Measles vaccine
Measles vaccine is a vaccine that prevents measles.[1] Nearly all of those who do not develop immunity after a single dose develop it after a second dose.[1] When rates of vaccination within a population are greater than 92% outbreaks of measles typically no longer occur; however, they may occur again if rates of vaccination decrease.[1] The vaccine's effectiveness lasts many years.[1] It is unclear if it becomes less effective over time.[1] The vaccine may also protect against measles if given within a couple of days after exposure to measles.[1]
.jpg) A child is given a measles vaccine. | |
| Vaccine description | |
|---|---|
| Target disease | Measles |
| Type | Attenuated virus |
| Clinical data | |
| MedlinePlus | a601176 |
| ATC code | |
| Identifiers | |
| ChemSpider |
|
| | |
The vaccine is generally safe, even for those with HIV infections.[1] Side effects are usually mild and short lived.[1] These may include pain at the site of injection or mild fever.[1] Anaphylaxis has been documented in about 3.5–10 cases per million doses.[1] Rates of Guillain–Barré syndrome, autism and inflammatory bowel disease do not appear to be increased by measles vaccination.[1]
The vaccine is available both by itself and in combinations such as the MMR vaccine (a combination with the rubella vaccine and mumps vaccine)[1] or the MMRV vaccine (a combination of MMR with the chickenpox vaccine).[2] The measles vaccine is equally effective for preventing measles in all formulations, but side effects vary depending with the combination.[1][3] The World Health Organization (WHO) recommends measles vaccine be given at nine months of age in areas of the world where the disease is common, or at twelve months where the disease is not common.[1] Measles vaccine is based on a live but weakened strain of measles.[1] It comes as a dried powder which is mixed with a specific liquid before being injected either just under the skin or into a muscle.[1] Verification that the vaccine was effective can be determined by blood tests.[1]
About 85% of children globally have received this vaccine as of 2013.[4] In 2015, at least 160 countries provided two doses in their routine immunization.[5] The measles vaccine was first introduced in 1963.[6] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[7] The wholesale cost in the developing world is about 0.70 USD per dose as of 2014.[8] As outbreaks easily occur in under-vaccinated populations, the disease is seen as a test of sufficient vaccination within a population.[9]
Medical uses
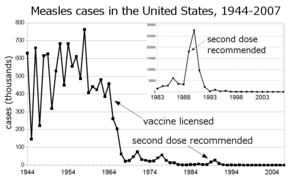
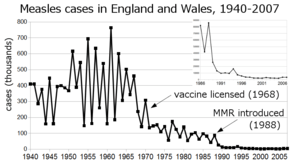
Before the widespread use of the vaccine, measles was so common that infection was considered "as inevitable as death and taxes."[10] In the United States, reported cases of measles fell from hundreds of thousands to tens of thousands per year following introduction of the vaccine in 1963 (see chart at right). Increasing uptake of the vaccine following outbreaks in 1971 and 1977 brought this down to thousands of cases per year in the 1980s. An outbreak of almost 30,000 cases in 1990 led to a renewed push for vaccination and the addition of a second vaccine to the recommended schedule. No more than 220 cases were reported in any year from 1997 to 2013, and the disease was believed no longer endemic in the United States.[11][12][13] In 2014, 667 cases were reported.[14]
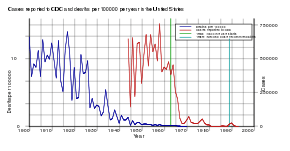
The benefit of measles vaccination in preventing illness, disability, and death have been well documented. Within the first 20 years of being licensed in the U.S., measles vaccination prevented an estimated 52 million cases of the disease, 17,400 cases of mental retardation, and 5,200 deaths.[15] During 1999–2004, a strategy led by the World Health Organization (WHO) and UNICEF led to improvements in measles vaccination coverage that averted an estimated 1.4 million measles deaths worldwide.[16] The vaccine for measles has led to the near-complete elimination of the disease in the United States and other developed countries.[17] While the vaccine is made with a live virus which can cause side effects, these are far fewer and less serious than the sickness and death caused by measles itself, side effects ranging from rashes to, rarely, convulsions, occur in a small percentage of recipients.[18]
Measles is common worldwide. Although it was declared eliminated from the U.S. in 2000, high rates of vaccination and excellent communication with those who refuse vaccination are needed to prevent outbreaks and sustain the elimination of measles in the U.S.[19] Of the 66 cases of measles reported in the U.S. in 2005, slightly over half were attributable to one unvaccinated individual who acquired measles during a visit to Romania.[20] This individual returned to a community with many unvaccinated children. The resulting outbreak infected 34 people, mostly children and virtually all unvaccinated; 9% were hospitalized, and the cost of containing the outbreak was estimated at $167,685. A major epidemic was averted due to high rates of vaccination in the surrounding communities.[19]
The vaccine has non specific effects such as preventing respiratory infections, that may be greater than those of measles prevention alone. These benefits are greater when the vaccine is given before one year of age. A high titre vaccine resulted in worse outcomes in girls and thus is not recommended by the World Health Organization.[21]
