Mold health issues
Mold health issues are potentially harmful effects of molds (US usage; British English "moulds").
Molds are ubiquitous in the biosphere, and mold spores are a common component of household and workplace dust. The vast majority of molds are not hazardous to humans, and reaction to molds can vary between individuals with relatively minor allergic reactions being the most common.[1] Nonetheless, the United States Centers for Disease Control and Prevention (CDC) reported in its June 2006 report, 'Mold Prevention Strategies and Possible Health Effects in the Aftermath of Hurricanes and Major Floods,' that "excessive exposure to mold-contaminated materials can cause adverse health effects in susceptible persons regardless of the type of mold or the extent of contamination."[2] When mold spores are present in abnormally high quantities, they can present especially hazardous health risks to humans after prolonged exposure, including allergic reactions or poisoning by mycotoxins,[3] or causing fungal infection (mycosis).[4]
Health effects
Studies have shown that people who are atopic (sensitive), already suffer from allergies, asthma, or compromised immune systems[5] and occupy damp or moldy buildings are at an increased risk of health problems such as inflammatory and toxic responses to mold spores, metabolites and other components.[6] The most common health problem is an allergic reaction. Other problems are respiratory and/or immune system responses including respiratory symptoms, respiratory infections, exacerbation of asthma, and rarely hypersensitivity pneumonitis, allergic alveolitis, chronic rhinosinusitis and allergic fungal sinusitis. Severe reactions are rare but possible. A person's reaction to mold depends on their sensitivity and other health conditions, the amount of mold present, length of exposure and the type of mold or mold products.
Some molds also produce mycotoxins that can pose serious health risks to humans and animals. The term "toxic mold" refers to molds that produce mycotoxins, such as Stachybotrys chartarum, not to all molds.[7] Exposure to high levels of mycotoxins can lead to neurological problems and in some cases death.[8] Prolonged exposure, e.g., daily workplace exposure, can be particularly harmful.
The five most common genera of indoor molds are Cladosporium, Penicillium, Aspergillus, Alternaria and Trichoderma.
Damp environments which allow mold to grow can also produce bacteria and help release volatile organic compounds.
Symptoms of mold exposure
Symptoms of mold exposure can include:[9]
- Nasal and sinus congestion, runny nose
- Respiratory problems, such as wheezing and difficulty breathing, chest tightness
- Cough
- Throat irritation
- Sneezing / Sneezing fits
Health effects linking to asthma
Infants may develop respiratory symptoms as a result of exposure to a specific type of fungal mold, called Penicillium. Signs that an infant may have mold-related respiratory problems include (but are not limited to) a persistent cough and/or wheeze. Increased exposure increases the probability of developing respiratory symptoms during their first year of life. Studies have shown that a correlation exists between the probability of developing asthma and increased exposure to Penicillium. The levels are deemed ‘no mold’ to ‘low level’, from ‘low’ to ‘intermediate’, and from ‘intermediate’ to ‘high’.[10]
Mold exposures have a variety of health effects depending on the person. Some people are more sensitive to mold than others. Exposure to mold can cause a number of health issues such as; throat irritation, nasal stuffiness, eye irritation, cough and wheezing, as well as skin irritation in some cases. Exposure to mold may also cause heightened sensitivity depending on the time and nature of exposure. People at higher risk for mold allergies are people with chronic lung illnesses, and weak immune systems, which can often result in more severe reactions when exposed to mold.[11]
There has been sufficient evidence that damp indoor environments are correlated with upper respiratory tract symptoms such as coughing, and wheezing in people with asthma.[12]
Flood specific mold health effects
Among children and adolescents, the most common health effect post-flooding was lower respiratory tract symptoms though there was a lack of association with measurements of total fungi.[13] Another study found that these respiratory symptoms were positively associated with exposure to water damaged homes, exposure included being inside without participating in clean up.[13] Despite lower respiratory effects among all children, there was a significant difference in health outcomes between children with pre-existing conditions and children without.[13] Children with pre-existing conditions were at greater risk that can likely be attributed to the greater disruption of care in the face of flooding and natural disaster.[13] Health effects in children and adolescents with chronic risk were also found to be at an increased risk of adverse outcomes following a natural disaster including diabetes, asthma, chronic lung disease, allergies, HIV/AIDS, other immune disease, heart defects, cystic fibrosis, depression, seizure disorders, Sickle Cell disease, kidney failure, and liver failure.[14]
Although mold is the primary focus post flooding for residents, the effects of dampness alone must also be considered. According to the Institute of Medicine, there is a significant association between dampness in the home and wheeze, cough, and upper respiratory symptoms.[15] A later analysis determined that 30% to 50% of asthma-related health outcomes are associated with not only mold, but also dampness in buildings.[15] Another health effect associated with dampness and mold is Sick Building Syndrome (SBS), which is defined by manifestations of symptomatic illness as a result of poor indoor air quality and pollutant exposures .[15] Signs of potentially illness-causing buildings include condensation on the windows, high humidity in the bathrooms, a moldy odor, or water leakage.[16]
