National Health Service
Each of the four separate and independent public healthcare providers in the United Kingdom are collectively the National Health Service (NHS). It includes the National Health Service in England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland. They were established together in 1948 as one of the major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery.[1] Each service provides a comprehensive range of health services, free at the point of use for people ordinarily resident in the United Kingdom, apart from dental treatment and optical care.[2] The English NHS also requires patients to pay prescription charges with a range of exemptions from these charges.
Each of the UK's health service systems operates independently, and is politically accountable to the relevant government: the Scottish Government, Welsh Government, Northern Ireland Executive, and the UK Government, responsible for England's NHS. Since 2013 operational responsibility for the NHS in England has been passed to NHS England.[3] NHS Wales was originally part of the same structure as that of England until powers over the NHS in Wales were first transferred to the Secretary of State for Wales in 1969 and thereafter, in 1999, to the Welsh Assembly as part of Welsh devolution. Some functions may be routinely performed by one health service on behalf of another. For example, Northern Ireland has no high-security psychiatric hospitals and depends on hospitals in Great Britain, routinely at Carstairs hospital in Scotland for male patients and Rampton Secure Hospital in England for female patients.[4] Similarly, patients in North Wales use specialist facilities in Manchester and Liverpool which are much closer than facilities in Cardiff, and more routine services at the Countess of Chester Hospital. There have been issues about cross-border payments.[5]
Taken together, the four National Health Services in 2015–16 employed around 1.6 million people with a combined budget of £136.7 billion.[6] In 2014 the total health sector workforce across the UK was 2,165,043. This broke down into 1,789,586 in England, 198,368 in Scotland, 110,292 in Wales and 66,797 in Northern Ireland.[7] In 2017, there were 691,000 nurses registered in the UK, down 1,783 from the previous year. However, this is the first time nursing numbers have fallen since 2008. Every 24 hours it sees one million patients, and with 1.7 million staff it is the fifth biggest employer in the world.[8]
Although there has been increasing policy divergence between the four National Health Services in the UK, it can be difficult to find evidence of the effect of this on performance since, as Nick Timmins says: "Some of the key data needed to compare performance – including data on waiting times – is defined and collected differently in the four countries."[9][10] Statistics released in December 2017 showed that, compared with 2012/3, 9% fewer patients in Scotland were waiting more than four hours in accident and emergency, whereas in England the number had increased by 155%.[11] However, since then Scotland in common with the other three UK countries has experienced increasing pressure in Scottish Accident and Emergency departments with deteriorating waiting times.[12][13][14]
When purchasing drugs, the NHS has significant market power that, based on its own assessment of the fair value of the drugs, influences the global price, typically keeping prices lower.[15] Several other countries either copy the U.K.'s model or directly rely on Britain’s assessments for their own decisions on state-financed drug reimbursements.[16]
History
Dr Somerville Hastings, President of the Socialist Medical Association, successfully proposed a resolution at the 1934 Labour Party Conference that the party should be committed to the establishment of a State Health Service.[18]
Conservative MP and Health Minister, Henry Willink, first proposed the National Health Service in 1944 with the publication of a White Paper "A National Health Service" which was widely distributed in full and short versions as well as in newsreel by Henry Willink himself.[19] Aneurin Bevan's National Health Service became Westminster legislation for England and Wales from 1946 and Scotland from 1947, and the Northern Ireland Parliament's Public Health Services Act 1947.[20] NHS Wales was split from NHS (England) in 1969 when control was passed to the Secretary of State for Wales before transferring to the Welsh Executive and Assembly under devolution in 1999.[21]
Calls for a "unified medical service" can be dated back to the Minority Report of the Royal Commission on the Poor Law in 1909,[22] but it was following the 1942 Beveridge Report's recommendation to create "comprehensive health and rehabilitation services for prevention and cure of disease" that cross-party consensus emerged on introducing a National Health Service of some description.[23] When Clement Attlee's Labour Party won the 1945 election he appointed Aneurin Bevan as Health Minister. Bevan then embarked upon what the official historian of the NHS, Charles Webster, called an "audacious campaign" to take charge of the form the NHS finally took.[24]
The NHS was born out of the ideal that good healthcare should be available to all, regardless of wealth. Although being freely accessible regardless of wealth maintained Henry Willink's principle of free healthcare for all, Conservative MPs were in favour of maintaining local administration of the NHS through existing arrangements with local authorities fearing that an NHS which owned hospitals on a national scale would lose the personal relationship between doctor and patient.[25]
Conservative MPs voted in favour of their amendment to Bevan's Bill to maintain local control and ownership of hospitals and against Bevan's plan for national ownership of all hospitals. The Labour government defeated Conservative amendments and went ahead with the NHS as it remains today; a single large national organisation (with devolved equivalents) which forced the transfer of ownership of hospitals from local authorities and charities to the new NHS. Bevan's principle of ownership with no private sector involvement has since been diluted, with later Labour governments implementing large scale financing arrangements with private builders in private finance initiatives and joint ventures.[26]
At its launch by Bevan on 5 July 1948 it had at its heart three core principles: That it meet the needs of everyone, that it be free at the point of delivery, and that it be based on clinical need, not ability to pay.[27]
Three years after the founding of the NHS, Bevan resigned from the Labour government in opposition to the introduction of charges for the provision of dentures and glasses.[28] The following year, Winston Churchill's Conservative government introduced prescription charges. These charges were the first of many controversies over reforms to the NHS throughout its history.[29]
From its earliest days, the cultural history of the NHS has shown its place in British society reflected and debated in film, TV, cartoons and literature. The NHS had a prominent slot during the 2012 London Summer Olympics opening ceremony directed by Danny Boyle, being described as "the institution which more than any other unites our nation".[30]
Eligibility for treatment
UK residents are not charged for most medical treatment, though NHS dentistry does have standard charges in each of the four national health services in the UK. In addition, most patients in England have to pay charges for prescriptions though some are exempted.
