Men's health
Men's health refers to a state of complete physical, mental, and social well-being, as experienced by men, and not merely the absence of disease or infirmity.[1] Differences in men's health compared to women's can be attributed to biological factors (such as male genitalia or hormones), behavioural factors (men are more likely to make unhealthy or risky choices and less likely to seek medical care) and social factors (e.g.: occupations).[2] These often relate to structures such as male genitalia or to conditions caused by hormones specific to, or most notable in, males. Some conditions that affect both men and women, such as cancer, and injury, also manifest differently in men.[3] Men's health issues also include medical situations in which men face problems not directly related to their biology, such as gender-differentiated access to medical treatment and other socioeconomic factors.[4][5][6] Some diseases that affect both genders are statistically more common in men. Outside Sub-Saharan Africa, men are at greater risk of HIV/AIDS – a phenomenon associated with unsafe sexual activity that is often nonconsensual.[7][8]
Definition
The concept of "men's health" is variously defined. A 2016 international literature review found seven different meanings, and proposed a definition based on the WHO general definition of health, that avoided male-specific disease and male stereotypes.[9]
Life expectancy
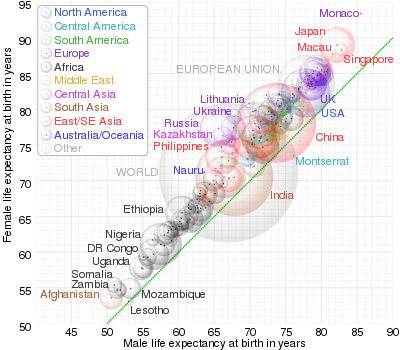
Despite overall increases in life expectancy globally, men's life expectancy is less than women's, regardless of race and geographic regions.[10][11] The global gap between the life expectancy of men and women has remained at approximately 4.4 years since 2016, according to the World Health Organization.[12] However, the gap does vary based on country, with low income countries having a smaller gap in life expectancy.[13] Biological, behavioural, and social factors contribute to a lower overall life expectancy in men, however the individual importance of each factor is not known.[14] Overall attitudes towards health differ by gender. Men are generally less likely to be proactive in seeking healthcare, resulting in poorer health outcomes.[15]
Biological influences on lower male life expectancies include genetics and hormones. For males, the 23rd pair of chromosomes are an X and a Y chromosome, rather than the two X chromosomes in females.[11] The Y chromosome is smaller in size and contains less genes. This distinction may contribute to the discrepancy between men and women's life expectancy, as the additional X chromosome in females may counterbalance potential disease producing genes from the other X chromosome. Since males don't have the second X chromosome, they lack this potential protection.[11] Hormonally, testosterone is a major male sex hormone important for a number of functions in males, and to a lesser extent, females.[16] Low testosterone in males is a risk factor of cardiovascular related diseases.[17] Conversely, high testosterone levels can contribute to prostate diseases.[11] These hormonal factors play a direct role in the life expectancy of men compared to women.