While there is a proven correlation between mold exposure and the development of upper and lower respiratory syndromes, there are still fewer incidences of negative health effect than one might expect.[17] Barbeau and colleagues suggested that studies do not show a greater impact from mold exposure for a number of reasons: 1) the types of health effects are not severe and are therefore not caught; 2) people whose homes have flooded find alternative housing to prevent exposure; 3) self-selection, the healthier people participated in mold clean-up and were less likely to get sick; 4) exposures were time-limited as result of remediation efforts and; 5) the lack of access to health care post-flooding may result in fewer illnesses being discovered and reported for their association with mold.[17] There are also certain notable scientific limitations in studying the exposure effects of molds on individuals because there are currently no known biomarkers that can prove that a person has been exposed to molds.[18] Thus, it is currently impossible to prove correlation between mold exposure and symptoms.[18]
Mold-associated conditions
Health problems associated with high levels of airborne mold spores include[19] allergic reactions, asthma episodes, irritations of the eye, nose and throat, sinus congestion, and other respiratory problems, although mold spores won't actually cause asthma, just irritate existing conditions. For example, residents of homes with mold are at an elevated risk for both respiratory infections and bronchitis.[20] When mold spores are inhaled by an immunocompromised individual, some mold spores may begin to grow on living tissue,[21] attaching to cells along the respiratory tract and causing further problems.[22][23] Generally, when this occurs, the illness is an epiphenomenon and not the primary pathology. Also, mold may produce mycotoxins, either before or after exposure to humans, potentially causing toxicity.
Fungal infection
A serious health threat from mold exposure for immunocompromised individuals is systemic fungal infection (systemic mycosis). Immunocompromised individuals exposed to high levels of mold, or individuals with chronic exposure may become infected.[24][25] Sinuses and digestive tract infections are most common; lung and skin infections are also possible. Mycotoxins may or may not be produced by the invading mold.
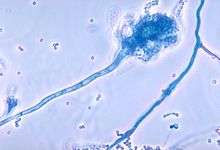
Dermatophytes are the parasitic fungi that cause skin infections such as athlete's foot and tinea cruris. Most dermataphyte fungi take the form of a mold, as opposed to a yeast, with appearance (when cultured) that is similar to other molds.
Opportunistic infection by molds[26] such as Talaromyces marneffei and Aspergillus fumigatus is a common cause of illness and death among immunocompromised people, including people with AIDS or asthma.[27][28]
Mold-induced hypersensitivity
The most common form of hypersensitivity is caused by the direct exposure to inhaled mold spores that can be dead or alive or hyphal fragments which can lead to allergic asthma or allergic rhinitis.[29] The most common effects are rhinorrhea (runny nose), watery eyes, coughing and asthma attacks. Another form of hypersensitivity is hypersensitivity pneumonitis. Exposure can occur at home, at work or in other settings.[29][30] It is predicted that about 5% of people have some airway symptoms due to allergic reactions to molds in their lifetimes.[31]
Hypersensitivity may also be a reaction toward an established fungal infection in allergic bronchopulmonary aspergillosis.
Mycotoxin toxicity
Molds excrete toxic compounds called mycotoxins, secondary metabolites produced by fungi under certain environmental conditions. These environmental conditions affect the production of mycotoxins at the transcription level. Temperature, water activity and pH, strongly influence mycotoxin biosynthesis by increasing the level of transcription within the fungal spore. It has also been found that low levels of fungicides can boost mycotoxin synthesis.[32][33] Certain mycotoxins can be harmful or lethal to humans and animals when exposure is high enough.[34][35]
Extreme exposure to very high levels of mycotoxins can lead to neurological problems and in some cases death; fortunately, such exposures rarely to never occur in normal exposure scenarios, even in residences with serious mold problems.[36] Prolonged exposure, such as daily workplace exposure, can be particularly harmful.[37]
The health hazards produced by mold have been associated with sick building syndrome, but no validated studies have been able to demonstrate that normal indoor exposures to these common organisms pose a significant threat.[38]
It is thought that all molds may produce mycotoxins and thus all molds may be potentially toxic if large enough quantities are ingested, or the human becomes exposed to extreme quantities of mold. Mycotoxins are not produced all the time, but only under specific growing conditions. Mycotoxins are harmful or lethal to humans and animals only when exposure is high enough, as with absolutely all other substances.[39][40]
Mycotoxins can be found on the mold spore and mold fragments, and therefore they can also be found on the substrate upon which the mold grows. Routes of entry for these insults can include ingestion, dermal exposure, and inhalation.