Aneurin Bevan in considering the provision of NHS services to overseas visitors wrote, in 1952, that it would be "unwise as well as mean to withhold the free service from the visitor to Britain. How do we distinguish a visitor from anybody else? Are British citizens to carry means of identification everywhere to prove that they are not visitors? For if the sheep are to be separated from the goats both must be classified. What began as an attempt to keep the Health Service for ourselves would end by being a nuisance to everybody." [31]
The provision of free treatment to non-UK-residents, formerly interpreted liberally, has been increasingly restricted, with new overseas visitor hospital charging regulations introduced in 2015.[32]
Citizens of the EU holding a valid European Health Insurance Card and persons from certain other countries with which the UK has reciprocal arrangements concerning health care can get emergency treatment without charge.[33]
The NHS is free at the point of use, for general practitioner (GP) and emergency treatment not including admission to hospital, to non-residents.[34] People with the right to medical care in European Economic Area (EEA) nations are also entitled to free treatment by using the European Health Insurance Card. Those from other countries with which the UK has reciprocal arrangements also qualify for free treatment.[35][36] Since 6 April 2015, non-EEA nationals who are subject to immigration control must have the immigration status of indefinite leave to remain at the time of treatment and be properly settled, to be considered ordinarily resident. People not ordinarily resident in the UK are in general not entitled to free hospital treatment, with some exceptions such as refugees.[2][37]
People not ordinarily resident may be subject to an interview to establish their eligibility, which must be resolved before non-emergency treatment can commence. Patients who do not qualify for free treatment are asked to pay in advance or to sign a written undertaking to pay, except for emergency treatment.
People from outside the EEA coming to the UK for a temporary stay of more than six months are required to pay an immigration health surcharge at the time of visa application, and will then be entitled to NHS treatment on the same basis as a resident. This includes overseas students with a visa to study at a recognised institution for 6 months or more, but not visitors on a tourist visa.[38] In 2016 the surcharge was £200 per year, with exemptions and reductions in some cases.[39] It is to increase to £400 in 2018. The discounted rate for students and those on the Youth Mobility Scheme will increase from £150 to £300.[40]
From 15 January 2007, anyone who is working outside the UK as a missionary for an organisation with its principal place of business in the UK is fully exempt from NHS charges for services that would normally be provided free of charge to those resident in the UK. This is regardless of whether they derive a salary or wage from the organisation, or receive any type of funding or assistance from the organisation for the purposes of working overseas.[41] This is in recognition of the fact that most missionaries would be unable to afford private health care and those working in developing countries should not effectively be penalised for their contribution to development and other work.
Those who are not ordinarily resident (including British citizens who may have paid National Insurance contributions in the past) are liable to charges for services.
There are some other categories of people who are exempt from the residence requirements such as specific government workers and those in the armed forces stationed overseas.
See also Immigration health surcharge.
