Blood donation restrictions on men who have sex with men
Many countries have laws that prohibit donations of blood or tissue for organ transplants from men who have sex with men (MSM), a classification of men who engage (or have engaged in the past) in sex with other men, regardless of whether they identify themselves as bisexual, gay or otherwise. Restrictions on donors are sometimes called "deferrals", since blood donors who are found ineligible may be found eligible at a later date. However, many deferrals are indefinite meaning that donation may not be accepted at any point in the future, thus constituting a de facto ban.
| Part of a series on |
| Discrimination |
|---|
|
General forms
|
| Specific forms |
|
Social
|
|
Religious
|
|
Ethnic/National
|
|
Manifestations
|
|
Policies
|
|
Countermeasures
|
|
Related topics
|
Restrictions vary from country to country, and in some countries practice of protected sex or periods of abstinence are not considered. The restrictions affect these men and, in some cases, any female sex partners. They do not otherwise affect other women, including women who have sex with women. The United States Food & Drug Administration (FDA) asserts that the one year deferral window is "supported by the best available scientific evidence".[1] However, in Canada, the deferral period has been decreased to 3 months, as of June 2019.[2] This change was also based on scientific evidence.[2]
Many LGBT organizations view the restrictions on donation as based on homophobia and not based on valid medical concern since donations are rigorously tested to rule out donors that are infected with known viruses such as HIV, HPV, Hepatitis B, and Hepatitis C. They state the deferrals are based on stereotypes.[3] Proponents of the lifetime restriction defend it because of the asserted risk of false negative test results[4] and because the MSM population in developed countries tends to have a higher prevalence of HIV/AIDS infection.[5] The UK government advisory committee, SABTO, stated in 2013 that "the risk of transfusion of HIV infected blood would increase if MSM were allowed to donate blood".[6] In July 2017 however, the UK government reduced the one year deferral window to three months, to take effect in the following months, resulting from SABTO's updated conclusions that "new testing systems were accurate and donors were good at complying with the rules". Furthermore, NHS Blood and Transplant are in the process of investigating how possible it is for MSM, depending on degree of risk, to donate without even the three-month deferral.[7] NHS has said that there is currently a limited amount of data on effective ways of conducting such risk assessments, and that the initial steps of scoping, evidence gathering and testing will potentially take up to two years to complete.[8]
Advocates for change to MSM prohibitions point out that screening of donors should focus on sexual behavior as well as safe sex practices since many MSM may always have protected sex, be monogamous, or be in other low risk categories.[3][6] Some groups in favor of lifting the restrictions support a waiting period after the blood is donated when the donor is considered to have had behavior considered higher risk, and before it is used, to match the blood bank's window of testing methods.[3] While HIV is reliably detected in 10 to 14 days with RNA testing, older testing methods provide accuracy for only up to 98% of positive cases after three months.[9]
Since 1982, the risk for HIV infection transmitted via transfusion has been almost eliminated by the use of questionnaires to exclude donors at higher risk for HIV infection and performing screening tests with highly sensitive equipment to identify infected blood donations. According to the 2015 surveillance report by Canadian Blood Services, the risk of HIV transfusion-transmitted infection was fairly low: in 1 in 21.4million donations.[10] Contaminated blood put haemophiliacs at massive risk and severe mortality, increasing the risk of common surgical procedures. People who contracted HIV from a contaminated blood transfusion include Isaac Asimov, who received a blood transfusion following a cardiac surgery.
HIV/AIDS
In many developed countries HIV is more prevalent among men who have sex with men (MSM) than among the general population.[5]
In the United States the population most affected by HIV includes gay, bisexual, and other MSM.[11] Of the 38,739 new HIV diagnoses in the US and dependent areas in 2017, 70% consisted of adult and adolescent gay and bisexual men.[11] Although approximately 492,000 sexually active gay and bisexual men are at high risk for HIV, there are more tools to prevent HIV than ever before.[11]
Current situation
List of countries with their stand on MSM blood donors
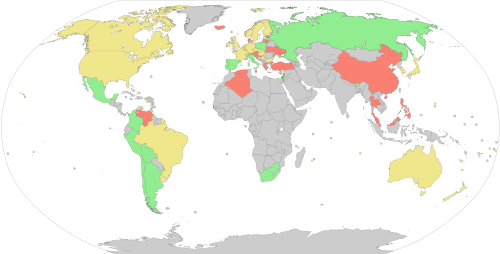
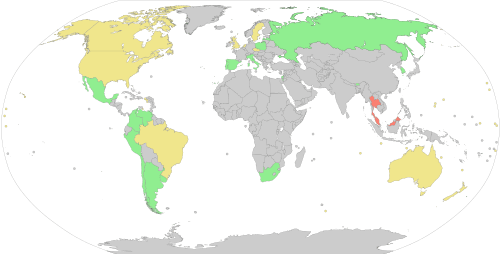
This list shows countries that had restrictions on blood donors.[12][13] Most national standards require direct questioning regarding a man's sexual history, but the length of deferral varies.
| Country | Deferral for MSM | Deferral for female sex partners of MSM | Ref(s) |
|---|---|---|---|
| No deferral | No deferral | ||
| Indefinite | |||
| No deferral | No deferral | [14][15][16][17] | |
| 1 year | 1 year | [18] | |
| Indefinite | [19] | ||
| 1 year | 1 year | In June 2019, it was explicitly reported by the LGBT media, that Belgium banned transgender individuals from donating blood.[20] | |
| No deferral | No deferral | [22] | |
| Indefinite | [23] | ||
| 1 year | 1 year | [24] | |
| No deferral | |||
| 3 months | 3 months | Since 2019, a 3-month deferral period for gay and bi men donating blood was implemented throughout Canada.[25] | |
| No deferral | No deferral | [26][27][28][29][30] | |
| Indefinite | [31] | ||
| No deferral | No deferral | [32] | |
| No deferral | [33] | ||
| Indefinite | [34] | ||
| 1 year | 1 year | [35] | |
| Indefinite | 4 months | [36] Sometime in 2019, Denmark will allow gay men to donate blood after a 4 month deferral period.[37][38] | |
| 1 year | 1 year | [39] | |
| 1 year | 1 year | [40] | |
| 1 year | [41] From 1 February 2020, France will allow gay men to donate blood after a 4-month deferral period.[42] | ||
| 1 year | [43] | ||
| Indefinite | [44] | ||
| 1 year | [45][46] | ||
| 1 year | [12] | ||
| Indefinite | |||
| 1 year | [47][48][49][50] | ||
| 1 year | No deferral | Since January 2018, Israel implemented a 1-year deferral period.[51][52][53] | |
| No deferral | No deferral | [12][54]High-risk sexual contact is banned irrespective of the partner's sex.[55] | |
| 6 months | [56] | ||
| No deferral [lower-alpha 1] | No deferral [lower-alpha 1] | [58] | |
| Indefinite | [59] | ||
| Indefinite | [60] | ||
| Indefinite | Indefinite | [61] | |
| 1 year | Since September 2019, Malta has implemented a 1-year deferral period for gay and bi men.[62][63] | ||
| No deferral | No deferral | [64] | |
| 1 year | 1 year | [65][66] | |
| 1 year | 1 year | [67] | |
| 1 year | 1 year | [68] | |
| 1 year | 1 year | [69][70] | |
| No deferral | No deferral | [71][72][73][74][75] | |
| Indefinite | [76] | ||
| No deferral [lower-alpha 1] | No deferral [lower-alpha 1] | [12][77][78][79] | |
| 1 year | 1 year | [80][81] | |
| No deferral | No deferral | [82][83] | |
| No deferral | No deferral | ||
| 6 months | [84] | ||
| Indefinite | [85] | ||
| No deferral | No deferral | [86] | |
| 1 year | No deferral | [87] | |
| 1 year | [88] | ||
| Indefinite | [89] | ||
| No deferral | No deferral | [12] | |
| 1 year | 1 year | [90][91] | |
| 1 year | 1 year | [92] | |
| 5 years | 5 years | Since May 2018, Taiwan legally by new blood donation regulations allows men who have sex with men to donate blood but only after a 5-year deferral period.[93] | |
| Indefinite | Indefinite | [94][95] | |
| Indefinite | 1 year | [96] | |
| Indefinite | |||
| Indefinite | [97] | ||
| 3 months[98] | 3 months[98] | [99][100][101] In June 2016, Northern Ireland's Minister of Health announced that the lifetime deferral on blood donation from men who have had sex with men was lifted. Currently, men who have sex with men in the last 12 months have a deferral period of 12 months before they are eligible to donate blood.[102][103] | |
| 1 year | 1 year | [104][105] | |
| 1 year | No deferral | [106] | |
| Indefinite [lower-alpha 2] | No deferral | [107] |
- People of any sexual orientation involved in any kind of sexual activity are welcome to donate blood, if they are confident that their sexual behaviour is safe and does not expose them to sexually transmitted diseases by e.g. unprotected sex with non-trusted partners, regardless of sexual orientation.[57]
- Individuals are requested to fill a "Yes/No" questionnaire about their sexual life. Direct questions like "Have you ever had any sexual intercourse with someone from your same sex?" could appear.