Schedule
The World Health Organization (WHO) recommends two doses of vaccine for all children.[1] In countries with high risk of disease the first dose should be given around nine months of age.[1] Otherwise it can be given at twelve months of age.[1] The second dose should be given at least one month after the first dose.[1] This is often done at age 15 to 18 months.[1] After one dose at the age of nine months 85% are immune, while a dose at twelve months results in 95% immunity.[6]
In the United States, the Centers for Disease Control and Prevention (CDC) recommends that children aged 6 to 12 months traveling outside the United States receive their first dose of MMR vaccine.[22] Otherwise the first dose is typically given between 12–18 months. A second dose is given by 7 years (on or before last day of year 6) or by kindergarten entry.[23]
In the UK, the National Health Service (NHS) recommendation is for a first dose at around 13 months of age and the second at three years and four months old.[24]
In Canada, Health Canada recommends that children travelling outside North America should receive an MMR vaccine if they are aged 6 to 12 months. However, after the child is 12 months old they should receive 2 additional doses to ensure long-lasting protection.[25]
Adverse effects
Adverse effects associated with the MMR vaccine include fever, rash, injection site pain and, in rare cases, red or purple discolorations on the skin known as thrombocytopenic purpura, or seizures related to fever (febrile seizure).[26][27]
Numerous studies have found no relationship between MMR vaccine and autism.[28][29][30][27]
History
As a fellow at Children's Hospital Boston, Thomas C. Peebles worked with John Franklin Enders. Enders became known as "The Father of Modern vaccines", and Enders shared the Nobel Prize in 1954 for his research on cultivating the polio virus that led to the development of a vaccination for the disease. Switching to study measles, Enders sent Peebles to Fay School in Massachusetts, where an outbreak of the disease was under way, and there Peebles was able to isolate the virus from some of the blood samples and throat swabs he had taken from the students. Even after Enders had taken him off the study team, Peebles was able to cultivate the virus and show that the disease could be passed on to monkeys inoculated with the material he had collected.[17] Enders was able to use the cultivated virus to develop a measles vaccine in 1963 based on the material isolated by Peebles.[33] In the late 1950s and early 1960s, nearly twice as many children died from measles as from polio.[34] The vaccine Enders developed was based on the Edmonston strain of attenuated live measles virus, which was named for the Fay student from whom Peebles had taken the culture that led to the virus's cultivation.[35]
In the mid-20th century, measles was particularly devastating in West Africa, where child mortality rates were 50 percent before age 5, and the children were struck with the type of rash and other symptoms common prior to 1900 in England and other countries. The first trial of a live attenuated measles vaccine was undertaken in 1960 by the British paediatrician David Morley in a village near Ilesha, Nigeria; in case he could be accused of exploiting the Nigerian population, Morley included his own four children in the study. The encouraging results led to a second study of about 450 children in the village and at the Wesley Guild Hospital in Ilesha. Following another epidemic, a larger trial was undertaken in September and October 1962, in New York City with the assistance of the World Health Organization (WHO): 131 children received the live Enders attenuated Edmonston B strain plus gamma globulin, 130 children received a "further attenuated" vaccine without gamma globulin, and 173 children acted as control subjects for both groups. As also shown in the Nigerian trial, the trial confirmed that the "further attenuated" vaccine was superior to the Edmonston B vaccine, and caused significantly fewer instances of fever and diarrhea. The successful results led to 2,000 children in the area being vaccinated.[36][37]
Maurice Hilleman at Merck & Co., a pioneer in the development of vaccinations, developed the MMR vaccine in 1971, which vaccinates against measles, mumps and rubella in a single shot followed by a booster.[18][38] One form is called "Attenuvax".[39] The measles component of the MMR vaccine uses Attenuvax, which is grown in a chick embryo cell culture using the Enders' attenuated Edmonston strain. Merck decided not to resume production of Attenuvax on October 21, 2009.[40]</ref>
Types

Measles is seldom given as an individual vaccine and is often given in combination with rubella, mumps, or varicella (chickenpox) vaccines. Below is the list of measles-containing vaccines:
- Measles vaccine (standalone vaccine)
- Measles rubella vaccine (MR vaccine)
- Mumps measles rubella vaccine, live (MMR vaccine)
- Mumps measles rubella and varicella virus vaccine (MMRV vaccine)
References
- "Measles vaccines: WHO position paper – April 2017" (PDF). Weekly Epidemiological Record. 92 (17): 205–27. April 2017. hdl:10665/255149. PMID 28459148.
