Nightmare disorder
Nightmare disorder, also known as dream anxiety disorder, is a sleep disorder characterized by frequent nightmares. The nightmares, which often portray the individual in a situation that jeopardizes their life or personal safety, usually occur during the REM stages of sleep. Though most people have experienced at least one nightmare during their life, subjects with nightmare disorder experience them with a greater frequency. The disorder's DSM-IV number is 307.47.
| Nightmare disorder | |
|---|---|
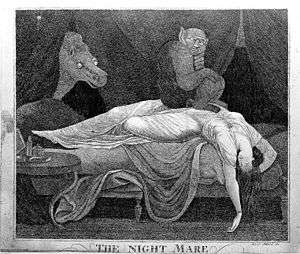 | |
| The Nightmare, by Johann Heinrich Füssli | |
| Specialty | Psychiatry |
| Frequency | c. 4%[1] |
Nightmare disorders are included in the parasomnias, which cover all the unusual behaviours during sleep.[2] Nightmare disorders can be confused with sleep terror disorders.[3] The difference is that after a sleep terror episode, the patient wakes up with more dramatic symptom than for a nightmare disorder, such as screaming and crying.[3] Furthermore, they don't remember the reason of the fear, while a patient with a nightmare disorder remembers every detail of the dream.[3] Finally, the sleep terrors usually occur during NREM Sleep.[4]
Nightmares also have to be distinguished from bad dreams, which are less emotionally intense.[5] Furthermore, nightmares contain more stories of aggression than bad dreams and more unhappy endings.[5] Finally, people experiencing nightmares feel more fear than for bad dreams.[5]
The treatment depends whether or not there is a comorbid PTSD diagnosis.[1] About 4% of American adults are affected.[1]
Signs and symptoms
During the nightmare, the sleeper may scream and yell out things. The nightmare sufferer is often awakened by these threatening, frightening dreams and can often vividly remember their experience. Upon awakening, the sleeper is usually alert and oriented within their surroundings, but may have an increased heart rate and symptoms of anxiety, like sweating. They may have trouble falling back to sleep for fear they will experience another nightmare.
A person experiencing nightmare disorder may have trouble going through everyday tasks; anxiety and lack of sleep caused by the fearful dreams may hinder the individual from completing everyday jobs efficiently and correctly. Upon experiencing this, these nightmare sufferers may consult with a psychiatrist.
The sleeper may have recurring episodes of awakening while recalling the intensely disturbing dream manifestations which usually result from fear or anxiety, but can also be triggered from anger, sadness, disgust, and other dysphoric emotions. The sleeper also can endure at least one of the following two features: delayed return of going back to sleep after episodes, and having episodes in the latter half of the patient's sleep.[6]
Consequences
Nightmare disorder is common: it affects about 4% of the adult population. Even if children have more nightmares than adults, only 1% of children meet the criteria of the disorder.[2] Nightmare disorder can impair the quality of life for the people who are affected with the condition. It can make the patient avoid sleep, which leads to sleep deprivation which could lead to even more intense nightmares for the patient. Some other consequences of the nightmare disorder are fatigue and insomnia.[6]
Nightmare disorders have negative consequences in several fields, such as sleep, cognitive and emotional functioning and well-being.[7] Nightmares can also have negative impact on the bed partner's life.[8]
Content of idiopathic nightmares
Physical aggression is the main theme of nightmares.[5] Other fields, such as interpersonal conflict, failure, helplessness, apprehension, being chased, accident, evil force, disaster, insects and environmental abnormality could also be part of nightmares.[5] Fear is the most frequent emotion associated with these nightmares, even if other emotions such as sadness, anger, and confusion can also be present.[5]
Criteria
According to the International Classification of Sleep Disorders, the criteria needed to diagnose a nightmare disorder are the following.[9] First, the presence of frequent nightmares that imply a danger for the person and that impact mood in a negative way is needed.[9] Second, when waking up from nightmares, the person behaves in an alert way.[9] Finally, the disorder has to impact clinically in a significative way the personal, social or professional functioning, in areas such as mood, sleep, cognition, behaviour, fatigue, family and occupation.[9]
Causes
Nightmares can be caused by extreme pressure or irritation if no other mental disorder is discovered. The death of a loved one or a stressful life event can be enough to cause a nightmare but mental conditions such as post-traumatic stress disorder and other psychiatric disorders have been known to cause nightmares as well. If the individual is on medication, the nightmares may be attributed to some side effects of the drug. Amphetamines, antidepressants, and stimulants like cocaine and caffeine can cause nightmares. Blood pressure medication, levodopa and medications for Parkinson's disease have also been known to cause nightmares.[10]