In terms of behavioural factors, men have higher levels of consumption of alcohol, substances, and tobacco compared to women, resulting in increased rates of diseases such as lung cancer, cardiovascular disease, and cirrhosis of the liver.[11][18] These diseases influence the overall life expectancy of men. For example, according to the World Health Organization, 3.14 million men died from causes linked to excessive alcohol use in 2010 compared to 1.72 million women. Men are more likely than women to engage in over 30 risky behaviours associated with increased morbidity, injury, and mortality.[19][20] Additionally, despite a disproportionately lower rate of suicide attempts than women, men have significantly higher rates of death by suicide.[21][22][23]
Social determinants of men's health involve factors such as greater levels of occupational exposure to physical and chemical hazards than women.[15] Historically, men had higher work related stress, which negatively impacted their life expectancy by increasing the risk of hypertension, heart attack, and stroke.[11] However, it is important to note that as women's role in the workplace continues to be established, these risks are no longer specific to just men.[11]
Mental health
Stress
Although most stress symptoms are similar in men and women, stress can be experienced differently by men.[24] According to the American Psychological Association, men are not as likely to report emotional and physical symptoms of stress compared to women.[24] Men are more likely to withdraw socially when stressed and are more likely to report doing nothing to manage their stress.[24] In terms of causes of stress, men are more likely to cite that work is a source of stress than women (who are more likely to report that money and the economy are a source of stress).[24]
Mental stress in men is associated with various complications which can affect men’s health: high blood pressure and subsequent cardiovascular morbidity and mortality,[25] cardiovascular disease,[26] erectile dysfunction (impotence)[27] and possibly reduced fertility (due to reduced libido and frequency of intercourse).[28]
Fathers experience stress during the time shortly before and after the time of birth (perinatal period).[29] Stress levels tend to increase from the prenatal period up until the time of birth, and then decrease from the time of birth to the later postnatal period.[29] Factors which contribute to stress in fathers include negative feelings about the pregnancy, role restrictions related to becoming a father, fear of childbirth, and feelings of incompetence related to infant care.[29] This stress has a negative impact on fathers.[29] Higher levels of stress in fathers are associated with mental health issues such as anxiety, depression, psychological distress, and fatigue.[29]
Substance abuse
Substance and alcohol abuse can be defined as a pattern of harmful use of substance for mood-altering purposes.[30] Alcohol is one of the most commonly abused substances, and men are up to twice as likely to develop alcoholism than women.[31] Gender differences in alcohol consumption remain universal, although the sizes of gender differences vary.[32] More drinking and heaving, binge drinking occurs in men, whereas more long-term abstention occurs in women.[32] Moreover, men are more likely to abuse substances such as drugs - with a lifetime prevalence of 11.5% in men compared to 6.4% in women - in the United States.[33] Additionally, males are more likely to be substance addicts and abuse substances due to peer pressure compared to females.[33]
Risks
Substance and alcohol abuse disorders are associated with various mental health issues in men and women.[34] Mental health problems are not only a result from drinking too much alcohol, they can also cause people to drink too much.[33] A major reason for consuming alcohol is to change mood or mental state.[35] Alcohol can temporarily alleviate feelings of anxiety and depression and some people use it as a form of ‘self-medication’ in an attempt to counteract these negative feelings.[36] However, alcohol consumption can make existing mental health problems worse.[33] Evidence shows that people who consume high amounts of alcohol or abuse substances are vulnerable to an increased risk of developing mental health problems.[37] Men with mental health disorders, like posttraumatic stress disorder, are twice as likely than women to develop a substance use disorder.[38]
Treatment
There have been identified gender differences in seeking treatment for mental health and substance abuse disorders between men and women.[39] Women are more likely to seek help from and disclose mental health problems to their primary care physicians, whereas men are more likely to seek specialist and inpatient care.[40] Men are more likely than women to disclose problems with alcohol use to their health care provider.[41] In the United States, there are more men than women in treatment for substance use disorders.[41] Both men and women receive better mental health outcomes with early treatment interventions.[42]
Suicide
.png)