European Union
Italy (since 2001[108]), Latvia, Poland, Russia and Spain are the only European countries that don't have deferral policies for men who have sex with men. The donation is allowed if the donor hasn't had a risky sexual encounter, but not depending on the sexual orientation of the donor.[109][110][55] For example, in Italy, the questionnaire item for sexual behavior is symmetrical with respect to homosexual, heterosexual and bisexual intercourses and mentions them explicitly, as well as all points of sexual contact (oral, genital, anal), and does not mention usage of protection.[55]
The UK since November 2017 has implemented a 3-month deferral policy on all gay/bi men who want to donate their blood. However this does not apply to Northern Ireland, which still has a 12-month deferral period in place.[111][112][113] The Advisory Committee on the Safety of Blood, Tissues and Organs recommended the policy change after a study concluded that a total ban may breach equality legislation and that the risk of HIV reaching the blood supply would only increase by approximately 2%.[114]
In Ireland, men who have sex with men (MSM) may donate blood if they have not engaged in oral or anal sex with another man at least 12 months prior to a donation. This policy came into effect from 16 January 2017. On 27 July 2015, Tomás Heneghan, a 23-year-old University of Limerick student and journalist from Galway began a legal challenge in the High Court against the permanent deferral imposed on MSM donors.[115][116] He argued that the questionnaire and interview process used by the IBTS does not adequately assess the risk of disease transmission posed by his donation. He claims this is in breach of EU law. He said that both failed to consider the length of time between a donor's last sexual experience and the end of a "window period" in which infections are sometimes not detected. Heneghan's previous sexual activity posed no risk of infection, according to HSE-approved advice and he said the service had no evidence upon which it could legitimately impose a life-long ban on him donating blood. Following several adjournments of the case to allow the blood service and Department of Health to examine and develop the donation policies, in late June 2016 the Irish Blood Transfusion Service recommended that the lifetime ban on MSM be reduced to a 12-month ban. Later that week the Minister for Health Simon Harris agreed to the recommendations and announced the reduction would take place. However no timeline was reported for the implementation of the new policies.[117]
On 26 July 2016, Tomás Heneghan dropped his High Court challenge against the service as an end to the lifetime deferral on MSM blood donors had been announced in the interim.[118] Heneghan then wrote about his experiences of challenging the ban in a number of national media outlets.[119][120] On 2 October 2016, it was reported that Minister Harris would implement the new policy from 16 January 2017, almost seven months after he announced the policy change.[47] On 16 January 2017, Heneghan (now 25) attended a blood donation clinic in D'Olier Street, Dublin and became the first man who has had sex with another man to donate blood openly in the Republic of Ireland since the lifetime deferral policy was first introduced in the 1980s. However he also criticised the new 12-month deferral policy on MSM and called on Ireland's Health Minister to initiate a review of the IBTS and replace the 12-month deferral period for MSM with no deferral or a 3-month deferral on all donors following sexual intercourse.[121][122][123][124]
On 20 May 2019, Heneghan (27) initiated a fresh legal challenge in the High Court against the blanket deferral on men who have had oral or anal sex with another man in the previous 12-month period.[125][126][127][128]
Heneghan claims he cannot understand the reasoning behind the IBTS policy and argues that the questionnaire does not enable the IBTS to make a full evaluation of the level of risk presented by an individual donor due to their sexual behaviour. He also states that according to the IBTS's own website, there is a window period following infection during which HIV and hepatitis may not be detected in the blood and that this window is seven days for HIV and 16 days for hepatitis. He claims that a far less onerous restriction could be imposed rather than the 12-month deferral, which would protect blood recipients. He claims the decision to place an "automatic deferral" on him is unlawful and in breach of EU law and European communities regulations on the quality and safety of human blood products and that the policy is disproportionate, discriminates against homosexual and bisexual men, and breaches his constitutional rights and rights under the European Convention on Human Rights. The case is due to return to the court in July 2019.
In July 2019, a gay man in Ireland filed two formal complaints with the European Commission against the Department of Health and the Irish Blood Transfusion Service, and the Northern Ireland Blood Transfusion Service (the only part of the United Kingdom to maintain a 12-month deferral policy for MSM) over the MSM one-year deferral policy. The man, who has chosen to have his complaints examined by the Commission anonymously, is alleging the ban in both jurisdictions violates a number of European Union laws, including two European Union Directives covering the standards of quality and safety for the collection of blood by EU member states, as well as provisions contained in both the EU Charter of Fundamental Rights and the European Convention on Human Rights. The Commission has informed the man his complaints will now be considered in light of EU law.[129]
A similar policy exists in the rest of the European Union and is the prevailing interpretation of the European Union Directive 2004/33/EC article 2.1 on donor deferrals.[130] The policy, however, is not very specific and refers to "high risk sexual contact." The UK interprets the directive to include all forms of homosexual sex as falling within 2.2.2 of Annex III to the directive "Persons whose behaviour or activity places them at risk of acquiring infectious diseases that may be transmitted by blood", requiring a deferral based on the window period for the diseases involved, and sets this at 12 months, despite the Annex suggesting 6 months for risk of exposure to Hepatitis B. Hélder Trindade, President of the Portuguese Institute of Blood and Transplantation (IPST), stated in 2015 that sexually abstinent homosexuals may give blood, but that MSM is definitely seen as a risk factor.[131]
In Finland, the parliamentary ombudsman launched an investigation on the possible unconstitutionality of the lifetime ban in January 2006. In June 2008, it was concluded that the ban was not unlawful in Finland as it is based on "appropriately reasoned epidemiological information" and because it is related to sexual behaviour rather than sexual orientation. The ombudsman added that people over the age of 65 and people who lived in Britain during the bovine spongiform encephalopathy (mad cow disease) outbreak are also screened out during blood donor interviews. In December 2013, the Finnish Red Cross blood service announced it was lifting the ban and introducing a one-year deferral instead.
