Nightmare
A nightmare, also called a bad dream,[1] is an unpleasant dream that can cause a strong emotional response from the mind, typically fear but also despair, anxiety and great sadness. However, psychological nomenclature differentiates between nightmares and bad dreams, specifically, people remain asleep during bad dreams whereas nightmares awaken individuals. Further, the process of psychological homeostasis employs bad dreams to protect an individual's Homeostatically Protected Mood (HPMood) from the impact of elevated anxiety levels. During sleep, nightmares indicate the failure of the homeostatic system employing bad dreams to extinguish anxiety accumulated throughout the day.[2] The dream may contain situations of discomfort, psychological or physical terror or panic. After a nightmare, a person will often awaken in a state of distress and may be unable to return to sleep for a short period of time.[3]
| Nightmare | |
|---|---|
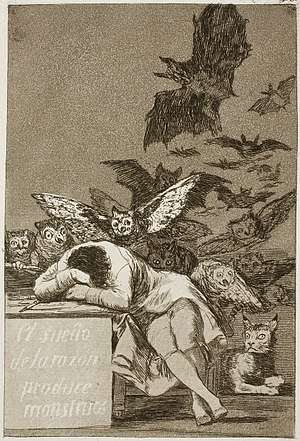 | |
| The Sleep of Reason Produces Monsters (Francisco de Goya, c.1797) | |
| Specialty | Psychiatry |
| Causes | Stress or Anxiety |
Nightmares can have physical causes such as sleeping in an uncomfortable position or having a fever, or psychological causes such as stress or anxiety. Eating before going to sleep, which triggers an increase in the body's metabolism and brain activity, is a potential stimulus for nightmares.[4]
Recurrent nightmares may require medical help, as they can interfere with sleeping patterns and cause insomnia.
Signs and symptoms
Those with nightmares experience abnormal sleep architecture and that the results of having a nightmare during the night were very similar to those of people who have insomnia. This is thought to be caused by frequent nocturnal awakenings and fear of falling asleep.[5]
Classification
According to the International Classification of Sleep Disorders-Third Edition (ICSD-3) the nightmare disorder, together with REM sleep behaviour disorder (RBD) and recurrent isolated sleep paralysis form the REM-related parasomnias subcategory of the Parasomnias cluster.[6] Nightmares may be idiopathic without any signs of psychopathology or associated with disorders like stress, anxiety, substance abuse, psychiatric illness or PTSD (>80% of PTSD patients report nightmares).[7] As regarding the dream content of the dreams they are usually imprinting negative emotions like sadness, fear or rage.[8] According to the clinical studies the content can range from being chased, injury or death of others,falling, natural disasters or accidents. Typical dreams or recurrent dreams may also have some of these topics.[9]
Cause
Scientific research shows that nightmares may have many causes. In a study focusing on children, researchers were able to conclude that nightmares directly correlate with the stress in children’s lives. Children who experienced the death of a family member or a close friend or know someone with a chronic illness have more frequent nightmares than those who are only faced with stress from school or stress from social aspects of daily life.[10] A study researching the causes of nightmares focuses on patients who have sleep apnea. The study was conducted to determine whether or not nightmares may be caused by sleep apnea, or being unable to breathe. In the nineteenth century, authors believed that nightmares were caused by not having enough oxygen, therefore it was believed that those with sleep apnea had more frequent nightmares than those without it. The results actually showed that healthy people have more nightmares than the sleep apnea patients.[11] Another study supports the hypothesis. In this study, 48 patients (aged 20–85 yrs) with obstructive airways disease (OAD), including 21 with and 27 without asthma, were compared with 149 sex- and age-matched controls without respiratory disease. OAD subjects with asthma reported approximately 3 times as many nightmares as controls or OAD subjects without asthma.[12] The evolutionary purpose of nightmares then could be a mechanism to awaken a person who is in danger.
Lucid-dreaming advocate Stephen LaBerge has outlined a possible reason for how dreams are formulated and why nightmares occur with a high frequency. To LaBerge, a dream starts with an individual thought or scene, such as walking down a dimly lit street. Since dreams are not predetermined, the brain responds to the situation by either thinking a good thought or a bad thought, and the dream framework follows from there. Since the prominence of bad thoughts in dreams is higher than good, the dream will proceed to be a nightmare.[13]
There is a view, possibly featured in the story A Christmas Carol, that eating cheese before sleep can cause nightmares, but there is little scientific evidence for this phenomenon.[14]
Treatment
Sigmund Freud and Carl Jung seemed to have shared a belief that people frequently distressed by nightmares could be re-experiencing some stressful event from the past. [15] Both perspectives on dreams suggest that therapy can provide relief from the dilemma of the nightmarish experience.
Halliday (1987), grouped treatment techniques into four classes. Direct nightmare interventions that combine compatible techniques from one or more of these classes may enhance overall treatment effectiveness:[16]
- Analytic and cathartic techniques
- Storyline alteration procedures
- Face-and-conquer approaches
- Desensitization and related behavioral techniques.