Some mycotoxins cause immune system responses that vary considerably, depending on the individual. The duration of exposure, the frequency of exposure and the concentration of the insult (exposure) are elements in triggering immune system response.
Aflatoxin is an example of a mycotoxin. It is a cancer-causing poison produced by certain fungi in or on foods and feeds, especially in field corn and peanuts.[41]
Originally, toxic effects from mold were thought to be the result of exposure to the mycotoxins of some mold species, such as Stachybotrys chartarum. However, studies are suggesting that the so-called toxic effects are actually the result of chronic activation of the immune system, leading to chronic inflammation.[42][43] Studies indicate that up to 25% of the population has the genetic capability of experiencing chronic inflammation to mold exposure, but it is unknown how many actually experience such symptoms due to frequent misdiagnosis. A 1993–94 case study based on cases of pulmonary hemorrhage in infants in Cleveland, Ohio originally concluded there was causal relationship between the exposure and the disease. The investigators revisited the cases and established that there was no link to the exposure to S. chartrum and the infants in their homes.[44]
The common house mold, Trichoderma longibrachiatum, produces small toxic peptides containing amino acids not found in common proteins, like alpha-aminoisobutyric acid, called trilongins (up to 10% w/w). Their toxicity is due to absorption into cells and production of nano-channels that obstruct vital ion channels that ferry potassium and sodium ions across the cell membrane. This affects in the cells action potential profile, as seen in cardiomyocytes, pneumocytes and neurons leading to conduction defects. Trilongins are highly resistant to heat and antimicrobials making primary prevention the only management option.[45][46][47]
Exposure sources and prevention
The main sources of mold exposure are from the indoor air in buildings with substantial mold growth, and from ingestion of food with mold growths.
Air
Prevention of mold exposure and its ensuing health issues begins with prevention of mold growth in the first place by avoiding a mold-supporting environment such as humid air. Extensive flooding and water damage can support extensive mold growth. Following hurricanes, homes with greater flood damage, especially those with more than 3 feet (0.91 m) of indoor flooding, demonstrated higher levels of mold growth compared with homes with little or no flooding.[48][49] The aftermath of a hurricane is the worst-case scenario, but the concept of water damage supporting widespread mold growth is more generally applicable.
It is useful to perform an assessment of the location and extent of the mold hazard in a structure. Various practices of remediation can be followed to mitigate mold issues in buildings, the most important of which is to reduce moisture levels.[50] Removal of affected materials after the source of moisture has been reduced and/or eliminated may be necessary.[51] Thus, the concept of mold growth, assessment, and remediation is essential in prevention of mold health issues.
A common issue with mold hazards in the household is the placement of furniture, and the lack of ventilation which this causes to certain parts of the wall. The simplest method of avoiding mold in a home so affected is to move the furniture in question.
Adverse respiratory health effects are associated with occupancy in buildings with moisture and mold damage.[52]
Molds may excrete liquids or low-volatility gases, but the concentrations are so low that frequently they cannot be detected even with sensitive analytical sampling techniques. Sometimes these by-products are detectable by odor, in which case they are referred to as "ergonomic odors" meaning the odors are detectable, but do not indicate toxicologically significant exposures.
Food

Molds that are often found on meat and poultry include members of the genera Alternaria, Aspergillus, Botrytis, Cladosporium, Fusarium, Geotrichum, Mortierella, Mucor, Neurospora, Paecilomyces, Penicillium, and Rhizopus.[53] Grain crops in particular incur considerable losses both in field and storage due to pathogens, post-harvest spoilage, and insect damage. A number of common microfungi are important agents of post-harvest spoilage, notably members of the genera Aspergillus, Fusarium, and Penicillium.[53] A number of these produce mycotoxins (soluble, non-volatile toxins produced by a range of microfungi that demonstrate specific and potent toxic properties on human and animal cells[54]) that can render foods unfit for consumption. When ingested, inhaled, or absorbed through skin, mycotoxins may cause or contribute to a range of effects from reduced appetite and general malaise to acute illness or death in rare cases.[55][56][57] Mycotoxins may also contribute to cancer. Dietary exposure to the mycotoxin aflatoxin B1, commonly produced by growth of the fungus Aspergillus flavus on improperly stored ground nuts in many areas of the developing world, is known to independently (and synergistically with Hepatitis B virus) induce liver cancer.[58] Mycotoxin-contaminated grain and other food products have a significant impact on human and animal health globally. According to the World Health Organization, roughly 25% of the world's food may be contaminated by mycotoxins.[55]
Prevention of mold exposure from food is generally to consume food that has no mold growths on it.[41] Also, mold growth in the first place can be prevented by the same concept of mold growth, assessment, and remediation that prevents air exposure. In addition, it is especially useful to clean the inside of the refrigerator, and to ensure dishcloths, towels, sponges and mops are clean.[41]
Ruminants are considered to have increased resistance to some mycotoxins, presumably due to the superior mycotoxin-degrading capabilities of their gut microbiota.[55] The passage of mycotoxins through the food chain may also have important consequences on human health.[59] For example, in China in December 2011, high levels of carcinogen aflatoxin M1 in Mengniu brand milk were found to be associated with the consumption of mold-contaminated feed by dairy cattle.[60]
Bed
