Number needed to treat
The number needed to treat (NNT) is an epidemiological measure used in communicating the effectiveness of a health-care intervention, typically a treatment with medication. The NNT is the average number of patients who need to be treated to prevent one additional bad outcome (e.g. the number of patients that need to be treated for one of them to benefit compared with a control in a clinical trial). It is defined as the inverse of the absolute risk reduction, and computed as , where is the incidence in the treated (exposed) group, and is the incidence in the control (unexposed) group.[1]
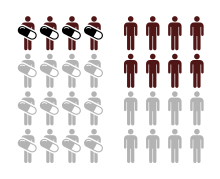
A type of effect size, the NNT was described in 1988 by McMaster University's Laupacis, Sackett and Roberts.[2] The ideal NNT is 1, where everyone improves with treatment and no one improves with control. The higher the NNT, the less effective the treatment is.[3]
NNT is similar to number needed to harm (NNH), where NNT usually refers to a therapeutic intervention and NNH to a detrimental effect or risk factor.
Relevance
The NNT is an important measure in pharmacoeconomics. If a clinical endpoint is devastating enough (e.g. death, heart attack), drugs with a high NNT may still be indicated in particular situations. If the endpoint is minor, health insurers may decline to reimburse drugs with a high NNT. NNT is significant to consider when comparing possible side effects of a medication against its benefits. For medications with a high NNT, even a small incidence of adverse effects may outweigh the benefits. Even though NNT is an important measure in a clinical trial, it is infrequently included in medical journal articles reporting the results of clinical trials.[4] There are several important problems with the NNT, involving bias and lack of reliable confidence intervals, as well as difficulties in excluding the possibility of no difference between two treatments or groups.[5]
NNT values are time-specific. For example, if a study ran for 5 years and another ran for 1 year, the NNT values would not be directly comparable.[6]
Explanation of NNT in practice
There are a number of factors that can affect the meaning of the NNT depending on the situation. The treatment may be a drug in the form of a pill or injection, a surgical procedure, or many other possibilities. The following examples demonstrate how NNT is determined and what it means. In this example, it is important to understand that every participant has the condition being treated, so there are only "diseased" patients who received the treatment or did not. This is typically a type of study that would occur only if both the control and the tested treatment carried significant risks of serious harm, or if the treatment was unethical for a healthy participant (for example, chemotherapy drugs or a new method of appendectomy - surgical removal of the appendix). Most drug trials test both the control and the treatment on both healthy and "diseased" participants. Or, if the treatment's purpose is to prevent a condition that is fairly common (an anticoagulant to prevent heart attack for example), a prospective study may be used. A study which starts with all healthy participants is termed a prospective study, and is in contrast to a retrospective study, in which some participants already have the condition in question. Prospective studies produce much higher quality evidence, but are much more difficult and time-consuming to perform.
In the table below:
- is the probability of seeing no improvement after receiving the treatment (this is the inverse of the probability of seeing improvement with the treatment). This measure applies only to the treated group.
- is the probability of seeing no improvement after receiving the control (this is the inverse of the probability of seeing improvement with only the control). This measure applies only to the control (unexposed) group. The control group may receive a placebo treatment, or in cases where the goal is to find evidence that a new treatment is more effective than an existing treatment, the control group will receive the existing treatment. The meaning of the NNT is dependent on whether the control group received a placebo treatment or an existing treatment, and, in cases where a placebo treatment is given, the NNT is also affected to the quality of the placebo (i.e. for participants, is the placebo completely indistinguishable from the tested treatment.
| Description | NNT | Interpretation | ||
|---|---|---|---|---|
| Perfect treatment, previously untreatable condition with no placebo effect involved | 0.0 | 1.0 | 1 | Half of participants receive the treatment, and half receive a control (which may be simply a placebo, or may be an existing treatment with a known effectiveness). Every person that receives the treatment shows improvement, which may be a reduction or halt in worsening of the condition, an improvement in the condition, or an outright cure of the condition. Every person in the control group shows no improvement, therefore the condition never improves on its own and the control is never effective. NNT is 1/(1.0-0.0), which is 1. |
| Very effective treatment with large improvement over control | 0.1 | 0.9 | 1.25 | For simplicity, a low number of participants will be used, thought scientific studies almost always require many more. Ten people receive the treatment, and ten receive a control. Of the ten in the treated group, nine show improvement, and one shows no improvement. In the control group, one person shows improvement and nine show none. Since one of those who received the control showed improvement without the treatment, it is said that one of the nine from the treated group would have improved without receiving the treatment. Therefore, one person’s outcome does not represent evidence that the treatment is better than the control. NNT is 1/(0.9-0.1), which is 1.25. The absolute risk reduction is 0.9-0.1, equal to 0.8. |