The nightmares may be idiopathic or could be associated with psychiatric disorders like post-traumatic stress disorder, schizophrenia, and borderline personality disorder. Nightmares can also be triggered by stress and anxiety and substance abuse, such as drugs that affect the neurotransmitters norepinephrine and dopamine and serotonin. Nevertheless, causality between drugs such as beta-blockers or alpha-agonists and nightmares is still unclear and further researches need to be done to investigate the biochemical mechanisms of nightmares.[4]
Eighty percent of patients who suffer from PTSD report nightmares. Patients suffering from PTSD have symptoms that are classified into three clusters: intrusive/re-experiencing, numbing, and hyperarousal. Nightmares are usually considered to be part of the intrusive/re-experiencing symptom.[6]
Some differences are existing between idiopathic and PTSD related nightmares.[11] A PTSD person having nightmares would wake up during the night more frequently and for a longer time than with idiopathic nightmares.[11] Consequently, people with PTSD would have a poorer sleep quality.[11] Furthermore, nightmares related to PTSD would be more stressful than idiopathic ones.[11] However, further studies have to be conducted in this area to obtain more reliable results.[4]
Assessment
Polysomnography records physiological parameters, such as electroencephalography (EEG), electromyography (EMG) and electrooculography (EOG) in a sleep laboratory.[12] However, the frequency of posttraumatic nightmares tends to decrease in an artificial lab setting, which would impact the content of nightmares.[4] Consequently, assessment of nightmare disorders using polysomnography has to last for a longer period, in order to let the patient getting used to the articial environnement.[4]
Self-report by a questionnaire or by a diary is another way to investigate nightmare disorders.[4] However, these methods are questionable.[4] Indeed, when filling out questionnaires with questions about a long period, people often tend to underestimate the frequency of their nightmares because of forgetting.[4] On the contrary, filling out a diary every day may lead to an overestimation of the numbers of nightmares, because of the focusing on this phenomenon.[4]
Comorbidity
Studies have reported that nightmare disorders were present in 50- 70% of the cases for PTSD, in 17.5% for depression, in 18.3% for insomnia, in 16.7% for schizophrenia and in 49% for borderline personality disorders.[13] For all psychiatric disorders taken together, nightmare disorders are present in 29.9% of the cases, a much bigger rate than for the general population, which is 2-5%.[13] Nightmare disorders can also be associated with sleep disorders such as night terrors, chronic insomnia and sleep-disordered breathing.[4] The presence of nightmares before a trauma would influence severity of PTSD symptoms.[8] Furthermore, having nightmares is linked to a significantly higher risk of attempting suicide and of death by suicide.[8]
Nightmares also seem to be correlated with some personality factors.[4] Studies found an association between anxiety, depression and nightmares in insomnia,[14] while only small relationship was found in other populations.[15] Neuroticism would be also link to nightmares.[16] Nevertheless, people with a higher score of neuroticism could be better at recalling their nightmares during the self-report assessment, which could have an influence on this association.[4]
Treatment
Stress reduction techniques such as yoga, meditation and exercise may help to eliminate stress and create a more peaceful sleeping atmosphere.[17]
Diagnosis and medication can only be given to patients that report the recurring nightmares to a psychiatrist or other physician. Medications like prazosin are sometimes used to treat nightmares in people with PTSD.[18][19][20] Therapy usually helps to deal with the frightening themes of the nightmares and alleviate the recurrence of the dreams. The persistent nightmares will usually improve as the patient gets older. Therapy is usually efficient to treat chronic nightmares in PTSD disorder or in other population.[20] Medication has shown efficacy to treat chronic nightmares among a PTSD population but the impact of pharmacological treatments on other populations, such as drug-related nightmares, are unknown.[20] Furthermore, patients usually take more than one medication at a time, whatever the cause related to nightmares, leading to possible interactive effects.[20]
Eye Movement Desensitization and Reprocessing (EMDR) has demonstrated a significant nightmares’ reduction, especially for the treatment of PTSD.[21] Silver, Brooks and Obenchain have found a decrease of the nightmares with Vietnam War veterans after 90 days of EMDR.[22] Jayatunge has found significant results with people who have survived to a tsunami.[23] Greenwald has successfully used the EMDR with children.[24] There wasn't any negative consequence due to the EMDR sessions.