- Mitchell D (2013). The essential guide to children's vaccines. New York: St. Martin's Press. p. 127. ISBN 9781466827509. Archived from the original on 9 September 2017.
- "Information Sheet Observed Rate of Vaccine Reactions" (PDF). World Health Organization (WHO). Retrieved 1 December 2018.
- "Measles Fact sheet N°286". World Health Organization (WHO). November 2014. Archived from the original on 3 February 2015. Retrieved 4 February 2015.
- "Immunization coverage". World Health Organization (WHO). Archived from the original on 13 July 2017. Retrieved 12 July 2017.
- Centers for Disease Control and Prevention (2014). CDC health information for international travel 2014 the yellow book. p. 250. ISBN 9780199948505. Archived from the original on 9 September 2017.
- "World Health Organization model list of essential medicines: 21st list 2019". World Health Organization. 2019. hdl:10665/325771. Cite journal requires
|journal=(help) - "Vaccine, Measles". International Drug Price Indicator Guide. Retrieved 6 December 2015.
- Abramson B (2018). Vaccine, vaccination, and immunization law. Bloomberg Law. pp. 10–30. ISBN 9781682675830.
- Babbott FL, Gordon JE (September 1954). "Modern measles". The American Journal of the Medical Sciences. 228 (3): 334–61. doi:10.1097/00000441-195409000-00013. PMID 13197385.
- Centers for Disease Control and Prevention (CDC) (1994). "Summary of notifiable diseases, United States, 1993". MMWR. Morbidity and Mortality Weekly Report. 42 (53): i–xvii, 1–73. PMID 9247368.
- Centers for Disease Control and Prevention (CDC) (July 2007). "Summary of notifiable diseases, United States, 2007". MMWR. Morbidity and Mortality Weekly Report. 56 (53): 1–94.
- Wallace G, Leroy Z (2015). "Measles". In Hamborsky J, Kroger A, Wolfe S (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases (13th ed.). Washington D.C.: Public Health Foundation.
- "Measles Cases and Outbreaks". Archived from the original on 13 February 2015. Retrieved 30 November 2018.
- Bloch AB, Orenstein WA, Stetler HC, Wassilak SG, Amler RW, Bart KJ, Kirby CD, Hinman AR (October 1985). "Health impact of measles vaccination in the United States". Pediatrics. 76 (4): 524–32. PMID 3931045.
- Centers for Disease Control and Prevention (CDC) (March 2006). "Progress in reducing global measles deaths, 1999-2004". MMWR. Morbidity and Mortality Weekly Report. 55 (9): 247–9. PMID 16528234. Archived from the original on 16 October 2007.
- Douglas M (4 August 2010). "Dr. Thomas C. Peebles, Who Identified Measles Virus, Dies at 89". The New York Times.
- Collins H (30 August 1999). "The Man Who Saved Your Life - Maurice R. Hilleman - Developer of Vaccines for Mumps and Pandemic Flu: Maurice Hilleman's Vaccines Prevent Millions of Deaths Every Year". The Philadelphia Inquirer.
- Parker AA, Staggs W, Dayan GH, Ortega-Sánchez IR, Rota PA, Lowe L, Boardman P, Teclaw R, Graves C, LeBaron CW (August 2006). "Implications of a 2005 measles outbreak in Indiana for sustained elimination of measles in the United States". The New England Journal of Medicine. 355 (5): 447–55. doi:10.1056/NEJMoa060775. PMID 16885548.