Posttraumatic stress disorder
Reccurring post-traumatic stress disorder nightmares in which traumas are re-experienced respond well to a technique called imagery rehearsal. This involves dreamers coming up with alternative, mastery outcomes to the nightmares, mentally rehearsing those outcomes while awake, and then reminding themselves at bedtime that they wish these alternate outcomes should the nightmares reoccur. Research has found that this technique not only reduces the occurrence of nightmares and insomnia,[17] but also improves other daytime PTSD symptoms.[18] The most common variations of Imagery Rehearsal Therapy (IRT) "relate to the number of sessions, duration of treatment, and the degree to which exposure therapy is included in the protocol".[19] The medication prazosin appears useful in decreasing the number of nightmares and the distress caused by them in people with PTSD.[20]
Epidemiology
Fearfulness in waking life is correlated with nightmares.[21] Studies of dreams have estimated that about 75% of the time, the emotions evoked by dreams are negative.[21] However, it is worth noting that people are more likely to remember unpleasant dreams.
One definition of "nightmare" is a dream which causes one to wake up in the middle of the sleep cycle and experience a negative emotion, such as fear. This type of event occurs on average once per month. They are not common in children under five, but they are more common in young children (25% experiencing a nightmare at least once per week), most common in teenagers, and common in adults (dropping in frequency about one third from age 25 to 55).[21] The prevalence in children (5-12 years old) is between 20-30% and in adults 8-30%.[8]
Etymology
The word "nightmare" is derived from the Old English "mare", a mythological demon or goblin who torments others with frightening dreams.[22] Subsequently, the prefix "night-" was added to stress the dream aspect. The word "nightmare" is cognate with the Dutch term nachtmerrie and German Nachtmahr (dated).
See also
- Succubus
- False awakening
- Hag in folklore
- Lucid dream
- Mare (folklore)
- Moroi
- Night terror
- Nightmare disorder
- Nocnitsa
- Sleep disorder
- Sleep paralysis
- Horror and terror
- A Christmas Carol
References
- Harper, Douglas. "nightmare". Online Etymology Dictionary. Retrieved July 11, 2016.
- Tunbridge, Lindsay (2014), International Journal of Dream Research, Vol 7 Issue 1, http://nbn-resolving.de/urn:nbn:de:bsz:16-ijodr-119592
- American Psychiatric Association (2000), Diagnostic and Statistical Manual of Mental Disorders, 4th ed, TR, p. 631
- Stephen, Laura (2006). "Nightmares". Psychologytoday.com. Archived from the original on 31 August 2007. Cite journal requires
|journal=(help) - Simor, Pé, et al. "Disturbed Dreaming and Sleep Quality: Altered Sleep Architecture in Subjects with Frequent Nightmares."European Archives of Psychiatry and Clinical Neuroscience 262.8 (2012): 687-96. ProQuest. Web. 24 Apr. 2014.
- Sateia, Michael J (2014). "International Classification of Sleep Disorders-Third Edition". Chest. 146 (5): 1387–1394. doi:10.1378/chest.14-0970. ISSN 0012-3692. PMID 25367475.
- Morgenthaler, Timothy I.; Auerbach, Sanford; et, al. (2018). "Position Paper for the Treatment of Nightmare Disorder in Adults: An American Academy of Sleep Medicine Position Paper". Journal of Clinical Sleep Medicine. 14 (6): 1041–1055. doi:10.5664/jcsm.7178. ISSN 1550-9389. PMC 5991964. PMID 29852917.
- Peter, Helga; Penzel, Thomas; Jörg, Hermann Peter (2007). Enzyklopädie der Schlafmedizin. Heidelberg: Springer Medizin Verlag. ISBN 978-3-540-28839-8.
- Schredl, Michael; Göritz, Anja S. (2018). "Nightmare Themes: An Online Study of Most Recent Nightmares and Childhood Nightmares". Journal of Clinical Sleep Medicine. 14 (3): 465–471. doi:10.5664/jcsm.7002. PMC 5837849. PMID 29458691.
- Schredl, Michael, et al. "Nightmares and Stress in Children." Sleep and Hypnosis 10.1 (2008): 19-25. ProQuest. Web. 29 Apr. 2014.
- Schredl, Michael, et al. "Nightmares and Oxygen Desaturations: Is Sleep Apnea Related to Heightened Nightmare Frequency?" Sleep and Breathing 10.4 (2006): 203-9. ProQuest. Web. 24 Apr. 2014.
- "Prevalence of nightmares among patients with asthma and chronic obstructive airways disease | Request PDF".
- Stephen, LaBerge (1990). Exploring the World of Lucid Dreaming. New York: BALLANTINE BOOKS. pp. 65–66.
- Hammond, Claudia (17 April 2012). "Does cheese give you nightmares?". BBC. Retrieved 7 October 2018.
- Coalson, Bob (1995). "Nightmare help: Treatment of trauma survivors with PTSD". Psychotherapy: Theory, Research, Practice, Training. 32 (3): 381–388. doi:10.1037/0033-3204.32.3.381.