Research has been undertaken to investigate if sufferers of nightmares could benefit from the ability to be aware that they are indeed dreaming, a process known as lucid dreaming.[25][26] The Lucid Dreaming Therapy is a specific method of the Imagery Rehearsal Therapy. The dreamer is conscious during his dream and can modulate it. Consequently, anxiety decreases, controllability increases, expectations change, which will impact the frequency of nightmares.[4][27] Several studies have shown significant results with the lucid dreaming therapy. Two studies indicate a decrease of the nightmare frequency after only 12 weeks and one study shows, in 80% of the cases, a total disappearance of the nightmares after one year.[21] Although these studies showed the efficacy of this therapy in the reduction of nightmare frequency on patients from the general population,[28] so far evidence for this treatment is still weak.[29]
Imagery Rehearsal Therapy has been shown as efficient to treat nightmare disorder in PTSD as well as in non PTSD populations.[20] In this treatment, the person has to write a new scenario of the nightmare with positive images that will be rehearsed during 10 to 20 minutes per day, in order to change the negative content of the nightmare.[20] Cognitive Behavioral Therapy for Insomnia is also efficient to treat nightmares in the PTSD population.[30] This method aims to change sleep habits with a clinician's help and the use of tools such as a sleep diary.[31]
Exposure, relaxation and rescripting therapy is used to treat PTSD related nightmares.[8] This intervention combine Imagery Rehearsal Therapy with exposure and relaxation techniques.[8] The main objective is to work on the trauma related themes of nightmares.[8]
Systematic Desensitization, using graduated exposure, has been shown to be efficient to treat chronic nightmares.[20] The person has to face the frightening elements of nightmares in a gradually way, from the less to the most stressful.[20] When the person starts to feel unsecure, she has to manage the stress by applying a relaxation technique.[20]
Pharmacological treatments could be also efficient to treat nightmare disorder.[8] Most of the treatments were assessed to patients suffering from PTSD.[21] The most efficient is an alpha-blocker, named Prazosin, which reduce tone during sleep by blocking noradrenergic receptors.[8] Prazosin would significantly decrease the number of PTSD related nightmares and would therefore improve sleep quality.[8] However, only few studies considered the effect of Prazosin in idiopathic nightmares.[8] Benzodiazepines are also often used to treat nightmare disorder, despite the lack of efficacy demonstrated in empirical studies.[8] Some patients were also treated with atypical antipsychotic medications.[21] Olanzapine has quickly decreased the nightmares.[21] Two studies have shown the positive effects of Risperidone.[21] Aripiprazol is more tolerated than olanzapine and has demonstrated substantial improvement in the nightmare frequency.[21] Some other drugs as clonidine, cyproheptadine, fluvoxamine, gabapentin, nabilone, phenelzine, topiramate or trazodone have presented an amelioration of the nightmares.[21] But some further researches are needed.[21]
Epidemiology
About 4% of American adults are affected by nightmare disorders.[1] Women seem to be more affected than men, the ratio being 2-4 : 1.[4] This inequality decreases with aging because of a less high prevalence in elderly women.[4] However, it is still unclear if the difference of prevalence between men and women is real or if it reflects a higher dream recall capacity of women.[4]