Suicide has a high incidence rate in men but often lacks public awareness.[43][44] Suicide is the 13th leading cause of death globally, with a disproportionate number of these deaths being men compared to women.[44][45][46] Despite the fact that women are significantly more likely to attempt suicide than men, men more frequently successfully commit suicide.[45][46] This is known as the gender paradox of suicidal behaviour.[45] The world-wide men to women ratio of age standardized suicide was 1.8 in 2016 according to the World Health Organization.[47] This means that nearly two times as many men as women die due to suicide worldwide. Looking at specific countries, the men to women ratio of suicide can vary, but the overall trend still exists. For example, the suicide rate of men is three times then that of women in the United Kingdom and Australia, and four times that of women in the United States, Russia, and Argentina.[48][49][50][51] In South Africa, the suicide rate amongst men is five times greater than women.[52] In East Asian countries, the gender gap in suicide rates are relatively smaller, with men to women ratios ranging from one to two.[53] Multiple factors exist to explain this gender gap in suicide rates, such as men more frequently completing high mortality actions such as hanging, carbon-monoxide poisoning, and the use of lethal weapons.[54][55] Additional factors that contribute to the disparity in suicide rates between men and women include the pressures of traditional gender roles for men in society and the socialization of men in society.[48][56][57]
Risk factors
Variations exist in the risk factors associated with suicidal behaviour between men and women which contributes to the discrepancy in suicide rates.[45][58][59] Suicide is complex and can not simply be attributed to a single cause, however there are psychological, social, and psychiatric factors to consider.[56][59][60] Mental illness is a major risk factor for suicide for both men and women.[60][61][62] Common mental illnesses that are associated with suicide include depression, bipolar disorder, Schizophrenia, and substance abuse disorders.[61][62][63] In addition to mental illness, psychosocial factors such as unemployment and occupational stress are established risk factors for men.[45][64][65] Alcohol abuse is a risk factor that is much more prevalent in men than in women, which increases risks of depression and impulsive behaviours.[66][67] This problem is exacerbated in men, as they are twice as likely as women to develop alcoholism.[31][68] Reluctance to seek help is another prevalent risk factor facing men, stemming from internalized notions of masculinity.[56][64][69][57] Traditional masculine stereotypes place expectations of strength and stoic, while any indication of vulnerability, such as consulting mental health services, is perceived as weak and emasculating.[56][64][69][57] As a result, depression is under-diagnosed in men and may often remain untreated, which may lead to suicide.[57][70]
Warning signs
Identifying warning signs is important for reducing suicide rates world-wide, but particularly for men, as distress may be expressed in a manner that is not easily recognizable.[54][71][72] For instance, depression, and suicidal thoughts may manifest in the form of anger, hostility, and irritability.[56][71] Additionally, risk-taking and avoidance behaviours may be demonstrated more commonly in men.[56][69]
Common conditions
The following is a list of conditions/diseases that have a high prevalence in men (relative to women).[73]
Cardiovascular conditions:
Respiratory conditions:
Mental health conditions:
- Autism
- Major depressive disorder
- Suicide
- Postpartum depression
- Addiction
Cancer:
Sexual health:
Other:
- Unintentional injuries
- Diabetes
- Influenza
- Liver disease
- Kidney disease
- Alcohol abuse
Organizations
In the UK, the Men's Health Forum was founded in 1994. It was established originally by the Royal College of Nursing but became completely independent of the RCN when it was established as a charity in 2001.[74] The first National Men's Health Week was held in the US in 1994. The first UK week took place in 2002, and the event went international (International Men's Health Week) the following year.[75] In 2005, the world's first professor of men's health, Alan White, was appointed at Leeds Metropolitan University in north-east England.
In Australia, the Men's Health Information and Resource Centre advocates a salutogenic approach to male health which focuses on the causal factors behind health. The Centre is led by John Macdonald and was established in 1999.[76] The Centre leads and executes Men's Health Week in Australia with core funding from the NSW Ministry of Health.
The Global Action on Men's Health (GAMH) was established in 2013 and was registered as a UK-based charity in May 2018. It is a collaborative initiative to bring together men's health organizations from across the globe into a new global network. GAMH is working at international and national levels to encourage international agencies (such as the World Health Organization) and individual governments to develop research, policies and strategies on men's health.[77]
See also
- Andrology
- Gender disparities in health
- International Journal of Men's Health
- International Men's Day November 19
- Movember
- National Prostate Cancer Awareness Month
- Women's health
References
- WHO Definition of Health. "Archived copy". Archived from the original on 2016-07-07. Retrieved 2016-07-06.CS1 maint: archived copy as title (link) Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
- "Men's Health". medlineplus.gov. Retrieved 2019-10-31.
- Almost Every Type of Cancer Kills More Men Than Women, Study Shows http://healthland.time.com/2011/07/13/almost-every-type-of-cancer-kills-more-men-than-women-study-shows Time, 13 July 2011
- Williams DR (2003). "The health of men: structured inequalities and opportunities". Am J Public Health. 93 (5): 724–31. doi:10.2105/ajph.93.5.724. PMC 1447828. PMID 12721133.
