Obliterative bronchiolitis affects up to 5.5% of people who have received HSCT.[21] One of the biggest risk factors after HSCT is the development of GVHD with a 14% risk.[22] Other risk factors post transplant including tobacco use, age of donor, age of recipient, lower baseline FEV1/FVC ratio, non-caucasian race, peripheral and lower circulating IgG levels.[6] Studies have, however, shown mixed results regarding these other risk factors. There has been an association shown between the increased use of peripheral stem cells and the risk of developing obliterative bronchiolitis.[6] Also, research has shown an increased risk for developing the disease within the first year of transplant if the person is infected with respiratory syncytial virus or parainfluenza virus within the first 100 days post transplant.[6]
Inhalants
There are many industrial inhalants that are known to cause various types of bronchiolitis, including obliterative bronchiolitis.[23]
Industrial workers who have presented with bronchiolitis:
- nylon-flock workers[19]
- workers who spray prints onto textiles with polyamide-amine dyes[19]
- battery workers who are exposed to thionyl chloride fumes
- workers at plants that use or manufacture flavorings such as diacetyl[9][19][24]
Diacetyl is a chemical used to produce the artificial butter flavoring[25] in many foods such as candy and microwave popcorn and occurring naturally in wines. This first came to public attention when eight former employees of the Gilster-Mary Lee popcorn plant in Jasper, Missouri developed obliterative bronchiolitis. Due to this event, obliterative bronchiolitis began to be referred to in the popular media as "popcorn lung" or "popcorn workers lung".[26][27][28][29] It is also referred to as "flavorings-related lung disease".[30]
Post-infectious
Typically found in young children and is the most common cause at this age.[31] Generally occurs after a viral infection of adenovirus (types 3, 7, and 21), measles (rubeola), mycoplasma, CMV, influenza, and parainfluenza.[4][6] Swyer-James syndrome is a rare complication of obliterative bronchiolitis caused by measles or adenovirus.[32] Post-infectious obliterative bronchiolitis is most common in the southern hemisphere particularly in countries such as Brazil, Argentina, Australia, Chile and New Zealand.[33] There was a large prevalence of the disease in these areas during the 1990s and early 2000s. In one hospital in Buenos Ares, the Ricardo Gutiérrez Children's hospital, the disease accounted for 14% of their inpatient respiratory population from 1993 to 2002.[33] As such, much of the information about post-infectious obliterative bronchiolitis has come from research out of South America. The most significant risk factors for the disease are infection with adenovirus and the need for ventilator support.[33] In contrast with another cause of obliterative bronchiolitis in children, Steven's Johnson's syndrome, post-infectious obliterative bronchiolitis tends to be a chronic but non-progressive disease.[31] The disease can have varying impact on children and their quality of life, which has been studied by lung function tests, as well as their exercise tolerance.[34] Children with lower lung function based on their pulmonary function testing, have lower exercise tolerance, which compounds the impact of the disease on cardiovascular function as they are not able to maintain age appropriate aerobic fitness.[34] This ultimately affects their activities of daily living (ADLs) and their quality of life going forward.[34]
Burn pits
A form of constrictive bronchiolitis is starting to present in Iraq and Afghanistan veterans. It has been attributed to veterans being exposed to trash burn pits. Veterans present with shortness of breath and other asthma-like symptoms. The only way to diagnose this condition is by doing a lung biopsy as chest X-rays and CT scans come back as normal. The government still denies that there is any correlation between burn pits and health problems but the government has started an "Airborne Hazards and Open Burn Pit Registry" to begin tracking the health of veterans who were exposed to burn pits to see if there is a connection.[35][36]
Mechanism