Since 10 July 2016, France implemented a 1-year deferral period policy on all gay and bisexual men donating blood.[132]
New Zealand
At the formation of the New Zealand Blood Service (NZBS) in 1998, the deferral period had been 10 years, but was reduced to 5 years in 2009. This was following an independent review of blood donation criteria in 2007–2008 which found no significant difference in risk of the blood supply for deferral period of 5 years compared to 10 years.[133]
In 2014, the NZBS dropped the ban period from 5 years to 1 year following the recommendation of Medsafe.[134] Their decision was mainly caused by new information about HIV transmission in Australia[135] which already had a one-year deferral period. The new 1 year deferral has been in effect since 15 December 2014.[136]
The one year deferral period for MSM is on par with the one year deferral period for persons engaging in prostitution outside of New Zealand and people who have resided in a country which has a high (1% or more) HIV prevalence.[136] Females who engage in sexual intercourse with a male who has had sex with another male are also deferred for twelve months.[137]
United States
In the US, the current guidance from the U.S. Food and Drug Administration (FDA) is to defer any male donor who has had sex with another man (MSM) in the past year. This has been so since December 2015.[138]
Female sexual partners of MSM are deferred for one year since the last exposure. This is the same policy used for any sexual partner of someone in a high risk group.[139] The argument used to follow these policies is that blood should be collected from a population that is at low risk for disease, since the tests are not perfect and human error may lead to infected units not being properly discarded, and these population groups would be considered a high risk. The policy was first put in place in 1983 by the FDA, which regulates blood donations to profit and non-profit organizations.[140]
Donors of what the FDA calls "HCT/P's", a category that includes transplants (other than organs) and some reproductive tissue, notably anonymous semen donations, are ineligible for five years after the most recent contact.[141] UNOS policies for Organ donation require the hospital receiving the organ to be notified if the donor was an MSM within the past 5 years.[142] The organs are generally used unless there is a clear positive test for a disease. The one year deferral was approved by the FDA on 21 December 2015, replacing a lifetime ban on donations from MSM.[143]
History of calls to change the policy
- In 2006, the AABB, American Red Cross, and America's Blood Centers all supported a change from the current US policy of a lifetime deferral of MSM to one year since most recent contact.[144] One model suggested that this change would result in one additional case of HIV transmitted by transfusion every 32.8 years. The AABB has suggested making this change since 1997. The FDA did not accept the proposal and had concerns about the data used to produce the model, citing that additional risk to recipients was not justified.
- On 19 August 2009, the Assembly Judiciary Committee in California passed AJR13, the U.S. Blood Donor Nondiscrimination Resolution, calling upon the FDA to end the MSM blood ban.[145]
- In April 2010, the New York City Council passed a resolution calling on the U.S. Food and Drug Administration (FDA) to eliminate the ban stating "This ban was based on prejudice, a knee-jerk reaction, and misunderstandings about the HIV/AIDS disease. Given the constant need for blood, it does not make common sense to prohibit donations from an entire population."[146]
- On 1 June 2010, the Council of the District of Columbia passed a resolution calling on the FDA to "reverse the lifetime deferment of blood donations by men who have had sex with men since 1977 in favor of a policy that protects the safety and integrity of the blood supply that is based on an up-to-date scientific criteria."[147]
- In June 2013, the American Medical Association issued a statement calling on the FDA to change the policy, stating that "The lifetime ban on blood donation for men who have sex with men is discriminatory and not based on sound science."[148][149]
- In July 2013, the American Osteopathic Association approved a policy calling on the FDA to "end the indefinite deferment period for Men who have sex with Men (MSM)", and to "modify the exclusion criteria for MSM to be consistent with deferrals for those judged to be at an increased risk of infection."[150]
- On 14 December 2015, Jordan Moll-Vigrass, Congressmen Brian Higgins and the Pride Center of Western New York held a community rally in Buffalo, New York to rally against the Food and Drug Administration policy that bans blood donations by gay and bisexual men. Moll-Vigrass, who is openly gay and had been in a committed relationship for four years, was refused as a blood donor after disclosing his sexual orientation during the questionnaire screening process. Outraged by the federal policy and disappointed by being refused as a blood donor, Moll-Vigrass started to advocate for change.[151] "The government’s unfounded policy is hurtful to the people being turned away solely based on sexual orientation and the millions of others who will be in need of a lifesaving blood donation," said Higgins. "Eligibility should be based on risk-based science rather than outdated, fear-based speculation."[152]
- On 21 December 2015, the U.S. Food and Drug Administration changed the policy by replacing the indefinite deferral with a 1-year deferral.[149] The change was proposed the previous July.[153][154]
- On 27 May 2016, the U.S. Food and Drug Administration approved of a new blood donor history questionnaire for general use by blood establishments, which is compatible with the deferral for 12 months.[155] Before this update, the approved questionnaires were compatible only with an indefinite deferral of blood donations from MSM.
- As of December 2016, the American Red Cross reports that MSM may be eligible to donate blood if they did not have sex with another man in more than 12 months. The American Red Cross reports that, in January 2017, the organization began donor reinstatement of MSM who were previously deferred from donating, and who later became qualified to donate blood in accordance with the new donation deferral period of 12 months.[156] The American Red Cross website specifies that this 12-month deferral does also apply to transgender men who have sex with men, but does not apply to transgender women who have sex with men.[157]
Others
Australia implemented a 12-month deferral; a comparison of confirmed HIV positive blood donations before and after the change did not see a statistically significant difference.[12] The Australian Red Cross Blood Service pushed to have the deferral period lowered from twelve to six months however it was rejected by the Therapeutic Goods Administration (TGA). The Red Cross will re-submit their application to reduce the deferral period to six months in 2018.[158]
Reasoning for the restrictions
Blood services first and foremost must ensure that all blood received for donation is safe for transfusion purposes. This is achieved by screening potential donors for high risk behaviors through questionnaires and interviews before blood is taken, and subsequent laboratory testing on samples of donated blood.