Current issues
While under pressure in recent years as a result of economic austerity according to Unite,[42] public satisfaction with the NHS has increased from 38% in 2001 to 53% in 2018.[43] Public satisfaction with NHS care is more than twice as high as for local authority-funded social care, which stands at 26%. Furthermore, the NHS is consistently ranked as the institution that makes people proudest to be British, beating the Royal family, Armed Forces and the BBC.[44] NHS staff - particularly nurses and doctors - are the most trusted professions in Britain.[45]
Funding
The systems are 98.8% funded from general taxation and National Insurance contributions, plus small amounts from patient charges for some services.[47][48] About 10% of GDP is spent on health and most is spent in the public sector.[49] The money to pay for the NHS comes directly from taxation. The 2008/9 budget roughly equates to a contribution of £1,980 per person in the UK.[50]
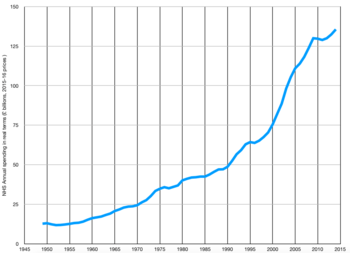
When the NHS was launched in 1948 it had a budget of £437 million (roughly £9 billion at today’s prices).[51] In 2016–17 it was £122.5 billion.[52] In 1955/6 health spending was 11.2% of the public services budget. In 2015/16 it was 29.7%.[53] This equates to an average rise in spending over the full 60-year period of about 4% a year once inflation has been taken into account. Under the Blair government spending levels increased by around 6% a year on average. Since 2010 spending growth has been constrained to just over 1% a year.[53] Many minor procedures may no longer be available from 2019 and the real reason may be to cut costs.[54]
Some 60% of the NHS budget is used to pay staff. A further 20% pays for drugs and other supplies, with the remaining 20% split between buildings, equipment, training costs, medical equipment, catering and cleaning. Nearly 80% of the total budget is distributed by local trusts in line with the particular health priorities in their areas.[55] Since 2010, there has been a cap of 1% on pay rises for staff continuing in the same role. Unions representing doctors, dentists, nurses and other health professionals have called on the government to end the cap on health service pay, claiming the cap is damaging the health service and damaging patient care.[56] The pay rise is likely to be below the level of inflation and to mean a real-terms pay cut.[57] The House of Commons Library did research showing that real-terms NHS funding per head will fall in 2018–19, and stay the same for two years afterwards.[58]
There appears to be support for higher taxation to pay for extra spending on the NHS as an opinion poll in 2016 showed that 70% of people were willing to pay an extra penny in the pound in income tax if the money were ringfenced and guaranteed for the NHS.[59] Two thirds of respondents to a King's Fund poll favour increased taxation to help finance the NHS.[60]
The Guardian has said that GPs face excessive workloads throughout Britain and that this puts the GP's health and that of their patients at risk.[61] The Royal College of Physicians did a survey of doctors in England, Wales, Scotland and Northern Ireland. Two-thirds of doctors surveyed maintained patient safety had deteriorated during the year to 2018, 80% feared they would be unable to provide safe patient care in the coming year while 84% felt increased pressure on the NHS was demoralising the workforce. Jane Dacre said, “We simply cannot go through this [a winter when the NHS is badly overstretched] again. It is not as if the situation was either new or unexpected. As the NHS reaches 70, our patients deserve better. Somehow, we need to move faster towards a better resourced, adequately staffed NHS during 2018 or it will happen again.”[62] At a time when the NHS is short of doctors foreign doctors are forced to leave the UK due to visa restrictions.[63] A study found that a fifth of doctors had faced bullying from seniors in the previous year due to pressure at work.[64]
The NHS is underresourced compared to health provisions in other developed nations. A King’s Fund study of OECD data from 21 nations, revealed that the NHS has among the lowest numbers of doctors, nurses and hospital beds per capita in the western world.[65] Nurses within the NHS maintain that patient care is compromised by the shortage of nurses and the lack of experienced nurses with the necessary qualifications.[66] According to a YouGov poll, 74 percent of the UK public believes there are too few nurses.[67] The NHS performs below average in preventing deaths from cancer, strokes and heart disease.[68] Staff shortages at histology departments are delaying diagnosis and start of treatment for cancer patients.[69] In England and Scotland cancer wards and children's wards have to close because the hospital cannot attract sufficient qualified doctors and nurses to run the wards safely. Cancer patients and child patients are having to travel very long distances to get treatment and their relatives must travel far to visit the patients. In wards which have not closed staff sometimes work under stress due to staff shortages. Brexit is likely to aggravate these problems.[70] Due to the shortage of nurses the NHS is relying on less qualified staff like healthcare assistants and nursing associates.[71]
Cancer survival rates in the UK have been rising fast but probably still lag behind the best results internationally, mainly because of late diagnosis.[72] However death rates from breast cancer are falling faster in Britain than in any other of the six largest countries in Europe, and are estimated now to have improved beyond the European average.[73][74] According to Breast Cancer Care 72% of NHS trusts across the UK do not provide dedicated specialist nurses for patients with incurable breast cancer."[75][72] Cancer Research UK maintains more NHS cancer personnel are needed to enable the UK to catch up The NHS in England is expanding early diagnosis services with the goal of increasing the proportion of cancers diagnosed early (at stages 1 and 2) from 53% to 75% in the decade to 2028.[76] The NHS was the first health service in Europe to negotiate coverage for novel CAR-T cancer therapy, with agreement reached within 10 days of its European marketing authorisation.[77]