The underlying mechanism involves injury and inflammation of epithelial and sub-epithelial cells. These cells then lose the ability to repair the tissue, in particular they lose the ability to regenerate the epithelial or outermost layer, leading to the excess growth of cells that cause scarring.[11][6][1] There are multiple pathways of the disease including fibrotic, lymphocytic, and antibody-mediated that have been described. However, while each pathway has a more unique starting point and cause, the end result is still injury and inflammation leading to scarring of the lung tissue.[11] The scarred tissue then makes the expiration phase of respiration more difficult, leading to air not being expelled from the lungs. This is termed "air-trapping", which can be seen on medical imaging.[6] Since the scarring is non-reversible, the disease generally does not improve over time, and depending on the inciting can progress to death.[11]
Diagnosis

-bronchiolitis_obliterans_(4734022020).jpg)
Obliterative bronchiolitis is often diagnosed based on the symptoms of obstructive lung disease following lung injury. The definitive diagnosis is through biopsy, but due to the variable distribution of lesions, leading to falsely negative tests, and invasive nature of this procedure it is often not performed.[6][11] Several tests are often needed to diagnose obliterative bronchiolitis, including spirometry, diffusing capacity of the lung tests (DLCO), lung volume tests, chest X-rays, high-resolution CT (HRCT), and lung biopsy.[11][4]
Pulmonary function testing
Spirometry tests usually show a obstructive pattern and is the most common presentation.[6] A slightly reduced to normal forced vital capacity (FVC), and a reduced FEV1 to FVC ratio and forced expiratory volume (FVC) with little to no correction with the use of bronchodialators are common findings.[11][4] Lung volume tests may show hyperinflation (excessive air in lungs caused by air trapping). Diffusing capacity of the lung (DLCO) tests are usually normal; people with early-stage OB are more likely to have normal DLCO.
FEV1 (forced expiratory volume in 1 second) should be above 80% of predicted values to be considered normal. Obliterative bronchiolitis reduces this to between 16% and 21%.
Medical imaging
Early in the disease chest radiography is typically normal but may show hyperinflation.[6] As the disease progresses a reticular pattern with thickening of airway walls may be present.[4][6] HRCT can also show air trapping when the person being scanned breathes out completely; it can also show thickening in the airway and haziness in the lungs.[11] A common finding on HRCT is patchy areas of decreased lung density, signifying reduced vascular caliber and air trapping.[6] This pattern is often described as a "mosaic pattern", and may indicate obliterative bronchiolitis.[6]
Lung biopsy
Transthoracic lung biopsies are preferable for diagnosis of constrictive BO compared to transbronchial biopsies; regardless of the type of biopsy, a diagnosis may only be achieved by examination of multiple samples.[30] Transthoracic biopsies are preferred over transbronchial due to the heterogeneity and distribution of the lesions.[11] OB can be further classified into two categories: constrictive or proliferative.[11] The constrictive pattern is demonstrated by peribronchiolar cellular infiltrates which eventually causes small airway damage and leads to subepithelial fibrosis.[11] The bronchial muscle can eventually become fibrosed which can be identified with trichrome staining.[11] In regards to proliferative disease, intraluminal buds called "Masson bodies" fill the lumen, which results in bronchiolar plugging.[11] Often people with proliferative disease will show butterfly wing-like appearance under microscopy.[11] One key determinate that can be seen on biopsy to differentiate constrictive from proliferative disease is the extent of lesions. Both lesions are localized from the small bronchi to the membranous bronchi, but in constrictive disease the lesions are intermittent while proliferative disease has a continuous distribution.[11]
Differential diagnosis
Other conditions that can present similarly include chronic obstructive pulmonary disease, asthma, bronchiectasis, hypersensitivity pneumonitis, and pneumonia.[30][37]
Prevention
Inhalants
Disease caused by exposure to industrial inhalants and burn pits can be prevented with the use of engineering controls (e.g., exhaust hoods or closed systems), personal protective equipment, monitoring of potentially affected personnel, worker education and training.