Blood services commonly justify their bans against MSM due to the marginal increase in the risk for transfusion-transmitted HIV.[159] Other groups with similar restrictions, or complete prohibition to donate blood, due to increased or possible risk for certain infectious diseases include intravenous drug users, recipients of animal organs or tissues, and those who have traveled or lived abroad in certain countries.[160]
In the 1980s, when the HIV/AIDS epidemic outbreak occurred, there was a high prevalence of the disease on MSM and no reliable tests for the virus, which justified blanket bans on blood donations from high-risk groups.[161]
These restrictions are similar to current restrictions on people with certain residence in the United Kingdom, France, or Saudi-Arabia during the height of the BSE ("mad cow disease") epidemic of 1980 through 1996, due to the absence of a test for its human form, Variant Creutzfeldt–Jakob disease (vCJD).[162]
In 1985, early tests using the ELISA method looked for antibodies, which are the immune system's response to the virus.[163] However, there is a window period when using this method in which a person who has been infected with HIV is able to spread the disease but may test negative for the virus.[164][165] This window period can be as long as three to six months,[166] with an average of 22 days.[167] Tests using the ELISA methods are often still used in developed countries because of their ease-of-use, as well as their fairly high sensitivity, which boasts 100% sensitivity.[168][169] To cover the window period resultant from the use of these tests, donors are also screened for high risk behaviors, one of which is a history of same-sex sexual activity among male potential donors.[170] Newer tests look for the virus itself, such as the p24 antigen test, which looks for a part of the virus on the surface of infected cells, and Nucleic acid tests (NAT), which look for the genetic material of the virus in HIV-infected cells.[171] With these tests, the window period is shorter, with an average duration of 12 days.[167] Fourth generation, or combination, HIV tests can detect HIV infection in 99% of individuals by one and a half months after infection.[172]
Risks are also associated with a non-MSM donors testing positive for HIV, which can have major implications as the donor's last donation could have been given within the window period for testing and could have entered the blood supply, potentially infecting blood product recipients. An incident in 2003 in New Zealand saw a non-MSM donor testing positive for HIV and subsequently all blood products made with the donor's last blood donation had to be recalled. This included NZ$4 million worth of Factor VIII, a blood clotting factor used to treat hemophiliacs which is manufactured from large pools of donated plasma, and subsequently led to a nationwide shortage of Factor VIII and the deferral of non-emergency surgery on hemophiliac patients, costing the health sector millions of dollars more.[133] Screening out those at high risk of blood borne diseases, including MSM, reduces the potential frequency and impact of such incidents.
Criticism of the restrictions
Need for blood
Objections to the restrictions, including those from the American Medical Association[173] and the American Red Cross, are generally based on the idea that improvements in testing and other safeguards have reduced the risk from transfusion transmitted HIV to an acceptable level. Blood shortages are common, and advocates for change to the policies point out that excluding healthy donors only makes the problem worse. In 2018, approximately 10,000 donations were still urgently needed by 10 March to continue to meet patients' needs. However, Canadian Blood Services noted that the national inventory and days on hand of several blood groups remain at critically low levels. Less than four per cent of eligible donors give blood each year.[174]
Risk of STD transmission
In some European countries, high-risk sexual intercourses lead to a temporary ban, regardless of the sex of the partner. In fact, advocates for change in other countries note that the ban encompasses all same-sex sexual contact, even if the partner's HIV status is shown beyond doubt to be negative. Advocates for change point out that a promiscuous straight male is a higher-risk donor than a gay or bisexual man in a monogamous relationship, but the former will usually be allowed to donate blood. Furthermore, in some countries, other high-risk activities determine a temporary ban, such as sexual contact with anyone who has used needles to take drugs not prescribed by their doctor, whereas MSM donors are deferred indefinitely. If a woman has had sexual contact with a man who has had sex with a man in the last year, she must wait three months from last sexual contact before donating blood.[25]
Activism regarding reform of MSM donor policies
Student and faculty activism on campuses
In Canada
- The students association at Carleton University in Ottawa, Ontario voted in 2012 to maintain a ban on blood clinics on campus.[175]
In the United States[140]
- In 2005, a student activist at the University of Vermont (UVM) filed a complaint with the university's Office of Affirmative Action, contending that American Red Cross blood drives on campus violated UVM's non-discrimination policy. The office recommended that the university no longer allow the Red Cross to conduct blood drives on campus, but the UVM administration rejected the recommendation, stating that it would not be in the interests of public health. Student and LGBT activism on the issue continued at UVM.[176] In 2007, the UVM Student Government Associated voted down, by a 16–15 vote, a nonbinding resolution calling on the university to ban blood drives over the policy.[177]
- In 2007, a group of Greek organizations at Iowa State University pulled their support for a blood drive, causing controversy.[178]
- In 2008, San Jose State University President Don Kassing suspended all blood drives on campus on the ground that the MSM policy for blood donors violated the university's non-discrimination policy.[179][180]
- In 2008, a faculty member at Sonoma State University proposed a resolution in the faculty senate to ban blood drives on campus,[181] The faculty senate passed the resolution by a 21–13 vote, clashing with the student senate, which passed a resolution earlier the same month noting the discrimination, but expressing support for the monthly blood drives because of their importance.[182][183]
- In 2010, a GLBT student group at Keene State College protested blood drives on their campus.[184]
- In 2011, the academic senate of Queens College, City University of New York recommended that all blood drives on campus should cease.[185][186]
- In 2013, a group of University of Michigan students favoring a loosening of the MSM blood-donation policy started a ""Bleeding for Equality" initiative in which individuals ineligible to donate because of the policy would bring eligible individuals to donate on their behalf, so as to both promote blood donation and also demonstrate that the amount of additional blood that could potentially be collected if the policy changed.[187][188] The Michigan Daily, the student newspaper of the University of Michigan, editorialized in favor of a loosening of the MSM blood donation policy.[189]
- On 27 July 2016, in the wake of the tragedy in Orlando on 12 June 2016, Blood is Blood hosted a blood drive on 27 July from 12 p.m. to 6 p.m. at the American Red Cross WNY Chapter Headquarters in Buffalo, NY. Jordan Moll-Vigrass, Founder of Blood is Blood & Matthew Crehan Higgins, Executive Director of the Pride Center of WNY[190] spoke at the event to raise awareness of existing archaic policies preventing many gay men from donating blood. There were reported expressions of frustration and disapproval by a number of gay and bisexual men who were forbidden to donate blood to victims, with LGBT activists across the country and a group of Democratic lawmakers[191] urging the ban to be lifted. The FDA later said it had no plans of changing the regulation and will reevaluate its policies "as new scientific information becomes available".[192][193][194]
In the United Kingdom
- The National Union of Students LGBT Campaign runs a "Donation Not Discrimination" campaign to have the blood ban changed, while also advocating continued donation by those who are not banned from donating.
Elsewhere
In 2015, Welsh writer and poet RJ Arkhipov exhibited a poetry series written with his own blood as ink in protest of the MSM blood donor restrictions. His poem Inkwell discusses the shame and stigma surrounding "gay blood". An abecedarian poem, each line of Inkwell's five quatrains begins with letters from each of the blood groups, alternating between A, B, AB and O.[195][196][197]
Court cases
In 2018 the European Court of Human Rights took up a case of a French citizen who was prevented from donating blood.[198]
See also
- Gay sexual practices
- Terminology of homosexuality
References
- "Gay and Bisexual Men Can Soon Donate Blood – but There's a Catch". US News & World Report. Retrieved 12 June 2016.