Staffing
.svg.png)
The plan to exit the European Union will affect physicians from EU countries, about 11% of the physician workforce.[79] Many of these physicians are considering leaving the UK if Brexit happens, as they have doubts that they and their families can live in the country.[79] A survey suggests 60% are considering leaving.[80] Record numbers of EU nationals (17,197 EU staff working in the NHS which include nurses and doctors) left in 2016. The figures, put together by NHS Digital, led to calls to reassure European workers over their future in the UK.[81]
In June 2018 the Royal College of Physicians calculated that medical training places need to be increased from 7,500 to 15,000 by 2030 to take account of part-time working among other factors. At that time there were 47,800 consultants working in the UK of which 15,700 were physicians. About 20% of consultants work less than full-time.[82]
Performance
A study by the King's Fund, Health Foundation, Nuffield Trust and the Institute for Fiscal Studies to mark the NHS 70th anniversary concluded that the main weakness of the NHS was health care outcomes. Mortality for cancer, heart attacks and stroke, was higher than average among comparable countries. The NHS does well at protecting people from heavy financial costs when they are ill. Waiting times are about the same and the management of longterm illness is better than in other comparable countries. Efficiency is good, with low administrative costs and high use of cheaper generic medicines.[83] Twenty-nine hospital trusts and boards out of 157 have not hit any waiting time target in the year 2017-2018.[84] The Office for National Statistics reported in January 2019 that productivity in the English NHS had been growing at 3%, considerably faster than across the rest of the UK economy.[85]
Over 130,000 deaths since 2012 in the UK could have been prevented if progress in public health policy had not stopped due to austerity, analysis by the Institute for Public Policy Research found. Dean Hochlaf of the IPPR said, “We have seen progress in reducing preventable disease flatline since 2012."[86]
British exit from the European Union
There is also concern that a disorderly Brexit may compromise patients' access to vital medicines. Many medical organisations are diverting resources from patient care to managing a possible worst-case Brexit scenario.[87] Pharmaceutical organisations working with the Civil Service to keep medicine supplies available if there is a no-deal Brexit have signed 26 Non-Disclosure Agreements (NDA's) or, “gagging orders” to prevent them giving the public information. The figures were given on 21 December 2018 after Rushanara Ali asked a parliamentary question. Ali said, “It is utterly unacceptable for the government to use non-disclosure agreements with pharmaceutical businesses and trade associations. By effectively ‘gagging’ these organisations, these secretive agreements are preventing essential information from being shared, are undermining transparency and are hampering businesses’ ability to speak out.”[88]
Rising social care costs
Social care will cost more in future according to research by Liverpool University, University College London, and others and higher investment are needed. Professor Helen Stokes-Lampard of the Royal College of GPs said, “It’s a great testament to medical research, and the NHS, that we are living longer – but we need to ensure that our patients are living longer with a good quality of life. For this to happen we need a properly funded, properly staffed health and social care sector with general practice, hospitals and social care all working together – and all communicating well with each other, in the best interests of delivering safe care to all our patients.”[89]
Mental health
Some patients have to wait excessively long for mental health care. The Royal College of Psychiatrists found some must wait up to thirteen months for the right care. Wendy Burn of the Royal College of Psychiatrists said, “It is a scandal that patients are waiting so long for treatment. The failure to give people with mental illnesses the prompt help they need is ruining their lives.” Even patients who are suicidal or who have attempted suicide are sometimes denied treatment; patients are told they are not ill enough or waiting lists are too long. During very long waits for treatment, one in three patients deteriorate, and they may become unemployed or get divorced. One in four patients throughout the UK wait over three months to see an NHS mental health professional, with 6% waiting at least a year.[90]
The National Audit Office found mental health provisions for children and young people will not meet growing demand, despite promises of increased funding. Even if promises to provide £1.4bn more for the sector are kept, there will be “significant unmet need” due to staff shortages, inadequate data and failure to control spending by NHS clinical commissioning groups. Currently one-quarter of young people needing mental health services can get NHS help. The Department of Health and Social Care hopes to raise the ratio to 35%. Efforts to improve mental health provisions could reveal previously unmet demand.[91]
Meg Hillier of the select committee on public accounts said, “The government currently estimates that less than a third of children and young people with a diagnosable mental health condition are receiving treatment. But the government doesn’t understand how many children and young people are in need of treatment or how funding is being spent locally. The government urgently needs to set out how departments, and national and local bodies, are going to work together to achieve its long-term ambition.” Amyas Morse said, “Current targets to improve care are modest and even if met would still mean two-thirds of those who need help are not seen. Rising estimates of demand may indicate that the government is even further away than it thought.”[91]