Transplant
The primary prevention of obliterative bronchiolitis in people who have received either lung transplant or HSCT therapy is immunosuppression.[6] In regards to post lung transplantion, the combination of calcineurin inhibitor combined with a purine synethesis inhibitor and a glucocorticoid is the general regimen used.[6] People also have a baseline post-transplant lung function testing done in order to determine over time if their lung function is declining. People who are post HSCT their immunosuppressive regimen typically includes methotrexate in combination with a calcineurin inhibitor to prevent GVHD, a risk factor for developing obliterative bronchiolitis.[6]
Treatment
While the disease is not reversible, treatments can slow further worsening.[1] This may include the use of corticosteroids or immunosuppressive medication which may have an effect on the ability to receive a lung transplant if offered.[1][4] If patients have difficulty breathing (hypoxemia) oxygen can be supplemented. Routine vaccinations are recommended for patients with chronic lung disease to prevent complications from secondary infections due to pneumonia and influenza.[11]
Transplant recipients are at risk for re-developing the disease, as obliterative bronchiolitis is a common complication of chronic rejection. Evaluation of interventions to prevent obliterative bronchiolitis relies on early detection of abnormal spirometry results or unusual decreases in repeated measurements.
Terminology
"Bronchiolitis obliterans" was originally a term used by pathologist to describe two patterns of airway disease.[6] One was bronchiolitis obliterans organizing pneumonia (BOOP), also known as cryptogenic pneumonia, and the other is now known as obliterative bronchiolitis.[6] The name cryptogenic obliterative (constrictive) bronchiolitis is used when a cause is unknown.[4]
Obliterative bronchiolitis is also not to be confused with bronchiolitis obliterans syndrome (BOS).[11][4] BOS is defined as a person who has had either a HSCT or lung transplant and develops symptoms or radiographic findings consistent with bronchiolitis obliterans, but has not been confirmed by biopsy.[22][38]
References
- "Bronchiolitis obliterans". GARD. 2012. Archived from the original on 21 January 2017. Retrieved 13 September 2016.
- Schlesinger C, Meyer CA, Veeraraghavan S, Koss MN (October 1998). "Constrictive (obliterative) bronchiolitis: diagnosis, etiology, and a critical review of the literature". Annals of Diagnostic Pathology. 2 (5): 321–34. doi:10.1016/S1092-9134(98)80026-9. PMID 9845757.
- Xie BQ, Wang W, Zhang WQ, Guo XH, Yang MF, Wang L, et al. (2014). "Ventilation/perfusion scintigraphy in children with post-infectious bronchiolitis obliterans: a pilot study". PLOS ONE. 9 (5): e98381. Bibcode:2014PLoSO...998381X. doi:10.1371/journal.pone.0098381. PMC 4031120. PMID 24852165.
- Lynch JP, Weigt SS, DerHovanessian A, Fishbein MC, Gutierrez A, Belperio JA (October 2012). "Obliterative (constrictive) bronchiolitis". Seminars in Respiratory and Critical Care Medicine. 33 (5): 509–32. doi:10.1055/s-0032-1325161. PMID 23001805.
- Lockey RF, Ledford DK (2014). Asthma: Comorbidities, Coexisting Conditions, and Differential Diagnosis. Oxford University Press. p. 111. ISBN 9780199918072. Archived from the original on 2017-09-08.
- Barker AF, Bergeron A, Rom WN, Hertz MI (May 2014). "Obliterative bronchiolitis". The New England Journal of Medicine. 370 (19): 1820–8. doi:10.1056/NEJMra1204664. PMID 24806161.
- Gosink BB, Friedman PJ, Liebow AA (April 1973). "Bronchiolitis obliterans. Roentgenologic-pathologic correlation". The American Journal of Roentgenology, Radium Therapy, and Nuclear Medicine. 117 (4): 816–32. doi:10.2214/ajr.117.4.816. PMID 4698820.
- Gourtsoyiannis NC, Ros PR (2005). Radiologic-Pathologic Correlations from Head to Toe: Understanding the Manifestations of Disease. Springer Science & Business Media. p. 154. ISBN 9783540266648. Archived from the original on 2017-09-08.
- Centers for Disease Control and Prevention (2002). Fixed obstructive lung disease in workers at a microwave popcorn factory (7th ed.).
- "More than a cold". Archived from the original on 2016-09-15. Retrieved 2016-08-18.
- Aguilar PR, Michelson AP, Isakow W (February 2016). "Obliterative Bronchiolitis". Transplantation. 100 (2): 272–83. doi:10.1097/TP.0000000000000892. PMID 26335918.