- "Men’s Health and Primary Care: Improving Access and Outcomes". http://www.ecoo.info/wp-content/uploads/2013/11/mens-health-and-primary-care-emhf-roundtable-report.2013.medium-res.pdf
- "The State of Men’s Health in Europe". http://ec.europa.eu/health/population_groups/docs/men_health_report_en.pdf ISBN 978-92-79-20167-7 doi:10.2772/60721
- "Gender Statistics Manual". United Nations Statistics Division. May 2015. Retrieved 29 November 2015.
- "Is the US the only country where more men are raped than women?". The Guardian. 21 February 2012. Retrieved 29 November 2015.
- Bardehle D, Dinges M, White A (July 2016). "Was ist Männergesundheit? Eine Definition" (PDF). Gesundheitswesen (Review) (in German). 78 (7): e30–9. doi:10.1055/s-0035-1564077. PMID 26492389.
- "Life Expectancy by Country 2019". World Population Review. Retrieved 31 October 2019.
- "Mars vs. Venus: The gender gap in health". Harvard Medical School. Harvard Health Publishing. Retrieved 31 October 2019.
- "Global Health Observatory data on Life Expectancy". World Health Organization.
- Thornton, Jacqui (5 April 2019). "WHO report shows that women outlive men worldwide". BMJ. 365: l1631. doi:10.1136/bmj.l1631. PMID 30952650.
- Ortiz-Ospina, Esteban; Beltekian, Diana. "Why do women live longer than men?". Our World in Data. Retrieved 31 October 2019.
- Baker, Peter; Dworkin, Shari L; Tong, Sengfah; Banks, Ian; Shand, Tim; Yamey, Gavin (March 6, 2014). "The men's health gap: men must be included in the global health equity agenda". Bulletin of the World Health Organization. 92 (8): 618–620. doi:10.2471/BLT.13.132795. PMC 4147416. PMID 25197149. Retrieved 31 October 2019.
- "Testosterone — What It Does And Doesn't Do". Harvard Medical School. Harvard Health Publishing. Retrieved 31 October 2019.
- Morris, Paul D; Channer, Kevin S (23 April 2012). "Testosterone and cardiovascular disease in men". Asian Journal of Andrology. 14 (3): 428–435. doi:10.1038/aja.2012.21. PMC 3720171. PMID 22522504.
- "World Health Report 2014" (PDF). World Health Organization. Retrieved 31 October 2019.
- Courtenay, W. H. (2000). "Constructions of masculinity and their influence on men's well-being: a theory of gender and health". Social Science & Medicine (1982). 50 (10): 1385–1401. doi:10.1016/s0277-9536(99)00390-1. ISSN 0277-9536. PMID 10741575.
- Williams, David R. (May 2003). "The Health of Men: Structured Inequalities and Opportunities". American Journal of Public Health. 93 (5): 724–731. doi:10.2105/ajph.93.5.724. PMC 1447828. PMID 12721133.
- Freeman, Aislinné; Mergl, Roland; Kohls, Elisabeth; Székely, András; Gusmao, Ricardo; Arensman, Ella; Koburger, Nicole; Hegerl, Ulrich; Rummel-Kluge, Christine (29 June 2017). "A cross-national study on gender differences in suicide intent". BMC Psychiatry. 17 (1): 234. doi:10.1186/s12888-017-1398-8. PMC 5492308. PMID 28662694.
- Moore, Fhionna; Taylor, Shanice; Beaumont, Joanna; Gibson, Rachel; Starkey, Charlotte; DeLuca, Vincenzo (23 August 2018). "The gender suicide paradox under gender role reversal during industrialisation". PLOS ONE. 13 (8): e0202487. Bibcode:2018PLoSO..1302487M. doi:10.1371/journal.pone.0202487. PMC 6107173. PMID 30138465.
- Miranda-Mendizabal, Andrea; Castellví, Pere; Parés-Badell, Oleguer; Alayo, Itxaso; Almenara, José; Alonso, Iciar; Blasco, Maria Jesús; Cebrià, Annabel; Gabilondo, Andrea; Gili, Margalida; Lagares, Carolina; Piqueras, José Antonio; Rodríguez-Jiménez, Tiscar; Rodríguez-Marín, Jesús; Roca, Miquel; Soto-Sanz, Victoria; Vilagut, Gemma; Alonso, Jordi (12 January 2019). "Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies". International Journal of Public Health. 64 (2): 265–283. doi:10.1007/s00038-018-1196-1. PMC 6439147. PMID 30635683.