In response, NHS England has embarked on a major programme to expand mental health services, whose budgets are now growing faster than the NHS overall.[92] MIND the mental health charity responded saying: "We are pleased that the plan includes a commitment of £2.3bn a year towards mental health, to help redress the balance. The plan promises that this money will see around two million more people with anxiety, depression and other mental health problems receive help, including new parents, and 24 hour access to crisis care. The plan also includes a guarantee that investment in primary, community and mental health care will grow faster than the growing overall NHS budget so that different parts of the NHS come together to provide better, joined-up care in partnership with local government. Since the funding announcement in the summer, Mind has been working with the NHS, Government and voluntary sector to help shape the long term plan. This longer-term strategy was developed in consultation with people with mental health problems to ensure their views are reflected."[92]
Surgery
Waiting times for routine surgery have fallen substantially since 2000. As of July 2019, the median wait for planned care in England is under 8 weeks. The number of people waiting over 12 months has fallen from over 200,000 in the 1980s to under 2000 in 2019.[93] However the number of patients on the waiting list has risen recently as constrained funding, hospital beds and staffing growth has not kept up with increasing patient need.[94]
2018 funding increase
In 2018, British Prime Minister Theresa May announced that NHS in England would receive a 3.4% increase in funding every year to 2024, which would allow it to receive an extra £20bn a year in real terms funding.[95] There is concern that a high proportion of this money will go to service NHS debts rather than for improved patient care. There are calls for the government to write off the NHS debt. Saffron Cordery of NHS Providers said that hospitals needed help to do their work without being up in deficit, as two-thirds were in the year to 2018.[96] Some expressed doubt over whether May could carry out this proposed increase in funding.[97] The next day, Health Secretary Jeremy Hunt backed the extra £20bn annual increase in NHS funding and responded to criticism by stating that taxation would be used to carry out the funding and that details would be revealed when the next budget is unveiled in November.[95][98]
The Institute for Fiscal Studies has stated a 5% real-terms increase was needed for real change. Paul Johnson of the IFS said the 3.4% was greater than recent increases, but less than the long-term average.[99] Health experts maintain the money will "help stem further decline in the health service, but it's simply not enough to address the fundamental challenges facing the NHS, or fund essential improvements to services that are flagging."[100] Inflation may erode the real value of this funding increase.[101]
As part of the 2018 funding increase the government asked the NHS to produce a 10-year plan as to how this funding would be used. On 7 January 2019, the NHS England published the NHS Long Term Plan.
Electronic systems
21 different electronic systems are used in the NHS to record data on patients. These systems do not communicate well with each other so there is a risk doctors treating a patient will not know everything they need to know to treat the patient effectively. There were 11 million patient interactions out of 121 million where information from a previous visit could not be accessed. Half the Trusts using Electronic Medical Records used one of three systems and at least those three should be able to share information. A tenth of Trusts used multiple systems in the same hospital. Dr Leigh Warren who participated in the research said, "Hospitals and GPs often don't have the right information about the right patient in the right place at the right time. This can lead to errors and accidents that can threaten patients' lives."[102]
Sale of data
Information on millions of NHS patients was sold to international pharmaceutical companies, in the US and other nations for research, adding to concerns over USA ambitions to access remunerative parts of the NHS after Brexit. There is concern over lack of transparency and clarity over the data and how it is used. Phil Booth of medConfidential, campaigning for privacy of health data said, “Patients should know how their data is used. There should be no surprises. While legitimate research for public health benefit is to be encouraged, it must always be consensual, safe and properly transparent. Do patients know – have they even been told by the one in seven GP practices across England that pass on their clinical details – that their medical histories are being sold to multinational pharma companies in the US and around the world?”[103]
Medicines
In November 2019 unprecedented shortages of medicines patients need developed. Drugs to treat cancer, heart disease Parkinson's disease, mental health conditions, some eye conditions, antibiotics for tuberculosis and drugs to control epilepsy are among those in short supply. Life saving drugs will have to be rationed and not all patients who need them will get them. Some patients can be switched onto other drugs, though this may increase the workload of hard-pressed medical staff; other patients cannot be switched to alternative drugs. Many problems can impact the supply chain, like IT failure, speculators stockpiling drugs, alterations in regulation and sudden disease outbreaks. Dr Tony O’Sullivan of Keep Our NHS Public said, “The Health Department’s guidance includes an unprecedented list of drugs unavailable or in short supply. Patients and clinicians alike should be on high alert when the advice includes how to ‘share stocks’ to make them last, to ‘prioritise’ patients already on specific treatments including cancer rather than a new patient and effectively how to ration so many vital drugs. Drug companies’ behaviour must be controlled. We must urgently protect the NHS from further risks of loss of control of drug prices and supplies from trade deals with the USA and that requires returning it to a wholly public service.”[104][105]
References
- Choices, NHS. "The principles and values of the NHS in England". www.nhs.uk. Retrieved 23 November 2016.