- "Canadian Blood Services Annual Report 2018-2019" (PDF). Retrieved 18 November 2019.
- Schoettes, Scott (December 2012). "Blood Donations Questions". Adelante Magazine.
- Stier, Jeff (13 June 2007). "Blood for Sale". HuffingtonPost.com, Inc. Retrieved 5 April 2008.
- UNAIDS 2006 report on the global AIDS epidemic, Chapter 05, June 2006
- Bloxham, Andy (10 April 2011). "Homosexual men allowed to give blood but sex banned for decade". Telegraph.
- "Blood donation rules relaxed for gay men and sex workers". BBC.co.uk. 23 July 2017. Retrieved 28 August 2017.
- "Scientific review offers chance for more people to give blood". NHS Blood and Transplant. Retrieved 19 November 2019.
- "HIV Test Window Periods". San Francisco AIDS Foundation. San Francisco AIDS Foundation. 2014. Retrieved 19 February 2015.
- "Surveillance Report 2015" (PDF). Retrieved 18 November 2019.
- "HIV and Gay and Bisexual Men". 12 November 2019. Retrieved 18 November 2019.
- Seed, Clive R.; Kiely, Philip; Law, Mathew; Keller, Anthony J. (December 2010). "No evidence of a significantly increased risk of transfusion-transmitted human immunodeficiency virus infection in Australia subsequent to implementing a 12-month deferral for men who have had sex with men". Transfusion. 50 (12): 2722–2730. doi:10.1111/j.1537-2995.2010.02793.x. PMID 20663106.
- "Mclaughlin Report on Risk Management for Canadian Blood Services" (PDF). McLaughlin Center for Population Health Risk Assessment, University of Ottawa. 31 January 2007. p. 28. Retrieved 25 May 2008.
- Matthew Corb (16 September 2015). "Health Ministry Removes Ban on Homosexual Blood Donors". The Argentina Independent. Archived from the original on 19 December 2018. Retrieved 17 September 2015.
- Stern, Mark Joseph (17 September 2015). "Argentina Abolishes Gay Blood Ban". Slate.
- "Nuevas normas para la donación de sangre" (in Spanish). 16 September 2015.
- Criterios para la selección de donantes de sangre (in Spanish)
- "FAQs – Who can give". Australian Red Cross Blood Service. 18 April 2012. Retrieved 7 June 2012.
- "Rotes Kreuz: Wer darf Blutspenden?". Roteskreuz.at. Retrieved 20 July 2012.
- "Red Cross bans transgender people from donating blood in Belgium". 13 June 2019.
- "Homo's mogen binnenkort bloed geven, "maar enkel als ze twaalf maanden geen seks hebben gehad"".
- "Who can be a blood donor?". Bhutan Medical and Health Council. 14 June 2013. Archived from the original on 1 January 2015. Retrieved 1 January 2015.
- "Decreto Supremo Nº 24547 de 1997". Archived from the original on 6 October 2018. Retrieved 6 March 2017.
- "Ordinance No. 2712 of November 12, 2013" (PDF) (in Portuguese). Archived from the original (PDF) on 17 January 2016. Retrieved 2 September 2015.
- "Men who have sex with men | Canadian Blood Services". blood.ca. Retrieved 3 November 2019.
- "Gays and lesbians in Chile now allowed to donate blood". Santiago Times. 25 April 2013. Archived from the original on 28 April 2015.
- Chile drops blood donation ban for gays. Washington Blade
- Norma que regula el procedimiento de atención de donantes de sangre (in Spanish)
- Guía Criterios Selección Donantes de Sangre (in Spanish)
- Histórico: Termina prohibición a gays, lesbianas y bisexuales para donar sangre en Chile (in Spanish)
- "China says lesbians may donate blood, but not gay men — Latitude News". Latitudenews.com. Archived from the original on 27 February 2014. Retrieved 4 March 2014.
- "Homosexualidad no es impedimento para donar sangre: Corte Constitucional" (in Spanish). 28 May 2012.
- García, Sagal Davison; Murillo, Jason Hernández (27 July 2015). "La igualdad del sistema costarricense enfocado en la percepción de la población de mujeres y homosexuales" (in Spanish). Mi tinta es el alma. Archived from the original on 13 March 2016. Retrieved 7 February 2016.
- Ministry of Health (Croatia) (16 December 1998). "Pravilnik o krvi i krvnim sastojcima" [Bylaw for blood and its contents] (in Croatian). Narodne novine. Retrieved 18 July 2011.
E`lanak 16. Trajno se iskljue`uju kao davatelji krvi: [...] osobe sa homoseksualnim ponašanjem [...]
- "Doporučení Společnosti pro transfuzní lékařství ČLS JEP č. STL2007_03 ze dne 12. 4. 2007 verze 6 (2012_04)" (DOC) (in Czech). Společnost pro transfuzní lékařství ČLS JEP. p. 8. Retrieved 7 February 2013.
- "Seksuel kontakt" (in Danish). Bloddonorerne i Danmark. Retrieved 9 September 2017.
- "Denmark to revise blood donation laws in 2019". 24 August 2018.
- "Denmark announces gay men will be able to donate blood by 2019". 24 August 2018.
- "Vereloovutusest" (in Estonian). Tartu Ülikooli Kliinikumi Verekeskus. Retrieved 22 November 2015.
- "Can you donate". Finnish Red Cross Blood Service. Retrieved 27 January 2019.
- "After 30-year ban, gay men in France allowed to donate blood". france24. 11 July 2016. Retrieved 12 July 2016.
- "Don du sang : la période d'abstinence imposée aux homosexuels réduite d'un an à 4 mois" [Gift of blood: the period of abstinence imposed on homosexuals reduced from one year to 4 months] (in French). L'Express. 17 July 2019.
- "Richtlinie zur Gewinnung von Blut und Blutbestandteilen und zur Anwendung von Blutprodukten (Richtlinie Hämotherapie)" [Guidelines for the collection of blood and blood components and the use of blood products (haemotherapy)] (PDF). German Medical Association. 2017. Archived from the original (PDF) on 13 April 2018. Retrieved 11 March 2019.
- "Why some countries still ban gay men from giving blood". The Economist. 16 April 2018. ISSN 0013-0613. Retrieved 31 October 2019.
- "Relaxed rules will allow gay men to donate blood in Hong Kong". 14 September 2017.
- "What should you know about the Health history Enquiry in Blood Donation?" (PDF) (in Chinese and English). Hong Kong: Hong Kong Red Cross Blood Transfusion Service. 2008. Archived from the original (PDF) on 29 October 2012. Retrieved 14 August 2011.
- "Ban on gay men giving blood to end in new year – Independent.ie".
- McNamee, Michael Sheils. "Lifting of blood ban welcome – but system will still discriminate against gay men in relationships".
- "Ireland lifts ban on gay men donating blood – BelfastTelegraph.co.uk". Belfasttelegraph.co.uk.
- "Lifelong ban on gay men donating blood to be lifted". Archived from the original on 28 June 2016. Retrieved 29 June 2016.