Over 47 species have been identified in pillows.[61]
Flooding
Flooding in houses causes a unique opportunity for mold growth which may be attributed to adverse health effects in people exposed to the mold, especially children and adolescents. In a study on the health effects of mold exposure after hurricanes Katrina and Rita, the predominant types of mold were Aspergillus, Penicillum, and Cladosporium with indoor spore counts ranging from 6,142 – 735,123 spores m−3.[17] Molds isolated following flooding were different from mold previously reported for non-water damaged homes in the area.[17] Further research found that homes with greater than three feet of indoor flooding demonstrated significantly higher levels of mold than those with little or no flooding.[17]
Mitigation
Recommended strategies to prevent mold include: avoiding mold-contamination; utilization of environmental controls; the use of personal protective equipment (PPE) including skin and eye protection and respiratory protection; and environmental controls such as ventilation and suppression of dust.[62] When mold cannot be prevented, the CDC recommends clean-up protocol including first taking emergency action to stop water intrusion.[62] Second, they recommend determining the extent of water damage and mold contamination. And third, they recommend planning remediation activities such as establishing containment and protection for workers and occupants; eliminating water or moisture sources if possible; decontaminating or removing damaged materials and drying any wet materials; evaluating whether the space has been successfully remediated; and reassembling the space to control sources of moisture.[62]
History
In the 1930s, mold was identified as the cause behind the mysterious deaths of farm animals in Russia and other countries. Stachybotrys chartarum was found growing on wet grain used for animal feed. Illness and death also occurred in humans when starving peasants ate large quantities of rotten food grains and cereals that were heavily overgrown with the Stachybotrys mold.[63]
In the 1970s, building construction techniques changed in response to changing economic realities including the energy crisis. As a result, homes and buildings became more airtight. Also, cheaper materials such as drywall came into common use. The newer building materials reduced the drying potential of the structures making moisture problems more prevalent. This combination of increased moisture and suitable substrates contributed to increased mold growth inside buildings.
Today, the US Food and Drug Administration and the agriculture industry closely monitor mold and mycotoxin levels in grains and foodstuffs in order to keep the contamination of animal feed and human food supplies below specific levels. In 2005 Diamond Pet Foods, a US pet food manufacturer, experienced a significant rise in the number of corn shipments containing elevated levels of aflatoxin. This mold toxin eventually made it into the pet food supply, and dozens of dogs and cats died before the company was forced to recall affected products.[64][65]
Litigation
In 2002, the U.S. International Trade Commission reported that according to one estimate, US insurers paid over $3 billion in mold-related lawsuits, more than double the previous year's total.[66] According to the Insurance Information Institute, in 2003 there were over 10,000 mold-related lawsuits pending in US state courts.[67] Most were filed in states with high humidity, but suits were on the rise in other states as well.[67] By 2004, many mold litigation settlements were for amounts well past $100,000.[68] In 2005, the U.S. International Trade Commission reported that toxic mold showed signs of being the "new asbestos" in terms of claims paid.[66] In 2012, a key appellate court in Manhattan found a consensus in the scientific literature for a causal relationship between the presence of mold and resultant illness.[69]
In 1999, an Austin, Texas, woman was awarded $32 million when she sued her insurer over mold damage in her 22-room mansion.[68]
In 2001, a jury awarded a couple and their eight-year-old son $2.7 million, plus attorney’s fees and costs, in a toxic mold-related personal injury lawsuit against the owners and managers of their apartment in Sacramento, California.[70]
In 2003, The Tonight Show co-host Ed McMahon received $7.2 million from insurers and others to settle his lawsuit alleging that toxic mold in his Beverly Hills home made him and his wife ill and killed their dog.[71] That same year environmental activist Erin Brockovich received settlements of $430,000 from two parties and an undisclosed amount from a third party to settle her lawsuit alleging toxic mold in her Agoura Hills, California, home.[72]
In 2006, a Manhattan Beach, California family received a $22.6 million settlement in a toxic mold case.[73] The family had asserted that that moldy lumber had caused severe medical problems in their child.[73] That same year, Hilton Hotels received $25 million in settlement of its lawsuit over mold growth in the Hilton Hawaiian Village's Kalia Tower.[74]
In 2010, a jury awarded $1.2 million in damages in a lawsuit against a landlord for neglecting to repair a mold-infested house in Laguna Beach, California.[75] The lawsuit asserted that a child in the home suffered from severe respiratory problems for several years as a result of the mold.[75]
In 2011, in North Pocono, Pennsylvania, a jury awarded two homeowners $4.3 million in a toxic mold verdict.[76]
Policy
While there is a national policy regarding mold, each state is responsible for independently creating and administering their own policy. For example, following Hurricane Harvey, the governor of Texas sought to expand the emergency response to allow mold remediation companies to come from out of state.[77]
See also
- Building biology
- Environmental engineering
- Environmental health
- Occupational asthma
- Occupational safety and health
References
- Kathy Orton (October 25, 2013) Mold: What every homeowner fears but probably shouldn’t, The Washington Post, accessed 16 April 2019
- Weinhold B (June 2007). "A spreading concern: inhalational health effects of mold". Environ. Health Perspect. 115 (6): A300–5. doi:10.1289/ehp.115-a300. PMC 1892134. PMID 17589582.