- Banks, Daniel E.; Bolduc, Caroline A.; Ali, Sayed; Morris, Michael J. (January 2018). "Constrictive Bronchiolitis Attributable to Inhalation of Toxic Agents: Considerations for a Case Definition". Journal of Occupational and Environmental Medicine. 60 (1): 90–96. doi:10.1097/JOM.0000000000001176. ISSN 1076-2752.
- Callahan SJ, Vranic A, Flors L, Hanley M, Stoler MH, Mehrad B (March 2019). "Sporadic Obliterative Bronchiolitis: Case Series and Systematic Review of the Literature". Mayo Clinic Proceedings. Innovations, Quality & Outcomes. 3 (1): 86–93. doi:10.1016/j.mayocpiqo.2018.10.003. PMC 6410330. PMID 30899912.
- Sam AH, Teo JT (2010). Rapid Medicine. Wiley-Blackwell. ISBN 978-1-4051-8323-9.
- Bairral BQ, Saito M, Morrone N (2012). "Activated charcoal bronchial aspiration". Jornal Brasileiro de Pneumologia. 38 (4): 533–4. doi:10.1590/S1806-37132012000400018. PMID 22964940.
- Bunawan H, Bunawan SN, Baharum SN, Noor NM (2015). "Sauropus androgynus (L.) Merr. Induced Bronchiolitis Obliterans: From Botanical Studies to Toxicology". Evidence-Based Complementary and Alternative Medicine. 2015: 714158. doi:10.1155/2015/714158. PMC 4564651. PMID 26413127.
- Brant & Helms (1999). Fundamentals of Diagnostic Radiology. Baltimore: Williams & Wilkins. ISBN 978-0-683-30093-2.
- Webb; et al. (2000). High Resolution CT of the Lung (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. ISBN 978-0-7817-0217-1.
- Brown, Jay A. "Haz-Map; Information on Hazardous Chemicals and Occupational Diseases". National Institutes of Health. Archived from the original on 2007-09-12. Retrieved 2007-09-09.
- Estenne M, Maurer JR, Boehler A, Egan JJ, Frost A, Hertz M, et al. (March 2002). "Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria". The Journal of Heart and Lung Transplantation. 21 (3): 297–310. doi:10.1016/S1053-2498(02)00398-4. PMID 11897517.
- Au BK, Au MA, Chien JW (July 2011). "Bronchiolitis obliterans syndrome epidemiology after allogeneic hematopoietic cell transplantation". Biology of Blood and Marrow Transplantation. 17 (7): 1072–8. doi:10.1016/j.bbmt.2010.11.018. PMC 3061253. PMID 21126596.
- Yadav H, Peters SG, Keogh KA, Hogan WJ, Erwin PJ, West CP, Kennedy CC (December 2016). "Azithromycin for the Treatment of Obliterative Bronchiolitis after Hematopoietic Stem Cell Transplantation: A Systematic Review and Meta-Analysis". Biology of Blood and Marrow Transplantation. 22 (12): 2264–2269. doi:10.1016/j.bbmt.2016.08.027. PMC 5116253. PMID 27575542.
- Colby TV (January 1998). "Bronchiolitis. Pathologic considerations". American Journal of Clinical Pathology. 109 (1): 101–9. doi:10.1093/ajcp/109.1.101. PMID 9426525.
- California Department of Public Health Archived 2009-10-16 at the Wayback Machine
- Harber P, Saechao K, Boomus C (2006). "Diacetyl-induced lung disease". Toxicological Reviews. 25 (4): 261–72. doi:10.2165/00139709-200625040-00006. PMID 17288497.
- "Preventing lung disease in workers who make or use flavorings". National Institute for Occupational Safety and Health. 2004. doi:10.26616/NIOSHPUB2004110. Archived from the original on 2006-07-18. Cite journal requires
|journal=(help) - Schachter EN (August 2002). "Popcorn worker's lung". The New England Journal of Medicine. 347 (5): 360–1. doi:10.1056/nejme020064. PMID 12151475.