- "Israel has lifted its ban on gay and bi men donating blood".
- "Israel to allow sexually active gay and bi men to donate blood". 11 January 2018.
- Efrati, Ido (25 September 2018). "Pilot Program in Israel Will Allow Gay Men to Donate Blood Without Abstaining From Sex". Haaretz.
- Administrator. "GAY E DONAZIONE DEL SANGUE". www.avisgiarre.it. Archived from the original on 22 February 2016. Retrieved 13 February 2016.
- Ministero della Salute. "Criteri per la selezione del donatore" (PDF). p. 39.
- "エイズ、肝炎などのウイルス保有者、またはそれと疑われる方" (in Japanese). Japanese Red Cross Society. Retrieved 14 June 2016.
... 輸血を必要とする患者さんへの感染を防ぐため、過去6カ月間に下記に該当する方は、献血をご遠慮いただいています。... 男性どうしの性的接触があった。 (Translation: To prevent infecting patients requiring blood transfusion, those who match any of the following within the last six months should refrain from donating blood. ... Sexual contact between two males.)
- "Archived copy". Archived from the original on 14 October 2013. Retrieved 21 November 2013.CS1 maint: archived copy as title (link)
- "Donora anketa" (in Latvian). Valsts asinsdonoru centrs. Retrieved 1 November 2015.
- "Criteria for blood donor selection" (PDF). Lebanese Committee of Blood Transfusion. Retrieved 12 July 2016.
- "Questionnaire for Donors of Blood and Blood Products" (PDF). VšĮ „Nacionalinis kraujo centras". Retrieved 1 November 2015.
- "Kriteria Penderma Darah" (in Burmese). Archived from the original on 3 August 2016. Retrieved 6 May 2016.
- "Gay men to be allowed to donate blood from Monday – the Malta Independent".
- "Gay Blood Donation Finally Kicks off in Malta... Caveats and All". 20 September 2019.
- Roberts, Scott (27 December 2012). "Mexico lifts ban on gay men donating blood". PinkNews.co.uk.
- TFE, tfe.nl (1 July 2013). "Bloed geven – Risicofactoren hiv mannen" [Giving Blood – Risk Factors of HIV for men] (in Dutch). Sanquin.nl. Archived from the original on 6 April 2015.
- TFE, tfe.nl (1 July 2013). "Bloed geven – Risicofactoren hiv vrouwen" [Giving Blood – Risk Factors of HIV for women] (in Dutch). Sanquin.nl. Archived from the original on 6 April 2015.
- "Detailed eligibility criteria". New Zealand Blood Service. 8 January 2015. Retrieved 1 February 2015.
- "Hvem kan, og hvem kan ikke være blodgivere". Helsedirektoratet. 3 April 2017. Retrieved 9 September 2017.
- Connolly, Marie-Louise (31 August 2016). "Gay blood donation: Lifetime ban in NI on gay men donating blood lifted". BBC News – via www.bbc.com.
- "Gay Men Can Now Donate Blood in Northern Ireland – VICE – United Kingdom". 1 September 2016.
- "Atención: En el Perú las personas LGBT sí pueden donar sangre" (in Spanish). 8 July 2015.
- "Mujer no pudo donar sangre por ser lesbiana: esto dice la ley" (in Spanish). 8 July 2015.
- Programa Nacional de Hemoterapia y Bancos de Sangre Archived 1 July 2018 at the Wayback Machine (in Spanish)
- Resolución Ministerial Nº 614-2004/MINSA "Aprueban el Sistema de Gestión de la Calidad del PRONAHEBAS". Archived 23 November 2015 at the Wayback Machine (in Spanish)
- EG05 – TB05 Requisitos de calificación del donante. Ministerio de Salud (in Spanish)
- "What does the term "Donor Referral" mean?". Republic of the Philippines Department of Health.
- "Internetowy System Aktów Prawnych" (in Polish). Isap.sejm.gov.pl. 24 May 2005.
- Slezak, Klaudiusz (9 May 2008). "Narodowe Centrum Krwi: Nie będziemy dyskryminować homoseksualistów" (in Polish). Wiadomosci.gazeta.pl. Archived from the original on 29 June 2009. Retrieved 30 July 2011.
- "Honorowe krwiodawstwo mężczyzn homo- i biseksualnych. Fakty i mity" [Honorable blood donation by gay and bisexual men. Facts and Myths] (in Polish). Kph.org.pl. 23 September 2009.
- "AR aprova diploma que permite a homossexuais dar sangue". diariodigital.sapo.pt (in Portuguese). 8 April 2010. Archived from the original on 22 November 2015. Retrieved 29 July 2018.
- "Direcção-Geral de Saúde – Norma nº 009/2016 de 19/09/2016 atualizada a 16/02/2017 – Comportamentos de Risco com Impacte na Segurança do Sangue e na Gestão de Dadores: Critérios de Inclusão e Exclusão de Dadores por Comportamento Sexual".
- "Приказ Минздравсоцразвития России от 16.04.2008 N 175н" (in Russian). Российская газета. 24 May 2008. Retrieved 13 November 2013.
- Россиянам вольют "голубую кровь" (in Russian). Полит.ру. 23 May 2008. Retrieved 13 November 2013.
- "Comments on FDA's blood donor deferral recommendations for reducing the risk of human immunodeficiency virus (HIV) transmission" (PDF). Plasma Protein Therapeutics Association.
- "About AIDS and HIV – When Not To Donate". Retrieved 6 May 2016.
- DeBarros, Luiz (20 May 2014). "SA finally ends gay blood donation ban". Mamba Online. Retrieved 20 May 2014.
- "FAQ". Korean Red Cross Blood Services.
- "Dotazník pre darcov krvi, plazmy a krvných buniek" (PDF). 1 May 2016. Archived from the original (PDF) on 24 September 2017. Retrieved 24 September 2017.
- "The Republic of Slovenia Institute for Transfusion: Who cannot donate blood". Ztm.si. Archived from the original on 19 February 2012. Retrieved 20 July 2012.
- Gallagher, James (8 September 2011). "Gay men blood donor ban to be lifted". BBC News Online.
- "Krav på blodgivares lämplighet" [Regulations on blood donation from the National Board of Health and Welfare, SOSFS 2009:28 Appendix 5 Section B:3] (PDF) (in Swedish). Archived from the original (PDF) on 23 September 2017. Retrieved 19 April 2015.
- "Switzerland lifts lifetime ban on gay men donating blood". 31 January 2017.
- News, Taiwan. "Blood donation rules for gay men in Taiwan to... – Taiwan News".
- "thai red cross reverses ban on gay blood donors – Gay News Asia". 15 April 2008.
- "Gay men launch online attack on Thai Red Cross over ban on gay blood donors". 28 February 2013.
- "Donating Blood". Government of Trinidad and Tobago. 2017.
- "Порядок медичного обстеження донорів крові та (або) її компонентів". Ministry of Health of Ukraine. 2005.
- "New reduced ban on blood donation for gay and bi men starts today". 27 November 2017.