- Indoor Environmental Quality: Dampness and Mold in Buildings. National Institute for Occupational Safety and Health. August 1, 2008.
- Wood, Robert A.; Terr, Abba I.; Saxon, Andrew; Portnoy, Jay M.; Bush, Robert K. (2006-02-01). "The medical effects of mold exposure". Journal of Allergy and Clinical Immunology. 117 (2): 326–333. doi:10.1016/j.jaci.2005.12.001. ISSN 0091-6749. PMID 16514772.
- Stöppler, Melissa Conrad (July 16, 2014). "Mold Exposure". medicinenet.com. Retrieved February 1, 2015.
- Heseltine, Elisabeth; Rosen, ed., Jerome (2009). WHO guidelines for indoor air quality: dampness and mould (PDF). p. 93. ISBN 978-92-890-4168-3. Retrieved February 1, 2015.CS1 maint: extra text: authors list (link)
- Indoor Environmental Quality Dampness and Mold in Buildings. National Institute for Occupational Safety and Health. August 1, 2008.
- Empting, L. D. (2009). "Neurologic and neuropsychiatric syndrome features of mold and mycotoxin exposure". Toxicology and Industrial Health. 25 (9–10): 577–81. doi:10.1177/0748233709348393. PMID 19854819.
- Minnesota Department of Health. "Mold and Moisture in Homes". Minnesota North Star. Retrieved November 22, 2011.
- Gent, Janneane (2002). "Levels of Household Mold Associated with Respiratory Symptoms in the First Year of Life in a Cohort at Risk for Asthma". Environ Health Perspect. 110 (12): A781–6. doi:10.1289/ehp.021100781. PMC 1241132. PMID 12460818.
- "Best Air Purifiers for Mold and Mildew Removal Reviews UPDATED OCT 2019!". www.freshairguide.com. Retrieved 2019-11-19.
- Cohen, Aaron. "WHO Guidelines for Indoor Air Quality: Dampness and Mould" (PDF). World Health Organization. Retrieved November 18, 2011.
- Rabito, Felicia A.; Iqbal, Shahed; Kiernan, Michael P.; Holt, Elizabeth; Chew, Ginger L. (March 2008). "Children's respiratory health and mold levels in New Orleans after Katrina: A preliminary look". Journal of Allergy and Clinical Immunology. 121 (3): 622–625. doi:10.1016/j.jaci.2007.11.022. PMID 18179814.
- Rath, Barbara; Donato, Jessica; Duggan, Alyson; Perrin, Keith; Bronfin, Daniel R.; Ratard, Raoult; VanDyke, Russell; Magnus, Manya (2007-05-01). "Adverse Health Outcomes after Hurricane Katrina among Children and Adolescents with Chronic Conditions". Journal of Health Care for the Poor and Underserved. 18 (2): 405–417. doi:10.1353/hpu.2007.0043. ISSN 1548-6869. PMID 17483568.
- Mendell, Mark J.; Mirer, Anna G.; Cheung, Kerry; Tong, My; Douwes, Jeroen (June 2011). "Respiratory and Allergic Health Effects of Dampness, Mold, and Dampness-Related Agents: A Review of the Epidemiologic Evidence". Environmental Health Perspectives. 119 (6): 748–756. doi:10.1289/ehp.1002410. PMC 3114807. PMID 21269928.
- Anyanwu, Ebere C.; Campbell, Andrew W.; Vojdani, Aristo (2003). "Neurophysiological Effects of Chronic Indoor Environmental Toxic Mold Exposure on Children". The Scientific World Journal. 3: 281–290. doi:10.1100/tsw.2003.22. PMC 5974888. PMID 12806113.