| Effective treatment with moderate improvement over control | 0.3 | 0.7 | 2.5 | Ten receive the treatment, and ten receive a control. In the treatment group, seven show improvement and three show none. In the control group, three show improvement and seven show none. Therefore, the treatment was more helpful than the control in three of ten cases, and was not any more helpful in seven. NNT is 1/(0.7 – 0.3), which is 2.5. |
| Effective treatment, but little improvement over control | 0.4 | 0.5 | 10 | Ten receive the treatment, and ten receive a control. Six improve with the treatment, and four do not. In the control group, five improve and five do not. Therefore, the treatment was more helpful than the control in only one of ten cases, and was not helpful is nine of ten. NNT is 1/(0.5 – 0.4), which is 10. |
| Not very effective treatment with little improvement over control | 0.8 | 0.9 | 10 | Ten receive the treatment, and ten receive a control. Two improve with the treatment and eight do not. In the control group, one improves and nine do not. Therefore, the treatment was more helpful than the control in only one of ten cases, and was not helpful is nine of ten. NNT is 1/(0.9 – 0.8), which is 10. |
| Very effective treatment, but with little improvement over control | 0.1 | 0.2 | 10 | Ten receive the treatment, and ten receive a control. Nine improve with the treatment and one does not. In the control group, eight improve and two do not. Therefore, the treatment was more helpful than the control in only one of ten cases, and was not helpful is nine of ten. NNT is 1/(0.2 – 0.1), which is 10. |
| Treatment is effective but worse than control | 0.2 | 0.1 | −10 | Ten receive the treatment, and ten receive a control. Eight improve with the treatment and two do not. In the control group, nine improve and one does not. Therefore, the treatment was less helpful than the control in one of ten cases. NNT is 1/(0.1 – 0.2), which is -10. Notice that, even though the treatment was effective in eight of ten cases (only one less than the previous example) the NNT has shifted from 10 to -10. This is because NNT measures how many patients must be given the treatment instead of the control in order to see improvement in one person. Since giving the treatment to ten people would cause one of those people to be worse than if they had received the control instead, the NNT is -10. |
Real life example
ASCOT-LLA manufacturer-sponsored study addressed the benefit of atorvastatin 10 mg (a cholesterol-lowering drug) in patients with hypertension (high blood pressure) but no previous cardiovascular disease (primary prevention). The trial ran for 3.3 years, and during this period the relative risk of a "primary event" (heart attack) was reduced by 36% (relative risk reduction, RRR). The absolute risk reduction (ARR), however, was much smaller, because the study group did not have a very high rate of cardiovascular events over the study period: 2.67% in the control group, compared to 1.65% in the treatment group.[7] Taking atorvastatin for 3.3 years, therefore, would lead to an ARR of only 1.02% (2.67% minus 1.65%). The number needed to treat to prevent one cardiovascular event would then be 98.04 for 3.3 years.[8]
Numerical example
| Example of risk reduction | |||
|---|---|---|---|
| Experimental group (E) | Control group (C) | Total | |
| Events (E) | EE = 15 | CE = 100 | 115 |
| Non-events (N) | EN = 135 | CN = 150 | 285 |
| Total subjects (S) | ES = EE + EN = 150 | CS = CE + CN = 250 | 400 |
| Event rate (ER) | EER = EE / ES = 0.1, or 10% | CER = CE / CS = 0.4, or 40% | |
| Equation | Variable | Abbr. | Value |
|---|---|---|---|
| CER - EER | absolute risk reduction | ARR | 0.3, or 30% |
| (CER - EER) / CER | relative risk reduction | RRR | 0.75, or 75% |
| 1 / (CER − EER) | number needed to treat | NNT | 3.33 |
| EER / CER | risk ratio | RR | 0.25 |
| (EE / EN) / (CE / CN) | odds ratio | OR | 0.167 |
| (CER - EER) / CER | preventable fraction among the unexposed | PFu | 0.75 |
See also
- Population Impact Measures
- Number needed to vaccinate
- Number needed to harm
References
- Dictionary of Epidemiology - Oxford Reference. Oxford University Press. 2016-07-21. doi:10.1093/acref/9780199976720.001.0001. ISBN 9780199976720. Retrieved 2018-05-09.
- Laupacis A, Sackett DL, Roberts RS (1988). "An assessment of clinically useful measures of the consequences of treatment". N. Engl. J. Med. 318 (26): 1728–33. doi:10.1056/NEJM198806303182605. PMID 3374545.
- "Number Needed to Treat". Bandolier. Retrieved 2017-04-21.
- Nuovo, J.; Melnikow J.; Chang D. (2002-06-05). "Reporting number needed to treat and absolute risk reduction in randomized controlled trials". JAMA. 287 (21): 2813–4. doi:10.1001/jama.287.21.2813. PMID 12038920.
- Hutton JL (2010). "Misleading Statistics: The Problems Surrounding Number Needed to Treat and Number Needed to Harm". Pharm Med. 24 (3): 145–9. doi:10.1007/BF03256810. ISSN 1178-2595.
- Palle Mark Christensen; Kristiansen, IS (2006). "Number-Needed-to-Treat (NNT) – Needs Treatment with Care". Basic & Clinical Pharmacology & Toxicology. 99 (1): 12–16. doi:10.1111/j.1742-7843.2006.pto_412.x. PMID 16867164. Archived from the original on 2013-01-05.
- Sever PS, Dahlöf B, Poulter NR, et al. (2003). "Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial". Lancet. 361 (9364): 1149–58. doi:10.1016/S0140-6736(03)12948-0. PMID 12686036.
- John Carey. "Do Cholesterol Drugs Do Any Good?". Business Week. Archived from the original on December 28, 2014. Retrieved 2008-03-31.