- Greenfield, Patrick (23 July 2017). "Gay men to be allowed to give blood three months after sex". the Guardian.
- "Blood donation rules relaxed for gay men and sex workers". BBC News. 23 July 2017. Retrieved 23 July 2017.
- "Blood donor rules for gay men relaxed". BBC News. 2 August 2017 – via www.bbc.com.
- "Can I Donate? – Northern Ireland Blood Transfusion Service". Retrieved 31 October 2019.
- Connolly, Marie-Louise (1 September 2016). "NI's 'gay blood' ban is lifted". Retrieved 31 October 2019.
- "FDA updates blood donor deferral policy". U.S. Food and Drug Administration. U.S. Food and Drug Administration. Retrieved 22 December 2015.
- "Revised Recommendations for Reducing the Risk of Human Immunodeficiency Virus Transmission by Blood and Blood Products – Questions and Answers". U.S. Food and Drug Administration. U.S. Food and Drug Administration. Retrieved 16 June 2016.
- "Analizan cambiar norma que impide donar sangre a gays". El Observador (in Spanish). 10 July 2016.
- "Homophobia in our blood". ideas.ted.com. 22 June 2016. Retrieved 31 October 2019.
- Chi può donare il sangue in Italia?
- "Donantes de sangre – Centro de Donación de Sangre de Cruz Roja" (in Spanish). Cruz Roja Española. Retrieved 5 August 2017.
- "España no discrimina a los donantes por su orientación sexual". El Mundo (in Spanish). 29 April 2015. Retrieved 6 August 2017.
- "Blood donation rules have changed".
- "Donor selection criteria review". Department of Health and SaBTO, Blood Donor Selection Steering Group. Retrieved 8 September 2011.
- Waygood, James (8 September 2011). "UK Government lifts lifetime ban on gay blood donation". So So Gay. Archived from the original on 12 May 2012. Retrieved 20 July 2012.
- "Homosexual men allowed to give blood but sex banned for decade". The Daily Telegraph. Retrieved 20 July 2012.
- Healy, Catherine. "This 23-year-old student is challenging Ireland's gay blood donation ban".
- "Gay man brings legal challenge over blood donation ban". The Irish Times.
- "IBTS votes to end ban on gay men donating blood". RTÉ News. 23 June 2016. Retrieved 21 August 2016.
- "Gay man drops challenge to blood donation ban after change in policy announced by Health Minister – Independent.ie". Retrieved 21 August 2016.
- "Tomás Heneghan on his High Court case: Why was I shaming the family? Why was my sex life being opened up to public scrutiny? – Independent.ie". Retrieved 21 August 2016.
- Heneghan, Tomás. "'They openly debated what sort of sex I had': What it was like being at the centre of the blood-ban case". Retrieved 21 August 2016.
- http://theoutmost.com/news/irish-lifetime-ban-blood-donation-lifted-gay-men/?platform=hootsuite
- "Blood Transfusion Service finally lifts ban on gay men donating blood". Irish Examiner. 17 January 2017.
- "Gay donor: 'Tooth and nail' battle to give blood at an end". The Irish Times.
- "'I abstained from sex for 23 months': Gay UL student wins fight over blood donations".
- O'Faolain, Aodhan. "Policy on gay men donating blood challenged in High Court". Irishtimes.com. Retrieved 25 May 2019.
- O'Faolain, Aodhan. "Man brings High Court challenge over IBTS policy on gay men donating blood". TheJournal.ie. Retrieved 25 May 2019.
- O'Faolain, Aodhan (21 May 2019). "Gay man challenges blood donor sex policy". The Times. Retrieved 25 May 2019.
- "Man brings court challenge against blood transfusion service after they prevented him from donating". independent.ie. Retrieved 25 May 2019.
- Dunne, Peter. "Irish man files formal complaint with European Commission over gay blood ban". GCN.ie. Retrieved 5 August 2018.
- "Commission Directive 2004/33/EC of 22 March 2004" (PDF). Iospress.metapress.com. Retrieved 28 October 2013.
- "Homosexuals may give blood if they abstain from sex (Homossexuais só podem dar sangue em abstinência sexual)" (in Portuguese). tvi24. 29 April 2015. Retrieved 5 November 2015.
The President of the Institute of Blood explains that "sexual contact by men with other men is definitely (seen) as a risk factor" (Presidente do Instituto do Sangue explica que "contacto sexual de homens com outros homens é definido como fator de risco")
- "France to Lift Ban on Gay Men Donating Blood". The New York Times. 4 November 2015. Retrieved 4 November 2015.
- "Behavioural Donor Deferral Criteria Review – Final Report to the New Zealand Blood Service" (PDF). April 2008. Archived from the original (PDF) on 29 October 2012. Retrieved 20 July 2012.
- "New one year blood ban now in place". 15 December 2014. Archived from the original on 9 February 2015. Retrieved 1 February 2015.
- "New Zealand: New one-year blood ban now in place". San Diego Gay and Lesbian News. 15 December 2014. Retrieved 1 February 2015.
- "Revised Donor Eligibility Criteria". www.nzblood.co.nz. Retrieved 30 November 2019.
- "Detailed Eligibility Criteria". New Zealand Blood Service. Retrieved 21 April 2015.
- "Health Index". ABC News.
- 1992 Recommendations for the prevention of Human Immunodeficiency Virus Transmission by Blood and Blood Products Archived 29 June 2007 at the Wayback Machine
- "Blood Donations from Men Who Have Sex with Other Men Questions and Answers (published: August 19th, 2013)". FDA.gov. Retrieved 26 August 2014.
- FDA/CBER – Guidance for Industry: Eligibility Determination for Donors of Human Cells, Tissues, and Cellular and Tissue-Based Products (HCT/Ps) Archived 19 March 2008 at the Wayback Machine
- "OPTN/UNOS POLICY 4" (PDF). Archived from the original (PDF) on 19 June 2010. Retrieved 20 July 2012.
- "FDA: Gay men can once again donate blood in U.S., if they haven't had sex for a year".
- "Meeting of Blood Products Advisory Committee" (133MB). Food and Drug Administration. 9 March 2006. p. 66. Retrieved 25 May 2008.
- "Ending the Federal Ban on Gay Blood Donations". California Progress Report. 19 August 2009. Retrieved 20 July 2012.
- "Legislative and Community Report" (PDF). New York: New York City Council. 30 April 2010. p. 2. Archived (PDF) from the original on 17 September 2011. Retrieved 18 September 2010.
- "A Resolution 18-486 : In the Council of the District of Columbia". Dcregs.dc.gov. 1 June 2010. Archived from the original on 29 October 2013. Retrieved 28 October 2013.
- no author listed (18 June 2013). "AMA Adopts New Policies on Second Day of Voting at Annual Meeting". ama-assn.org. American Medical Association. Retrieved 16 January 2014.
- Mohney, Gillian (20 June 2013). "FDA Ban on Gay Men as Blood Donors Opposed by American Medical Association". ABC News. Retrieved 1 August 2013.
- "American Osteopathic Association Calls for Removing FDA's Blood Donor Ban". Osteopathic.org. 20 July 2013. Archived from the original on 21 August 2013. Retrieved 1 August 2013.