- Barbeau, Deborah N.; Grimsley, L. Faye; White, LuAnn E.; El-Dahr, Jane M.; Lichtveld, Maureen (2010-03-01). "Mold Exposure and Health Effects Following Hurricanes Katrina and Rita". Annual Review of Public Health. 31 (1): 165–178. doi:10.1146/annurev.publhealth.012809.103643. ISSN 0163-7525. PMID 20070193.
- Davis, Pamela (2001). Molds, Toxic Molds, and Indoor Air Quality. California State Library. ISBN 978-1-58703-133-5.
- "Mold: A Health Hazard (Release #1605-096)". FEMA. November 8, 2005. Retrieved September 25, 2007.
- Fisk WJ, Eliseeva EA, Mendell MJ (2010). "Association of residential dampness and mold with respiratory tract infections and bronchitis: a meta-analysis". Environ Health. 9: 72. doi:10.1186/1476-069X-9-72. PMC 3000394. PMID 21078183.
- Müller FM, Seidler M (August 2010). "Characteristics of pathogenic fungi and antifungal therapy in cystic fibrosis". Expert Rev Anti Infect Ther. 8 (8): 957–64. doi:10.1586/eri.10.72. PMID 20695750.
- Simicic S, Matos T, “Microbiological diagnosis of invasive aspergillosis.” Zdravnisji vestnik-slovanian medical journal. 2010, Vol. 79, Issue 10, p. 716-725.
- Erol S (April 2010). "Nosocomial aspergillosis: epidemiology and control". Mikrobiyol Bul (in Turkish). 44 (2): 323–38. PMID 20549969.
- Nucci M, Anaissie E (October 2007). "Fusarium infections in immunocompromised patients". Clin. Microbiol. Rev. 20 (4): 695–704. doi:10.1128/CMR.00014-07. PMC 2176050. PMID 17934079.
- Gaviria JM, van Burik JA, Dale DC, Root RK, Liles WC (April 1999). "Comparison of interferon-gamma, granulocyte colony-stimulating factor, and granulocyte-macrophage colony-stimulating factor for priming leukocyte-mediated hyphal damage of opportunistic fungal pathogens". J. Infect. Dis. 179 (4): 1038–41. doi:10.1086/314679. PMID 10068606.
- McCormick A, Loeffler J, Ebel F (November 2010). "Aspergillus fumigatus: contours of an opportunistic human pathogen". Cell. Microbiol. 12 (11): 1535–43. doi:10.1111/j.1462-5822.2010.01517.x. PMID 20716206.
- Ben-Ami R, Lewis RE, Kontoyiannis DP (August 2010). "Enemy of the (immunosuppressed) state: an update on the pathogenesis of Aspergillus fumigatus infection". Br. J. Haematol. 150 (4): 406–17. doi:10.1111/j.1365-2141.2010.08283.x. PMID 20618330.
- Shang ST, Lin JC, Ho SJ, Yang YS, Chang FY, Wang NC (June 2010). "The emerging life-threatening opportunistic fungal pathogen Kodamaea ohmeri: optimal treatment and literature review". J Microbiol Immunol Infect. 43 (3): 200–6. doi:10.1016/S1684-1182(10)60032-1. PMID 21291847.
- Indian Health Service: Bemidji Area Office of Environmental Health and Engineering Environmental Health Services Section “Guideline on the Assessment and Remediation of Fungi in Indoor Environments”
- "What Is Hypersensitivity Pneumonitis?". National Heart, Lung, and Blood Institute. October 1, 2010. Retrieved January 15, 2014.
- Hardin, B. D.; Kelman, B. J.; Saxon, A. (2003). "Adverse human health effects associated with molds in the indoor environment" (PDF). Journal of Occupational and Environmental Medicine. 45 (5): 470–478. CiteSeerX 10.1.1.161.3936. doi:10.1097/00043764-200305000-00006. PMID 12762072.
- Reverberi M, Ricelli A, Zjalic S, Fabbri AA, Fanelli C (July 2010). "Natural functions of mycotoxins and control of their biosynthesis in fungi". Appl. Microbiol. Biotechnol. 87 (3): 899–911. doi:10.1007/s00253-010-2657-5. PMID 20495914.
- Bohnert M, Wackler B, Hoffmeister D (June 2010). "Spotlights on advances in mycotoxin research". Appl. Microbiol. Biotechnol. 87 (1): 1–7. doi:10.1007/s00253-010-2565-8. PMID 20376632.
- Ryan KJ; Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 633–8. ISBN 978-0-8385-8529-0.
- Etzel RA, Montaña E, Sorenson WG, et al. (August 1998). "Acute pulmonary hemorrhage in infants associated with exposure to Stachybotrys atra and other fungi". Arch Pediatr Adolesc Med. 152 (8): 757–62. doi:10.1001/archpedi.152.8.757. PMID 9701134.