- "NHS entitlements: migrant health guide – Detailed guidance". UK Government. Retrieved 6 June 2016.
- Timmins, Nicholas (24 May 2018). "The first five years of NHS England" (PDF). Institute for Government and The Kings Fund.
- "Guidance on the Transfer of Mentally Disordered Patients August 2011".
- "Breakdown of cross-border agreements is costing English trusts millions". Health Service Journal. 14 February 2008. Retrieved 19 January 2016.
- "10 truths about Britain's health service". Guardian. 18 January 2016. Retrieved 19 January 2016.
- Cowper, Andy (23 May 2016). "Visible and valued: the way forward for the NHS's hidden army". Health Service Journal. Retrieved 28 July 2016.
- Triggle, Nick (24 May 2018). "10 charts that show why the NHS is in trouble". Retrieved 6 October 2019.
- "Outcomes in EHCI 2015" (PDF). Health Consumer Powerhouse. 26 January 2016. Archived from the original (PDF) on 6 June 2017. Retrieved 27 January 2016.
- Timmins, Nick (13 June 2013). "The four UK health systems: Learning from each other". Kings Fund. Retrieved 2 February 2016.
- "Scottish A&E bucks trend on long waits". BBC. 7 December 2017. Retrieved 10 December 2017.
- "STV".
- "The Scotsman". 7 May 2009.
- "The Scotsman". 21 August 2019.
- "The UK has much to fear from a US trade agreement". www.newstatesman.com. Retrieved 5 June 2019.
- "US takes aim at the UK's National Health Service". POLITICO. 4 June 2019. Retrieved 5 June 2019.
- Thomas-Symonds, Nick (3 July 2018). "70 years of the NHS: How Aneurin Bevan created our beloved health service". The Independent. Retrieved 5 July 2018.
- "Health Service debate". Labour Party. October 1934. Retrieved 30 June 2018.
- White Paper – A National Health Service, YouTube
- Ruth Barrington, Health, Medicine & Politics in Ireland 1900–1970 (Institute of Public Administration: Dublin, 1987) pp. 188–89.
- Wales, NHS (23 October 2006). "NHS Wales | 1960's". www.wales.nhs.uk. Retrieved 22 November 2016.
- Brian Abel-Smith, The Hospitals 1800–1948 (London, 1964), p.229
- Beveridge, William (November 1942). "Social Insurance and Allied Services" (PDF). HM Stationery Office. Retrieved 3 March 2013.
- Charles Webster, The Health Services since the War, Volume 1: Problems of Health Care, The National Health Service Before 1957 (London: HMSO, 1988), p. 399.
- "NHS Bill Second Reading". Hansard. 30 April 1946.
- "Kingsfund, July 2013".
- "The NHS in England – About the NHS – NHS core principles". Nhs.uk. 23 March 2009. Retrieved 27 June 2017.
- Kenneth O. Morgan, 'Aneurin Bevan' in Kevin Jeffreys (ed.), Labour Forces: From Ernie Bevin to Gordon Brown (I.B. Taurus: London & New York, 2002), pp. 91–92.
- Martin Powell and Robin Miller, 'Seventy Years of Privatising the British National Health Service?', Social Policy & Administration, vol. 50, no. 1 (January 2016), pp. 99–118.
- Adams, Ryan (27 July 2012). "Danny Boyle's intro on Olympics programme". Awards Daily. Retrieved 27 November 2016.
- Bevan, Aneurin (1952). In Place of Fear. Retrieved 2 April 2018.