- Egilman, David (2007). "Popcorn Workers Lung" (PDF). Archived from the original (PDF) on 2007-09-27. Retrieved 2007-08-09.
- Sauler M, Gulati M (December 2012). "Newly recognized occupational and environmental causes of chronic terminal airways and parenchymal lung disease". Clinics in Chest Medicine. 33 (4): 667–80. doi:10.1016/j.ccm.2012.09.002. PMC 3515663. PMID 23153608.
- "CDC - Flavorings-Related Lung Disease - NIOSH Workplace Safety and Health Topic". www.cdc.gov. Archived from the original on 17 October 2015. Retrieved 15 October 2015.
- Champs NS, Lasmar LM, Camargos PA, Marguet C, Fischer GB, Mocelin HT (2011-05-05). "Post-infectious bronchiolitis obliterans in children". Jornal de Pediatria. 87 (3): 187–98. doi:10.2223/JPED.2083. PMID 21547332.
- Hamada K, Oishi K, Hirano T, Shiinoki T, Shibuya K, Matsunaga K (January 2018). "Swyer-James Syndrome". American Journal of Respiratory and Critical Care Medicine. 197 (1): 130–131. doi:10.1164/rccm.201708-1691IM. PMID 29064268.
- Colom AJ, Teper AM, Vollmer WM, Diette GB (June 2006). "Risk factors for the development of bronchiolitis obliterans in children with bronchiolitis". Thorax. 61 (6): 503–6. doi:10.1136/thx.2005.044909. PMC 2111218. PMID 16517579.
- Rodrigues CM, Schiwe D, Campos NE, Niederauer F, Heinzmann-Filho JP (April 2019). "Exercise Capacity in Children and Adolescents With Post-Infectious Bronchiolitis Obliterans: A Systematic Review". Revista Paulista de Pediatria. 37 (2): 234–240. doi:10.1590/1984-0462/;2019;37;2;00017. PMC 6651318. PMID 30892545.
- http://www.usmedicine.com/compendium/where-theres-smoke-dod-investigates-causes-of-deployment-related-pulmonary-symptoms-reported-by-troops.html#.UsH-jNJDvSs Archived 2013-12-31 at the Wayback Machine
- Harrison Jacobs (5 November 2013). "Open-Air Burn Pits Leave Troops Sickly – Business Insider". Business Insider. Archived from the original on 22 December 2015. Retrieved 18 December 2015.
- Arakawa, H; Webb, W R (May 1998). "Air trapping on expiratory high-resolution CT scans in the absence of inspiratory scan abnormalities: correlation with pulmonary function tests and differential diagnosis". American Journal of Roentgenology. 170 (5): 1349–1353. doi:10.2214/ajr.170.5.9574614. ISSN 0361-803X.
- Estenne M, Maurer JR, Boehler A, Egan JJ, Frost A, Hertz M, et al. (March 2002). "Bronchiolitis obliterans syndrome 2001: an update of the diagnostic criteria". The Journal of Heart and Lung Transplantation. 21 (3): 297–310. doi:10.1016/S1053-2498(02)00398-4. PMID 11897517.
Further reading
- King MS, Eisenberg R, Newman JH, Tolle JJ, Harrell FE, Nian H, et al. (July 2011). "Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan". The New England Journal of Medicine. 365 (3): 222–30. doi:10.1056/NEJMoa1101388. PMC 3296566. PMID 21774710.
- Brown JA. "Bronchiolitis obliterans". Haz-Map Information on Hazardous Chemicals and Occupational Diseases. National Institutes of Health. Archived from the original on 2007-09-12. Retrieved 2007-09-09.
- "(NIOSH) Alert: Preventing lung disease in workers who make or use flavorings". National Institute for Occupational Safety and Health. 2004. doi:10.26616/NIOSHPUB2004110. Cite journal requires
|journal=(help) - "Flavorings-Related Lung Disease". National Institute for Occupational Safety and Health. 2018-11-21.
External links
| Classification |
|---|