- "Gender and Stress". American Psychological Association. Retrieved 2019-11-22.
- Schneider, Robert H.; Alexander, Charles N.; Staggers, Frank; Rainforth, Maxwell; Salerno, John W.; Hartz, Arthur; Arndt, Stephen; Barnes, Vernon A.; Nidich, Sanford I. (2005). "Long-Term Effects of Stress Reduction on Mortality in Persons ≥55 Years of Age With Systemic Hypertension". The American Journal of Cardiology. 95 (9): 1060–1064. doi:10.1016/j.amjcard.2004.12.058. ISSN 0002-9149. PMC 1482831. PMID 15842971.
- Oettgen, Peter. "Cardiovascular Disease Possible Risk Factors". DynaMed.
- "Erectile dysfunction (impotence)". Evidence-Based Medicine Guidelines. Nov 30, 2018.
- Rove, Kyle. "Infertility in Men". DynaMed.
- Philpott, Lloyd Frank; Leahy-Warren, Patricia; FitzGerald, Serena; Savage, Eileen (2017). "Stress in fathers in the perinatal period: A systematic review". Midwifery. 55: 113–127. doi:10.1016/j.midw.2017.09.016. ISSN 1532-3099. PMID 28992554.
- "WHO | Substance abuse". WHO. Retrieved 2019-11-22.
- "CDC - Fact Sheets-Excessive Alcohol Use and Risks to Men's Health - Alcohol". www.cdc.gov. 2018-09-18. Retrieved 2019-11-22.
- Wilsnack, Richard W.; Wilsnack, Sharon C.; Kristjanson, Arlinda F.; Vogeltanz-Holm, Nancy D.; Gmel, Gerhard (September 2009). "Gender and alcohol consumption: Patterns from the multinational GENACIS project". Addiction (Abingdon, England). 104 (9): 1487–1500. doi:10.1111/j.1360-0443.2009.02696.x. ISSN 0965-2140. PMC 2844334. PMID 19686518.
- "The Differences in Addiction Between Men and Women - Addiction Center". AddictionCenter. Retrieved 2019-11-22.
- Melinda (2018-11-02). "Substance Abuse and Mental Health Issues - HelpGuide.org". https://www.helpguide.org. Retrieved 2019-11-22. External link in
|website=(help) - ABBEY, ANTONIA; SMITH, MARY JO; SCOTT, RICHARD O. (1993). "The relationship between reasons for drinking alcohol and alcohol consumption: An interactional approach". Addictive Behaviors. 18 (6): 659–670. doi:10.1016/0306-4603(93)90019-6. ISSN 0306-4603. PMC 4493891. PMID 8178704.
- Crum, Rosa M.; Mojtabai, Ramin; Lazareck, Samuel; Bolton, James M.; Robinson, Jennifer; Sareen, Jitender; Green, Kerry M.; Stuart, Elizabeth A.; Flair, Lareina La; Alvanzo, Anika A. H.; Storr, Carla L. (2013-07-01). "A Prospective Assessment of Reports of Drinking to Self-medicate Mood Symptoms With the Incidence and Persistence of Alcohol Dependence". JAMA Psychiatry. 70 (7): 718–726. doi:10.1001/jamapsychiatry.2013.1098. ISSN 2168-622X. PMC 4151472. PMID 23636710.
- Monahan, John; Steadman, Henry J. (1996-05-15). Violence and Mental Disorder: Developments in Risk Assessment. University of Chicago Press. ISBN 978-0-226-53406-0.
- "Men More Likely Than Women to Face Substance Use Disorders and Mental Illness". pew.org. Retrieved 2019-11-22.
- Abuse, National Institute on Drug. "Sex and Gender Differences in Substance Use Disorder Treatment". www.drugabuse.gov. Retrieved 2019-11-22.
- "WHO | Gender and women's mental health". WHO. Retrieved 2019-11-22.
- "NIAAA Publications". pubs.niaaa.nih.gov. Retrieved 2019-11-22.