- "Guidance on overseas visitors hospital charging regulations". UK Government. 6 April 2016. Retrieved 6 June 2016. Links to many relevant documents: Guidance on implementing the overseas visitor hospital charging regulations 2015; Ways in which people can be lawfully resident in the UK; Summary of changes made to the way the NHS charges overseas visitors for NHS hospital care; Biometric residence permits: overseas applicant and sponsor information; Information sharing with the Home Office: guidance for overseas patients; Overseas chargeable patients, NHS debt and immigration rules: guidance on administration and data sharing; Ordinary residence tool; and documents on Equality analysis.
- Nardelli, Alberto (11 August 2015). "Are foreigners really gaming the NHS to pay for their medical treatment abroad?". the Guardian.
- "Visiting or moving to England? – How to access NHS services (see "Hospital Services" section)". NHS Choices. 26 June 2015. Retrieved 6 June 2016.
- "NHS charges for people from abroad". Citizens Advice. Retrieved 16 November 2010.
- "Non-EEA country-by-country guide – Healthcare abroad". NHS Choices. 1 January 2016. Retrieved 6 June 2016.
- "Categories of exemption – Healthcare in England for visitors – NHS Choices". NHS England. 18 August 2015. Retrieved 6 June 2016.
- Bruno Rodrigues, "Important NHS charges in visa applications", "Immigration Media", 18 March 2015
- NHS Choices (18 August 2015). "Moving from outside the EEA – Access to healthcare in England". Nhs.uk. Retrieved 6 June 2016.
- "Increase in health charge paid by temporary migrants". OnMedica. 6 February 2018. Retrieved 2 April 2018.
- National Health Service (Charges to Overseas Visitors) Regulations 1989
- NHS public satisfaction dip due to government austerity policies, says Unite
- "Public satisfaction with the NHS and social care in 2018". The King's Fund. 7 March 2019. Retrieved 30 September 2019.
- Team, Mintel Press. "The NHS tops list of UK's most cherished institutions". Mintel. Retrieved 30 September 2019.
- "Advertising execs rank below politicians as Britain's least-trusted profession". Ipsos MORI. Retrieved 30 September 2019.
- "Health spending -". www.ifs.org.uk.
- "How the NHS is funded". TheKing'sFund. 15 January 2016. Retrieved 6 June 2016.
- "Underfunded, underdoctored, overstretched: The NHS in 2016". 21 September 2016.
- "Health care spending compared to other countries". 20 January 2016.
- NHS Choices The NHS in England: The NHS: About the NHS: Overview. Retrieved 22 June 2010.
- "The NHS in England". NHS choices. 28 January 2013. Retrieved 27 July 2014.
- Burch, Patrick (19 December 2018). "Funding in primary care". InnovAiT: Education and Inspiration for General Practice. 12 (2): 100–104. doi:10.1177/1755738018805186.
- "10 charts that show why the NHS is in trouble". BBC News. 8 February 2017. Retrieved 10 February 2017.
- "'Here's a step-by-step guide to saving the NHS, starting with amateur surgery at home'". July 2018.
- https://portal.rcem.ac.uk/LIVE/docs/International/6.5.2%20Part-2---The-structure-and-funding-of-the-NHS.pdf%5B%5D
- Health unions urge Theresa May to ditch NHS pay cap The Guardian
- NHS staff suffer pay cuts in real terms as salaries rise by one per cent The Independent
- Conservatives will break NHS funding pledge, Labour claims The Guardian
- editor, Rowena Mason Deputy political (30 December 2016). "People may be ready to pay extra penny on tax for NHS, Tim Farron says". The Guardian.
- Two-thirds support higher taxes to maintain NHS funding The Observer
- Family doctors working 'beyond safe levels', says GPs' leader The Guardian
- Patient safety getting worse, say two-thirds of NHS doctors The Guardian
- Doctors told to leave UK after Home Office refuses to issue them visas The Independent
- A fifth of NHS doctors were bullied or abused last year, study finds The Guardian
- Shock figures from top thinktank reveal extent of NHS crisis The Observer
- Danger to patients revealed in reports by 18,000 NHS nurses The Observer
- 'Three-quarters of public worried about nurse staffing' BBC
- NHS no longer the envy of the world, says independent report BBC
- Pathologists shortage 'delaying cancer diagnosis' BBC
- UK cancer and children’s wards being hit by closures The Guardian
- Nursing shortages forcing NHS to rely on less qualified staff – report The Guardian
- Cancer survival in the UK improving, but lagging behind - study BBC
- Malvezzi, M; et al. (19 March 2019). "European cancer mortality predictions for the year 2019 with focus on breast cancer". Annals of Oncology. 30 (5, May 2019): 781–787. doi:10.1093/annonc/mdz051. PMID 30887043. Explicit use of et al. in:
|last=(help) - Campbell, Denis (19 March 2019). "UK breast cancer death rates falling fastest in 'big six' of Europe". The Guardian.