- Cushway, Delia; Sewell, Robyn (2012). Therapy with Dreams and Nightmares: Theory, Research & Practice (2 ed.). SAGE Publications Ltd. p. 73. ISBN 9781446247105.
- Davis, J. L.; Wright, D. C. (2005). "Case Series Utilizing Exposure, Relaxation, and Rescripting Therapy: Impact on Nightmares, Sleep Quality, and Psychological Distress". Behavioral Sleep Medicine. 3 (3): 151–157. doi:10.1207/s15402010bsm0303_3. PMID 15984916.
- Krakow, B.; Hollifield, M.; Johnston, L.; Koss, M.; Schrader, R.; Warner, T. D.; Tandberg, D.; Lauriello, J.; McBride, L. (2001). "Imagery Rehearsal Therapy for Chronic Nightmares in Sexual Assault Survivors with Posttraumatic Stress Disorder: A Randomized Controlled Trial". JAMA: The Journal of the American Medical Association. 286 (5): 537–45. doi:10.1001/jama.286.5.537. PMID 11476655.
- Lu, M.; Wagner, A.; Van Male, L.; Whitehead, A.; Boehnlein, J. (2009). "Imagery rehearsal therapy for posttraumatic nightmares in U.S. Veterans". Journal of Traumatic Stress. 22 (3): 236–239. doi:10.1002/jts.20407. PMID 19444882., p. 234
- El-Solh, AA (2018). "Management of nightmares in patients with posttraumatic stress disorder: current perspectives". Nature and Science of Sleep. 10: 409–420. doi:10.2147/NSS.S166089. PMC 6263296. PMID 30538593.
- The Science Behind Dreams and Nightmares, Talk of the Nation, National Public Radio. 30 October 2007.
- Liberman, Anatoly (2005). Word Origins And How We Know Them. Oxford: Oxford University Press. p. 87. ISBN 978-0-19-538707-0. Retrieved 29 March 2012.
Further reading
- Anch, A. M.; Browman, C. P.; Mitler, M. M.; Walsh, J. K. (1988). Sleep: A Scientific Perspective. New Jersey: Prentice-Hall.
- Harris, J. C. (2004). "The Nightmare". Archives of General Psychiatry. 61 (5): 439–40. doi:10.1001/archpsyc.61.5.439. PMID 15123487.
- Husser, J.-M.; Mouton, A., eds. (2010). Le Cauchemar dans les sociétés antiques. Actes des journées d'étude de l'UMR 7044 (15–16 Novembre 2007, Strasbourg) (in French). Paris: De Boccard.
- Jones, Ernest (1951). On the Nightmare. ISBN 978-0-87140-912-6.
- Forbes, D.; et al. (2001). "Brief Report: Treatment of Combat-Related Nightmares Using Imagery Rehearsal: A Pilot Study". Journal of Traumatic Stress. 14 (2): 433–442. doi:10.1023/A:1011133422340. PMID 11469167.
- Siegel, A. (2003). "A mini-course for clinicians and trauma workers on posttraumatic nightmares".
- Burns, Sarah (2004). Painting the Dark Side : Art and the Gothic Imagination in Nineteenth-Century America. Ahmanson-Murphy Fine Are Imprint. University of California Press. ISBN 978-0-520-23821-3.
- Davenport-Hines, Richard (1999). Gothic: Four Hundred Years of Excess, Horror, Evil and Ruin. North Point Press. pp. 160–61.
- Hill, Anne (2009). What To Do When Dreams Go Bad: A Practical Guide to Nightmares. Serpentine Media. ISBN 978-1-887590-04-4.
- Simons, Ronald C.; Hughes, Charles C., eds. (1985). Culture-Bound Syndromes. Springer.
- Sagan, Carl (1997). The Demon-Haunted World: Science as a Candle in the Dark.
- Coalson, Bob (1995). "Nightmare help: Treatment of trauma survivors with PTSD". Psychotherapy: Theory, Research, Practice, Training. 32 (3): 381–388. doi:10.1037/0033-3204.32.3.381.
- "Nightmares? Bad Dreams, or Recurring Dreams? Lucky You!". Archived from the original on 19 March 2012. Retrieved 8 December 2015.
- Halliday, G. (1987). "Direct psychological therapies for nightmares: A review". Clinical Psychology Review. 7 (5): 501–523. doi:10.1016/0272-7358(87)90041-9.
- Doctor, Ronald M.; Shiromoto, Frank N., eds. (2010). "Imagery Rehearsal Therapy (IRT)". The Encyclopedia of Trauma and Traumatic Stress Disorders. New York: Facts on File. p. 148.
- Mayer, Mercer (1976). There's a Nightmare in My Closet. [New York]: Puffin Pied Piper.
- Moore, Bret A.; Kraków, Barry (2010). "Imagery rehearsal therapy: An emerging treatment for posttraumatic nightmares in veterans". Psychological Trauma: Theory, Research, Practice, and Policy. 2 (3): 232–238. doi:10.1037/a0019895.
External links
| Classification |
|---|
| Look up nightmare in Wiktionary, the free dictionary. |
![]()
| Wikisource has original text related to this article: |