- Administration (US), Substance Abuse and Mental Health Services; General (US), Office of the Surgeon (November 2016). EARLY INTERVENTION, TREATMENT, AND MANAGEMENT OF SUBSTANCE USE DISORDERS. US Department of Health and Human Services.
- "The silent epidemic of male suicide | British Columbia Medical Journal". www.bcmj.org. Retrieved 2019-11-22.
- Ritchie, Hannah; Roser, Max; Ortiz-Ospina, Esteban (2015-06-15). "Suicide". Our World in Data.
- Freeman, Aislinné; Mergl, Roland; Kohls, Elisabeth; Székely, András; Gusmao, Ricardo; Arensman, Ella; Koburger, Nicole; Hegerl, Ulrich; Rummel-Kluge, Christine (2017). "A cross-national study on gender differences in suicide intent". BMC Psychiatry. 17 (1): 234. doi:10.1186/s12888-017-1398-8. ISSN 1471-244X. PMC 5492308. PMID 28662694.
- "UpToDate". www.uptodate.com. Retrieved 2019-11-22.
- "WHO | Suicide rates (per 100 000 population)". WHO. Retrieved 2019-11-22.
- "Men: A Different Depression". American Psychological Association. Retrieved 2019-11-22.
- "Suicides in the UK - Office for National Statistics". www.ons.gov.uk. Retrieved 2019-11-22.
- "Male:Female ratio of age-standardized suicide rates". World Health Organization. 2016.
- World Health Organization. Preventing suicide: A global imperative. Geneva: World Health Organization; 2014. 1–88 p.
- "#5facts: The sad extent of suicide in South Africa". Africa Check. Retrieved 2019-11-22.
- Chen, Ying-Yeh; Chen, Mengni; Lui, Carrie S. M.; Yip, Paul S. F. (2017). "Female labour force participation and suicide rates in the world". Social Science & Medicine. 195: 61–67. doi:10.1016/j.socscimed.2017.11.014. ISSN 0277-9536. PMID 29154181.
- Hunt, Tara; Wilson, Coralie J.; Caputi, Peter; Woodward, Alan; Wilson, Ian (2017-03-29). Voracek, Martin (ed.). "Signs of current suicidality in men: A systematic review". PLOS ONE. 12 (3): e0174675. Bibcode:2017PLoSO..1274675H. doi:10.1371/journal.pone.0174675. ISSN 1932-6203. PMC 5371342. PMID 28355268.
- Beautrais, Annette L. (2002). "Gender issues in youth suicidal behaviour". Emergency Medicine (Fremantle, W.A.). 14 (1): 35–42. doi:10.1046/j.1442-2026.2002.00283.x. ISSN 1035-6851. PMID 11993833.
- "Men and Suicide". Centre for Suicide Prevention. Retrieved 2019-11-22.
- Seidler, Zac E.; Dawes, Alexei J.; Rice, Simon M.; Oliffe, John L.; Dhillon, Haryana M. (2016). "The role of masculinity in men's help-seeking for depression: A systematic review". Clinical Psychology Review. 49: 106–118. doi:10.1016/j.cpr.2016.09.002. ISSN 0272-7358. PMID 27664823.
- Ibrahim, Norhayati; Amit, Noh; Din, Normah Che; Ong, Hui Chien (2017-04-28). "Gender differences and psychological factors associated with suicidal ideation among youth in Malaysia". Psychology Research and Behavior Management. 10: 129–135. doi:10.2147/prbm.s125176. PMC 5417667. PMID 28496374.
- Donker, Tara; Batterham, Philip J; Van Orden, Kimberly A; Christensen, Helen (2014). "Gender-differences in risk factors for suicidal behaviour identified by perceived burdensomeness, thwarted belongingness and acquired capability: cross-sectional analysis from a longitudinal cohort study". BMC Psychology. 2 (1): 20. doi:10.1186/2050-7283-2-20. ISSN 2050-7283. PMC 4363058. PMID 25815191.
- Platt, Stephen (2017). "Suicide in men: what is the problem?". Trends in Urology & Men's Health. 8 (4): 9–12. doi:10.1002/tre.587. ISSN 2044-3749.