- Terminal breast cancer patients 'abandoned' in nurse shortage BBC
- UK still behind in cancer survival despite recent surge The Guardian
- "Children with 'no other hope' to receive groundbreaking cancer treatment on NHS after funding deal". The Independent. 5 September 2018. Retrieved 30 September 2019.
- Aguilar, Carmen (29 May 2018). "Brexit causes flight of European health workers from the NHS". VoxEurop/EDJNet. Retrieved 30 August 2018.
- mamk (23 February 2017). "Brexit gelungenn, Patient tot". Spiegel Online (in German). Der Spiegel. Retrieved 23 February 2017.
- O'Carroll, Lisa; Campbell, Denis (28 February 2017). "Poll shows 60% of European doctors are considering leaving UK". The Guardian.
- Marsh, Sarah; Duncan, Pamela (30 March 2017). "Record number of EU citizens quit working in NHS last year". The Guardian.
- "Medical school places must double by 2030 to meet demand for doctors, college warns". GP Online. 25 June 2018. Retrieved 27 June 2018.
- "How good is the NHS?" (PDF). Kings Fund. July 2018. Retrieved 8 September 2018.
- The hospitals that fail to treat patients on time BBC
- "Public service productivity: healthcare, England: financial year ending 2017". 9 January 2019.
- Austerity to blame for 130,000 ‘preventable’ UK deaths – report The Guardian
- Brexit deal delay could put NHS patients at risk, Tory MP warns The Guardian
- Pharmaceutical firms preparing no-deal Brexit ordered to sign NDAs The Guardian
- NHS faces staggering increase in cost of elderly care, academics warn The Guardian
- Delays in NHS mental health treatment 'ruining lives' The Guardian
- Child mental health services will not meet demand, NAO warns The Guardian
- "Mind responds to NHS long term plan". www.mind.org.uk. Retrieved 30 September 2019.
- "Statistics » Consultant-led Referral to Treatment Waiting Times". www.england.nhs.uk. Retrieved 30 September 2019.
- NHS cancels 14% of operations at last minute, research finds The Guardian
- "Taxes and 'Brexit dividend' to fund NHS cash boost".
- NHS £20bn boost risks being spent to pay off debts, experts warn The Observer
- Walker, Peter (17 June 2018). "May's NHS 'Brexit dividend' claim draws scepticism and doubt". the Guardian.
- "NHS spending boost will increase burden of taxation, says Jeremy Hunt". jerseyeveningpost.com.
- May's NHS 'Brexit dividend' claim draws scepticism and doubt The Guardian
- "Spending on the NHS in England".
- NHS facing huge shortfall without Treasury injection The Observer
- NHS e-health systems 'risk patient safety' BBC
- Patient data from GP surgeries sold to US companies The Observer
- Revealed: NHS running short of dozens of lifesaving medicines The Guardian
- Britain's 'unprecedented' drug shortage BBC
Further reading
- Brady, Robert A. Crisis in Britain. Plans and Achievements of the Labour Government (1950) pp. 352–41 excerpt
- Gorsky, Martin. "The British National Health Service 1948–2008: A Review of the Historiography," Social History of Medicine, Dec 2008, Vol. 21 Issue 3, pp. 437–60
- Hacker, Jacob S. "The Historical Logic of National Health Insurance: Structure and Sequence in the Development of British, Canadian, and U.S. Medical Policy," Studies in American Political Development, April 1998, Vol. 12 Issue 1, pp. 57–130.
- Hilton, Claire. (26 August 2016). Whistle-blowing in the National Health Service since the 1960s History and Policy. Retrieved 11 May 2017.
- Loudon, Irvine, John Horder and Charles Webster. General Practice under the National Health Service 1948–1997 (1998) online
- Rintala, Marvin. Creating the National Health Service: Aneurin Bevan and the Medical Lords (2003) online.
- Rivett G C From Cradle to Grave – the first 50 (65) years of the NHS. King's Fund, London, 1998 now updated to 2014 and available at www.nhshistory.co.uk
- Stewart, John. "The Political Economy of the British National Health Service, 1945–1975: Opportunities and Constraints," Medical History, Oct 2008, Vol. 52 Issue 4, pp. 453–70
- Webster, Charles. "Conflict and Consensus: Explaining the British Health Service," Twentieth Century British History, April 1990, Vol. 1 Issue 2, pp. 115–51
- Webster, Charles. Health Services since the War. 'Vol. 1:' Problems of Health Care. The National Health Service before 1957 (1988) 479pp online
External links
| Wikimedia Commons has media related to National Health Service. |