- Centers for Disease Control and Prevention (CDC) (December 2006). "Measles--United States, 2005". MMWR. Morbidity and Mortality Weekly Report. 55 (50): 1348–51. PMID 17183226. Archived from the original on 13 March 2015.
- Sankoh O, Welaga P, Debpuur C, Zandoh C, Gyaase S, Poma MA, Mutua MK, Hanifi SM, Martins C, Nebie E, Kagoné M, Emina JB, Aaby P (June 2014). "The non-specific effects of vaccines and other childhood interventions: the contribution of INDEPTH Health and Demographic Surveillance Systems". International Journal of Epidemiology. 43 (3): 645–53. doi:10.1093/ije/dyu101. PMC 4052142. PMID 24920644.
- "Measles and the Vaccine (Shot) to Prevent It". Centers for Disease Control. Archived from the original on 20 January 2015. Retrieved 24 January 2015.
- Washington Stat Dept of Health
- "Measles". National Health Service UK. 20 October 2017. Retrieved 11 March 2019.
- "Measles vaccine: Canadian immunization guide". Public Health Agency of Canada. 18 July 2007. Retrieved 13 March 2019.
- "Information Sheet: Observed Rate of Vaccine Reactions: Measles, Mumps and Rubella Vaccines" (PDF). World Health Organization (WHO). May 2014.
- Demicheli V, Rivetti A, Debalini MG, Di Pietrantonj C (February 2012). "Vaccines for measles, mumps and rubella in children". Cochrane Database Syst Rev (2). doi:10.1002/14651858.CD004407.pub3. PMC 6458016. PMID 22336803. CD004407.
- "Measles, Mumps, and Rubella Vaccine". Adverse Effects of Vaccines: Evidence and Causality. Washington, D.C.: The National Academies Press. 9 April 2012. ISBN 978-0-309-21436-0.
- "Measles, mumps, and rubella (MMR) vaccine". Centers for Disease Control and Prevention. 22 August 2008. Archived from the original on 9 October 2008. Retrieved 21 December 2008.
- Immunization Safety Review: Vaccines and Autism. Institute of Medicine of the National Academy of Sciences. 17 May 2004. doi:10.17226/10997. ISBN 978-0-309-09237-1.
- "Guidelines for Vaccinating Pregnant Women". Centers for Disease Control and Prevention. U.S. Department of Health & Human Services. August 2016.
- "Contraindications and Precautions". Vaccine Recommendations and Guidelines of the ACIP. Centers for Disease Control and Prevention. U.S. Department of Health & Human Services.
- "Work by Enders Brings Measles Vaccine License". The Hartford Courant. 22 March 1963. Archived from the original on 3 November 2012.
A strain of measles virus isolated in 1954 by Dr. Thomas C. Peebles, instructor in pediatrics at Harvard, and Enders, formed the basis for the development of the present vaccine
- "The Measles Vaccine". The New York Times. 28 March 1963.
- Hilleman MR (July 1992). "Past, present, and future of measles, mumps, and rubella virus vaccines". Pediatrics. 90 (1 Pt 2): 149–53. PMID 1603640.
- Morley DC, Woodland M, Krugman S, Friedman H, Grab B (1964). "Measles and Measles Vaccination in an African Village". Bulletin of the World Health Organization. 30: 733–9. PMC 2554995. PMID 14196817.
- Pritchard J (13 November 1997). "Obituary: Dr C. A. Pearson". The Independent. Archived from the original on 24 February 2014. Retrieved 29 January 2014.
- Sullivan P (13 April 2005). "Maurice R. Hilleman Dies; Created Vaccines (washingtonpost.com)". The Washington Post. Archived from the original on 20 October 2012. Retrieved 21 July 2009.
- Ovsyannikova IG, Johnson KL, Naylor S, Poland GA (February 2005). "Identification of HLA-DRB1-bound self-peptides following measles virus infection". Journal of Immunological Methods. 297 (1–2): 153–67. doi:10.1016/j.jim.2004.12.020. PMID 15777939.
- "Q&As about Monovalent M-M-R Vaccines". Centers for Disease Control and Prevention (CDC). 26 October 2009. Archived from the original on 19 October 2019. Retrieved 18 October 2019.