- Brådvik, Louise (2018-09-17). "Suicide Risk and Mental Disorders". International Journal of Environmental Research and Public Health. 15 (9): 2028. doi:10.3390/ijerph15092028. ISSN 1660-4601. PMC 6165520. PMID 30227658.
- Too, Lay San; Spittal, Matthew J.; Bugeja, Lyndal; Reifels, Lennart; Butterworth, Peter; Pirkis, Jane (2019). "The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies". Journal of Affective Disorders. 259: 302–313. doi:10.1016/j.jad.2019.08.054. ISSN 0165-0327. PMID 31450139.
- Breet, Elsie; Goldstone, Daniel; Bantjes, Jason (2018). "Substance use and suicidal ideation and behaviour in low- and middle-income countries: a systematic review". BMC Public Health. 18 (1): 549. doi:10.1186/s12889-018-5425-6. ISSN 1471-2458. PMC 5921303. PMID 29699529.
- Boettcher, Nick; Mitchell, Jennifer; Lashewicz, Bonnie; Jones, Erin; Wang, JianLi; Gundu, Sarika; Marchand, Alain; Michalak, Erin; Lam, Ray (2019). "Men's Work-Related Stress and Mental Health: Illustrating the Workings of Masculine Role Norms". American Journal of Men's Health. 13 (2): 155798831983841. doi:10.1177/1557988319838416. ISSN 1557-9883. PMC 6438430. PMID 30880590.
- "The Effect of Unemployment on Suicide Risk" (PDF). US department of veteran affairs.
- Gilman, Stephen E; Abraham, Henry David (2001). "A longitudinal study of the order of onset of alcohol dependence and major depression". Drug and Alcohol Dependence. 63 (3): 277–286. doi:10.1016/S0376-8716(00)00216-7. ISSN 0376-8716. PMID 11418232.
- Norström, Thor; Rossow, Ingeborg (2016). "Alcohol Consumption as a Risk Factor for Suicidal Behavior: A Systematic Review of Associations at the Individual and at the Population Level". Archives of Suicide Research. 20 (4): 489–506. doi:10.1080/13811118.2016.1158678. hdl:11250/2387826. ISSN 1381-1118. PMID 26953621.
- "Why Are Men More Susceptible to Alcoholism?". www.elsevier.com. Retrieved 2019-11-22.
- Goyne, Anne (2018). "Suicide, male honour and the masculinity paradox: its impact on the ADF" (PDF). Australian Defence Force Journal.
- Call, Jarrod B.; Shafer, Kevin (2018). "Gendered Manifestations of Depression and Help Seeking Among Men". American Journal of Men's Health. 12 (1): 41–51. doi:10.1177/1557988315623993. ISSN 1557-9883. PMC 5734537. PMID 26721265.
- Rochlen, Aaron B.; Paterniti, Debora A.; Epstein, Ronald M.; Duberstein, Paul; Willeford, Lindsay; Kravitz, Richard L. (2010). "Barriers in Diagnosing and Treating Men With Depression: A Focus Group Report". American Journal of Men's Health. 4 (2): 167–175. doi:10.1177/1557988309335823. ISSN 1557-9883. PMC 3140791. PMID 19477750.
- Kilmartin, Christopher (2005). "Depression in men: communication, diagnosis and therapy". The Journal of Men's Health & Gender. 2 (1): 95–99. doi:10.1016/j.jmhg.2004.10.010. ISSN 1571-8913.
- "20 Diseases That Affect Men More Than Women". Best Life. October 12, 2018.
- "More About Us". Men's Health Forum. Retrieved Oct 29, 2019.
- "Men's Health Week". GLOBAL ACTION ON MEN’S HEALTH. 2014-05-26. Retrieved 2019-10-29.
- Macken, University of Western Sydney-Michael. "Men's Health Information and Resource Centre". www.westernsydney.edu.au. Retrieved 2019-10-29.
- "About Us". GLOBAL ACTION ON MEN’S HEALTH. Retrieved 2019-10-29.
External links
| Wikimedia Commons has media related to Men's health. |