- Pasceri, Joanna (December 2015). "Gay man fighting for right to give blood". WKBW.
- "Community Rally Against FDA". Congressmen Brian Higgins. 14 December 2015.

- U.S. Food and Drug Administration (May 2015). "Revised Recommendations for Reducing the Risk of Human Immunodeficiency Virus Transmission by Blood and Blood Products" (PDF). Retrieved 2 July 2015.
- Sabrina Tavernise (23 December 2014). "F.D.A. Easing Ban on Gays, to Let Some Give Blood". New York Times. Retrieved 26 December 2014.
- "Blood Donor History Questionnaires".
- "Eligibility Criteria by Topic".
- "LGBTQ+ Donors". American Red Cross. Retrieved 5 July 2017.
- "Why Can't Gay Men Donate Blood in Australia?". VICE. 17 June 2016. Retrieved 28 August 2017.
- Davison KL, Conti S, Brailsford SR. The risk of transfusion-transmitted HIV from blood donations of men who have sex with men, 12 months after last sex with a man: 2005–2007 estimates from England and Wales. Vox Sang. 2013;105: 85–8
- U.S. Food and Drug Administration. Blood donations from men who have sex with other men questions and answers. Accessed at www.fda.gov/biologicsbloodvaccines/bloodbloodproducts/questionsaboutblood/ucm108186.htm on 10 December 2014.
- Karamitros, G., Kitsos, N., & Karamitrou, I. (2017). The ban on blood donation on men who have sex with men: time to rethink and reassess an outdated policy. The Pan African medical journal, 27, 99. doi:10.11604/pamj.2017.27.99.12891
- Strong, D. M., & Katz, L. (2002). Blood-bank testing for infectious diseases: How safe is blood transfusion? Trends in Molecular Medicine, 8(7), 355–358. Retrieved from http://resolver.scholarsportal.info/resolve/14714914/v08i0007/355_btfidhsibt
- Roberts, Bill D. (Spring 1994). "HIV Antibody Testing Methods" (PDF). Update on HIV/AIDS. 26: 13–14.
- "The Window Period | HIV Risk Reduction Tool | CDC". wwwn.cdc.gov. Retrieved 19 November 2019.
- "HIV testing". Canadian AIDS Society. 29 November 2016. Retrieved 19 November 2019.
- "San Francisco AIDS Foundation: HIV Testing". Sfaf.org. Archived from the original on 7 August 2010. Retrieved 20 July 2012.
- FDA Approves First Nucleic Acid Test (Nat) System To Screen Whole Blood Donors For Infections With Human Immunodeficiency Virus (Hiv) And Hepatitis C Virus (Hcv) Archived 21 February 2008 at the Wayback Machine
- "HIV Antibody Assays". hivinsite.ucsf.edu. Retrieved 19 November 2019.
- Desai, Darash; Wu, Grace; Zaman, Muhammad H. (21 January 2011). "Tackling HIV through Robust Diagnostics in the Developing World: Current Status and Future Opportunities". Lab on a Chip. 11 (2): 194–211. doi:10.1039/c0lc00340a. ISSN 1473-0197. PMC 5181793. PMID 21125097.
- O’Brien SF, Ram SS, Yi QL, Goldman M. Donor’s understanding of the definition of sex as applied to predonation screening questions. Vox Sang. 2008;94(4):329–33.
- "Types of HIV Tests | HIV Risk Reduction Tool | CDC". wwwn.cdc.gov. Retrieved 19 November 2019.
- "HIV testing technologies". www.catie.ca. Retrieved 19 November 2019.
- "Policies on Lesbian, Gay, Bisexual, Transgender & Queer (LGBTQ) Issues – AMA". www.ama-assn.org.
- "Donate now: urgent need for blood across Canada continues | Canadian Blood Services". blood.ca. Retrieved 2 November 2019.
- "Blood clinic ban on campus upheld due to policy on gay men". CBC News. 10 July 2012.
- Ken Picard (18 April 2008). "Queer Community Seeing Red Over Blood-Donation Policy". Seven Days.
- UVM student government rejects ban on Red Cross blood drives, Associated Press (18 October 2007).
- Kevin Newman (26 February 2007). "LETTER: Political correctness may cripple blood drive turnout". Iowa State Daily.
- Potts, Carolyn (6 February 2008). "College protests blood drives". Badger Herald.
- "President's Message: Campus Blood Drives". Office of the President, San Jose State University. 29 January 2008.
- Norton, Laura (8 March 2008). "Battle over blood". Press Democrat.
- Sonoma State faculty senate OKs resolution opposing blood drives, Bay City News Service (25 April 2008).
- SSU faculty backs blood drive ban, says federal policy biased, Press Democrat (25 April 2008).
- "Students protest discriminatory blood donor rule". Keene Sentinel. 17 February 2016. Archived from the original on 8 August 2016. Retrieved 15 June 2016.
- "Queens College Academic Senate Bans Discriminatory Blood Drives" (Press release). 14 April 2011.
- "Minutes of the Academic Senate of Queens College" (PDF). 14 April 2011.
- "Blood Battle at the University of Michigan".
- Gast, Betsy; Fournier, Chelsea (21 October 2013). "Viewpoint: Ending a discriminatory blood policy". The Michigan Daily.
- "Editorial: The battle for donor equality". The Michigan Daily. 22 October 2013.
- "Pride Center of WNY".
- Barron-Lopez, Laura (13 June 2016). "Democrats Call on FDA To End Ban on Blood Donations From Gay Men". The Huffington Post. Retrieved 31 July 2016.
- Levin, Sam (14 June 2016). "Activists urge US to end ban on gay men donating blood after Orlando massacre". The Guardian. Retrieved 15 June 2016.
'The FDA has examined the possibility of eliminating all deferrals for HIV and simply relying on testing of donated blood or reducing the deferral window; however, scientifically robust data are not available to show that this would not lead to decreased safety of the blood supply,' the agency said in a statement to the Guardian.
- Margolin, Emma (15 June 2016). "Blood Donations Skyrocket, but Gay Men Left Out". NBC News. Retrieved 15 June 2016.
- McKenzie, Sheena (14 June 2016). "Gay men outraged over continued ban on blood donation". CNN. Retrieved 11 July 2016.
- "RJ Arkhipov Works With His Own Blood to Protest Ban on Gay Donors". Out. 25 September 2015.
- "Gay Welsh poet tackles the stigma of 'gay blood' on World Blood Donor Day". Attitude. 14 June 2017.
- "This gay poet is writing in his own blood to protest gay blood donations rules". PinkNews. 23 June 2017.
- "Gay man banned from giving blood takes case to European court". 22 June 2018.
External links
- FDA:Blood Products Advisory Committee, 09Mar2006 transcript See page 53 (page 59 of the pdf) for the discussion of test error rates. Warning: this is a 133 MB scanned transcript.
- CDC: HIV/AIDS among Men Who Have Sex with Men
- British Medical Journal Debate: Should men who have ever had sex with men be allowed to give blood? No
- British Medical Journal Debate: Should men who have ever had sex with men be allowed to give blood? Yes