According to studies, children at the age of 6–10 years are 41% more likely to experience nightmares and 22% at the age of 11.[32] Children with persistent nightmares range from 10% to 50%.[3] However, only 1% of children meet the criteria of a nightmare disorder.[2] Some factors tend to predict the development of a disorder from the presence of nightmares during childhood, such as a fear of going to sleep or going back to bed after a nightmare, an irregular sleep life and an avoidance of thinking about the nightmare.[4]
Research
- Dissociative disorders are usually paired with Nightmare Disorder 57% of the time. Nightmare disorder is believed to be associated with Dissociative Disorders as a defense mechanism that is used to escape from the traumatic event that caused the Dissociative Disorder. People with Dissociative Disorder and Nightmare disorder are more likely to self-mutilate, attempt suicide, and have Borderline Personality Disorder.[33]
- Borderline personality disorder with Nightmare Disorder is very common, since the stages of sleep vary from that of a normal person (i.e. increased stage one sleep, and less stage four sleep). People with Borderline Personality disorder and Nightmare Disorder are usually the severest of those who have Borderline Personality Disorder; therefore, treating those with Nightmare Disorder may also help some with Borderline Personality Disorder.[34]
- Hypnosis seems to be a new and effective treatment for those with Nightmare Disorder, since it increases relaxation.[35]
- Nightmare disorder is also associated with those who have lower cholesterol. This connection is unclear; however, cholesterol may affect other hormones in the body (such as serotonin) which may affect one's sleep.[36]
References
- Morgenthaler, Timothy I.; Auerbach, Sanford; Casey, Kenneth R.; Kristo, David; Maganti, Rama; Ramar, Kannan; Zak, Rochelle; Kartje, Rebecca (15 June 2018). "Position Paper for the Treatment of Nightmare Disorder in Adults: An American Academy of Sleep Medicine Position Paper". Journal of Clinical Sleep Medicine. 14 (6): 1041–1055. doi:10.5664/jcsm.7178. PMC 5991964. PMID 29852917.
- Agargun, Mehmet Y; Cilli, Ali Savas; Sener, Sahnur; Bilici, Mustafa; Ozer, Omer Akil; Selvi, Yavuz; Karacan, Elvan (June 2004). "The Prevalence of Parasomnias in Preadolescent School-aged Children: a Turkish Sample". Sleep. 27 (4): 701–705. doi:10.1093/sleep/27.4.701. ISSN 1550-9109. PMID 15283005.
- "Nightmare disorder". minddisorders.com.
- Spoormaker, Victor I.; Schredl, Michael; Bout, Jan van den (2006-02-01). "Nightmares: from anxiety symptom to sleep disorder". Sleep Medicine Reviews. 10 (1): 19–31. doi:10.1016/j.smrv.2005.06.001. ISSN 1087-0792. PMID 16377217.
- Zadra, Antonio; Robert, Geneviève (2014-02-01). "Thematic and Content Analysis of Idiopathic Nightmares and Bad Dreams". Sleep. 37 (2): 409–417. doi:10.5665/sleep.3426. ISSN 0161-8105. PMC 3900621.
- "Journal of Clinical Sleep Medicine - Research & Review Articles in Sleep Medicine". jcsm.aasm.org. Retrieved 2018-10-07.
- Schagen, Annette van; Lancee, Jaap; Swart, Marijke; Spoormaker, Victor; Bout, Jan van den (2017). "Nightmare Disorder, Psychopathology Levels, and Coping in a Diverse Psychiatric Sample". Journal of Clinical Psychology. 73 (1): 65–75. doi:10.1002/jclp.22315. ISSN 1097-4679. PMID 27100372.
- Nadorff, Michael R.; Lambdin, Karen K.; Germain, Anne (2014-04-01). "Pharmacological and non-pharmacological treatments for nightmare disorder". International Review of Psychiatry. 26 (2): 225–236. doi:10.3109/09540261.2014.888989. ISSN 0954-0261. PMID 24892897.
- Sateia, Michael J (2014-11-01). "International Classification of Sleep Disorders-Third Edition". Chest. 146 (5): 1387–1394. doi:10.1378/chest.14-0970. ISSN 0012-3692. PMID 25367475.