- Bennett, J. W.; Klich, M. (2003). "Mycotoxins". Clinical Microbiology Reviews. 16 (3): 497–516. doi:10.1128/CMR.16.3.497-516.2003. ISSN 0893-8512. PMC 164220. PMID 12857779.
- "CDC - Mold - General Information - Basic Facts". www.cdc.gov. 2019-10-28. Retrieved 2019-11-19.
- Weinhold, Bob (2007). "A Spreading Concern: Inhalational Health Effects of Mold". Environmental Health Perspectives. 115 (6): A300–A305. doi:10.1289/ehp.115-a300. ISSN 0091-6765. PMC 1892134. PMID 17589582.
- "Agriculture". Province of Manitoba. Retrieved 2019-11-19.
- "Mycotoxins". www.who.int. Retrieved 2019-11-19.
- United States Food Safety and Inspection Service > Molds On Food: Are They Dangerous? Last Modified: August 22, 2013
- Kuhn, D. M.; Ghannoum, M. A. (2003). "Indoor Mold, Toxigenic Fungi, and Stachybotrys chartarum: Infectious Disease Perspective". Clinical Microbiology Reviews. 16 (1): 144–172. doi:10.1128/CMR.16.1.144-172.2003. PMC 145304. PMID 12525430.
- "oxigenic Fungi, and Stachybotrys chartarum: Infectious Disease Perspective" (PDF).
- loreto, olga (17 October 2018). "Mold Health Issues". EE&G Restoration Miami, FL.
- Reason Discovered for the Toxicity of Indoor Mould – ScienceDaily (Oct. 12, 2012) : https://www.sciencedaily.com/releases/2012/10/121012074655.htm
- 20-Residue and 11-residue peptaibols from the fungus Trichoderma longibrachiatum are synergistic in forming Na+/K+-permeable channels and adverse action towards mammalian cells Raimo Mikkola1,†, Maria A. Andersson1,†, László Kredics2, Pavel A. Grigoriev1,3, Nina Sundell1, Mirja S. Salkinoja-Salonen1,* doi:10.1111/febs.12010
- “Trilongins” Offer Insight into Mold Toxicity Environmental health perspectives 2/2013.
- Barbeau DN, Grimsley LF, White LE, El-Dahr JM, Lichtveld M (2010). "Mold exposure and health effects following hurricanes Katrina and Rita". Annu Rev Public Health. 31: 165–78. doi:10.1146/annurev.publhealth.012809.103643. PMID 20070193.CS1 maint: multiple names: authors list (link)
- Shoemaker RC, House DE (2006). "Sick building syndrome (SBS) and exposure to water-damaged buildings: time series study, clinical trial and mechanisms". Neurotoxicol Teratol. 28 (5): 573–88. doi:10.1016/j.ntt.2006.07.003. PMID 17010568.
- Kumar, Manisha; Verma, Rajesh K (September 2010). "Fungi diversity, their effects on building materials, occupants and control– a brief review". Journal of Scientific and Industrial Research. 69 (9): 657–661. ISSN 0975-1084.
- Wilson SC, Holder WH, Easterwood KV, et al. (2004). Identification, remediation, and monitoring processes used in a mold-contaminated high school. Adv. Appl. Microbiol. Advances in Applied Microbiology. 55. pp. 409–23. doi:10.1016/S0065-2164(04)55016-5. ISBN 9780120026579. PMID 15350804.
- Krieger J, Jacobs DE, Ashley PJ, et al. (2010). "Housing interventions and control of asthma-related indoor biologic agents: a review of the evidence". J Public Health Manag Pract. 16 (5 Suppl): S11–20. doi:10.1097/PHH.0b013e3181ddcbd9. PMC 3934496. PMID 20689369.
- Samson, Robert A., Ellen S. Hoekstra, Jens C. Frisvad (2000). Introduction to food- and airborne fungi (6., rev. ed.). Utrecht, The Netherlands: Centraalbureau voor Schimmelcultures. ISBN 978-9070351427.
- Kankolongo M, Hell K, Nawa I (June 2009). "Assessment for fungal, mycotoxin and insect spoilage in maize stored for human consumption in Zambia". J. Sci. Food Agric. 89 (8): 1366–75. doi:10.1002/jsfa.3596.
- Upadhaya S, Park M, Ha J (September 2010). "Mycotoxins and their biotransformation in the rumen: a review" (PDF). Asian-Aust. J. Anim. Sci. 23 (9): 1250–9. doi:10.5713/ajas.2010.r.06.
- Reddy K, Salleh B, Saad B, Abbas H, Abel C, Shier W (2010). "An overview of mycotoxin contamination in foods and its implications for human health". Toxin Reviews. 29 (1): 3–26. doi:10.3109/15569541003598553.