- "Nightmare Disorder". The Gale Encyclopedia of Mental Health. January 1, 2008. Archived from the original on May 29, 2016. Retrieved April 14, 2016.
Nightmares can be a side effect of some medications or drugs of abuse, including drugs given for high blood pressure; levodopa and other drugs given to treat Parkinson’s disease; amphetamines, cocaine and other stimulants; and some antidepressants.
– via HighBeam (subscription required) - Germain, Anne; Nielsen, Tore A (2003-11-15). "Sleep pathophysiology in posttraumatic stress disorder and idiopathic nightmare sufferers". Biological Psychiatry. 54 (10): 1092–1098. doi:10.1016/S0006-3223(03)00071-4. ISSN 0006-3223.
- Berry, Richard B.; Budhiraja, Rohit; Gottlieb, Daniel J.; Gozal, David; Iber, Conrad; Kapur, Vishesh K.; Marcus, Carole L.; Mehra, Reena; Parthasarathy, Sairam (2012-10-15). "Rules for Scoring Respiratory Events in Sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events". Journal of Clinical Sleep Medicine. doi:10.5664/jcsm.2172. ISSN 1550-9389. PMC 3459210.
- Swart, Marijke L.; van Schagen, Annette M.; Lancee, Jaap; van den Bout, Jan (2013). "Prevalence of Nightmare Disorder in Psychiatric Outpatients". Psychotherapy and Psychosomatics. 82 (4): 267–268. doi:10.1159/000343590. ISSN 1423-0348. PMID 23735876.
- Guilleminault, C.; Morselli, P. L.; Ohayon, M. M. (1997-05-01). "Prevalence of Nightmares and Their Relationship to Psychopathology and Daytime Functioning in Insomnia Subjects". Sleep. 20 (5): 340–348. doi:10.1093/sleep/20.5.340. ISSN 0161-8105. PMID 9381055.
- Puska, Pekka; Lehtonen, Johannes; Vartiainen, Erkki; Viinamäki, Heimo; Tuomilehto, Jaakko; Tanskanen, Antti (2001-10-01). "Nightmares as Predictors of Suicide". Sleep. 24 (7): 845–848. doi:10.1093/sleep/24.7.845. ISSN 0161-8105.
- Blagrove, Mark; Farmer, Laura; Williams, Elvira (2004). "The relationship of nightmare frequency and nightmare distress to well-being". Journal of Sleep Research. 13 (2): 129–136. doi:10.1111/j.1365-2869.2004.00394.x. ISSN 1365-2869.
- "Nightmare Disorder". The Gale Encyclopedia of Mental Health. January 1, 2008. Archived from the original on May 29, 2016. Retrieved April 14, 2016.
Because stress is thought to be the most common cause of nightmares, stress reduction techniques may prove to be effective complementary treatments. Typical relaxation techniques such as yoga, meditation or exercise may be helpful.
– via HighBeam (subscription required) - Murray A. Raskind, Elaine R. Peskind, Evan D. Kanter, (February 2003). Reduction of Nightmares and Other PTSD Symptoms in Combat Veterans by Prazosin: A Placebo-Controlled Study, American Journal of Psychiatry, (160) 371-373.
- "Drug Helps PTSD Nightmares" (Press release). Department of Veteran Affairs. March 30, 2008. Archived from the original on July 3, 2009. Retrieved 2012-06-23. (Archived page)
- Kartje, Rebecca; Zak, Rochelle; Ramar, Kannan; Maganti, Rama; Kristo, David; Casey, Kenneth R.; Auerbach, Sanford; Morgenthaler, Timothy I. (2018-06-15). "Position Paper for the Treatment of Nightmare Disorder in Adults: An American Academy of Sleep Medicine Position Paper". Journal of Clinical Sleep Medicine. 14 (6): 1041–1055. doi:10.5664/jcsm.7178. ISSN 1550-9389. PMC 5991964. PMID 29852917.
- Morgenthaler, T. I., Auerbach, S., Casey, K. R., Kristo, D., Maganti, R., Ramar, K., ... & Kartje, R. (2018). Position paper for the treatment of nightmare disorder in adults: an American Academy of Sleep Medicine position paper. Journal of Clinical Sleep Medicine, 14(06), 1041-1055.
- Silver, S. M., Brooks, A., & Obenchain, J. (1995). Treatment of Vietnam War veterans with PTSD: A comparison of eye movement desensitization and reprocessing, biofeedback, and relaxation training. Journal of Traumatic Stress, 8(2), 337–342.
- Jayatunge, R. M. (2008). Combating Tsunami Disaster Through EMDR. Journal of EMDR Practice and Research, 2(2), 140‑145. https://doi.org/10.1891/1933-3196.2.2.140
- Greenwald, G. (1993b). Treating children’s nightmares with EMDR. EMDR Network Newsletter, 3 (1), 7–9.
- Spoormaker, Victor I.; van den Bout, Jan (October 2006). "Lucid Dreaming Treatment for Nightmares: A Pilot Study" (PDF). Psychotherapy and Psychosomatics. 75 (6): 389–394. doi:10.1159/000095446. PMID 17053341.
Conclusions: LDT seems effective in reducing nightmare frequency, although the primary therapeutic component (i.e. exposure, mastery, or lucidity) remains unclear.
- Colic, M. (2007). "Kanna's lucid dreams and the use of narrative practices to explore their meaning." The International Journal of Narrative Therapy and Community Work (4): 19–26.
- Zadra, A. L., & Pihl, R. O. (1997). Lucid Dreaming as a Treatment for Recurrent Nightmares. Psychotherapy and Psychosomatics, 66(1), 50‑55. https://doi.org/10.1159/000289106
- Bout, Jan van den; Spoormaker, Victor I. (2006). "Lucid Dreaming Treatment for Nightmares: A Pilot Study". Psychotherapy and Psychosomatics. 75 (6): 389–394. doi:10.1159/000095446. ISSN 0033-3190. PMID 17053341.
- R. Nisha Aurora.; et al. (2010). "Best Practice Guide for the Treatment of Nightmare Disorder in Adults" (PDF). Journal of Clinical Sleep Medicine. 6 (4): 549–553.
- Lynch, John; Leszczyszyn, David J.; Vrana, Scott R.; Rybarczyk, Bruce; Margolies, Skye Ochsner (2013-10-01). "Efficacy of a Cognitive‐Behavioral Treatment for Insomnia and Nightmares in Afghanistan and Iraq Veterans With PTSD". Journal of Clinical Psychology. 69 (10): 1026–1042. doi:10.1002/jclp.21970. ISSN 1097-4679.
- "CBT for Insomnia: Techniques & Case Study - National Sleep Foundation". www.sleepfoundation.org. Retrieved 2019-06-17.
- Salzarulo, P.; Chevalier, A. (September 1983). "Sleep Problems in Children and Their Relationship with Early Disturbances of the Waking-Sleeping Rhythms". Sleep. 6 (1): 47–51. doi:10.1093/sleep/6.1.47. ISSN 0161-8105.
- Agargun, MY; Kara, H; Ozer, OA; Selvi, Y; Kiran, U; Ozer, B (December 2003). "Clinical importance of nightmare disorder in patients with dissociative disorders". Psychiatry and Clinical Neurosciences. 57 (6): 575–9. doi:10.1046/j.1440-1819.2003.01169.x. PMID 14629705.
- Semiz, UB; Basoglu, C; Ebrinc, S; Cetin, M (February 2008). "Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder". Psychiatry and Clinical Neurosciences. 62 (1): 48–55. doi:10.1111/j.1440-1819.2007.01789.x. PMID 18289141.
- Kennedy, G. (2002, November). A review of hypnosis in the treatment of parasomnias: Nightmare, sleepwalking, and sleep terror disorders. Australian Journal of Clinical & Experimental Hypnosis, 30(2), 99-155.
- Agargun, MY; Gulec, M; Cilli, AS; Kara, H; Sekeroglu, R; Dulger, H; Besiroglu, L; Inci, R (May 2005). "Nightmares and serum cholesterol level: a preliminary report". Canadian Journal of Psychiatry. 50 (6): 361–4. doi:10.1177/070674370505000613. PMID 15999954.