- He J, Zhou T (June 2010). "Patented techniques for detoxification of mycotoxins in feeds and food matrices". Recent Pat Food Nutr Agric. 2 (2): 96–104. doi:10.2174/1876142911002020096. PMID 20653554.
- Liu, Yan; Wu, Felicia (February 19, 2010). "Global Burden of Aflatoxin-Induced Hepatocellular Carcinoma: A Risk Assessment". Environmental Health Perspectives. 118 (6): 818–824. doi:10.1289/ehp.0901388. PMC 2898859. PMID 20172840.
- Tanuma H, Hiramatsu M, Mukai H, et al. (2000). "Case report. A case of chromoblastomycosis effectively treated with terbinafine. Characteristics of chromoblastomycosis in the Kitasato region, Japan". Mycoses. 43 (1–2): 79–83. doi:10.1046/j.1439-0507.2000.00548.x. PMID 10838854.
- "Tainted Mengniu Milk Products Caused by Mildewed Feed, Regulator Says". Bloomberg. December 26, 2011.
- Woodcock, AA; Steel, N; Moore, CB; Howard, SJ; Custovic, A; Denning, DW (January 2006). "Fungal contamination of bedding". Allergy. 61 (1): 140–2. doi:10.1111/j.1398-9995.2005.00941.x. PMID 16364170.
- Brandt, Mary; Brown, Clive; Burkhart, Joe; Burton, Nancy; Cox-Ganser, Jean; Damon, Scott; Falk, Henry; Fridkin, Scott; Garbe, Paul (2006). "Mold Prevention Strategies and Possible Health Effects in the Aftermath of Hurricanes and Major Floods". Morbidity and Mortality Weekly Report: Recommendations and Reports. 55 (8): 1–CE–4. JSTOR 24842334.
- Miller, JD; Rand, TG; Jarvis, BB (August 2003). "Stachybotrys chartarum: cause of human disease or media darling?". Medical Mycology. 41 (4): 271–91. doi:10.1080/1369378031000137350. PMID 12964721.
- Mark Brinkman (December 20, 2005). "Diamond Pet Food Recalled Due to Aflatoxin". FDA.gov. Retrieved May 9, 2014.
- FDA, Center for Veterinary Medicine Communications Staff (December 30, 2005). "FDA Investigation of Diamond Pet Food Finds Some Product Exported". FDA.gov. Retrieved May 9, 2014.
- Industry Trade and Technology Review. U.S. International Trade Commission. July 2005. ISBN 978-1457819612. Retrieved October 27, 2014.
- Jay Romano (January 26, 2003), "Your Home; Managing Mold, and Lawsuits", The New York Times
- Alex Williams. "Spore War; New York has all the right conditions for a mold outbreak: middle-age buildings, lots of lawyers—and Bianca Jagger as toxic avenger". New York Magazine. Retrieved October 26, 2014.
- Josh Barbanel (April 2, 2012). "Mold Claims For Damages Get New Life". Wall Street Journal. Retrieved October 26, 2014.
- Catherine Tapia (November 26, 2001). "Jury Awards $2.7M In Calif. Mold Case". Insurance Journal. Retrieved October 26, 2014.
- Jean Guccione (May 9, 2003). "Ed McMahon Settles Suit Over Mold for $7.2 Million; TV celebrity and his wife said contamination of their home made them ill, killed their dog". Los Angeles Times. Retrieved October 26, 2014.
- Grace Lee (September 16, 2003). "ACTIVIST ERIN BROCKOVICH SETTLES HOME MOLD SUIT". Daily News. Retrieved October 27, 2014.
- Dolan Newswire (January 11, 2006). "California construction defect lawsuit settles for $22 million". Daily Journal of Commerce. Retrieved October 26, 2014.
- "Hilton gets $25M from mold lawsuit". Honolulu Star-Bulletin. May 3, 2006. Retrieved October 26, 2014.
- Jonathan Oyama (April 29, 2010). "Family wins mold lawsuit". Coastline Pilot. Retrieved October 26, 2014.
- Steve McConnell (February 24, 2011). "$4.3M mold verdict buried in litigation". The Times-Tribune. Retrieved October 26, 2014.
- "Mold Remediation After a Flood". Boulder County. Retrieved 2017-10-25.
External links
- Barrett JR (January 2000). "Mycotoxins: of molds and maladies". Environ. Health Perspect. 108 (1): A20–3. doi:10.1289/ehp.108-a20. PMC 1637848. PMID 10620533.
- CDC.gov Mold
- US EPA: Mold Information — U.S. Environmental Protection Agency
- US EPA: EPA Publication #402-K-02-003 "A Brief Guide to Mold, Moisture, and Your Home"
- NIBS: Whole Building Design Guide: Air Decontamination
- NPIC: Mold Pest Control Information — National Pesticide Information Center
- Mycotoxins in grains and the food supply: