Luteal phase
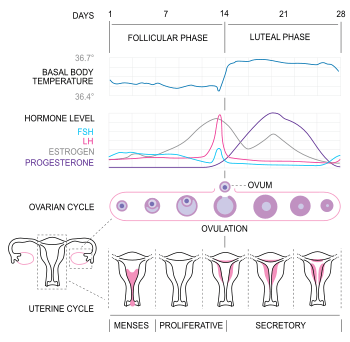
The luteal phase is the latter phase of the menstrual cycle (in humans and a few other animals) or the earlier phase of the estrous cycle (in other placental mammals). It begins with the formation of the corpus luteum and ends in either pregnancy or luteolysis. The main hormone associated with this stage is progesterone, which is significantly higher during the luteal phase than other phases of the cycle.[1] Another is the endocannabinoid anandamide AEA, where the lowest plasma AEA level is observed in the luteal phase.[2] The opposite of the luteal phase, the rest of the two weeks, is called the follicular phase.
Hormonal events
After ovulation, the pituitary hormones–FSH and LH released from the anterior pituitary cause the remaining parts of the dominant follicle to transform into the corpus luteum. It continues to grow for some time after ovulation and produces significant amounts of hormones, particularly progesterone,[3] and, to a lesser extent, estrogen. Progesterone plays a vital role in making the endometrium receptive to implantation of the blastocyst and supportive of the early pregnancy; it also has the side effect of raising the woman's basal body temperature.[4]
Several days after ovulation, the increasing amount of estrogen produced by the corpus luteum may cause one or two days of fertile cervical mucus, lower basal body temperatures, or both. This is known as a "secondary estrogen surge".[5]
The hormones produced by the corpus luteum also suppress production of the FSH and LH that the corpus luteum needs to maintain itself. With continued low levels of FSH and LH, the corpus luteum will atrophy.[3] The death of the corpus luteum results in falling levels of progesterone and estrogen. These falling levels of ovarian hormones cause increased levels of FSH, which begins recruiting follicles for the next cycle. Continued drops in levels of estrogen and progesterone trigger the end of the luteal phase: menstruation and the beginning of the next cycle.[4]
The human luteal phase lasts between ten and sixteen days, the average being fourteen days. Luteal phases of less than twelve days may make it more difficult to achieve pregnancy. While luteal phase length varies significantly from woman to woman, for the same woman the length will be fairly consistent from cycle to cycle.[6]
The loss of the corpus luteum can be prevented by implantation of an embryo: after implantation, human embryos produce human chorionic gonadotropin (hCG),[7] which is structurally similar to LH and can preserve the corpus luteum.[3] Because the hormone is unique to the embryo, most pregnancy tests look for the presence of hCG.[3] If implantation occurs, the corpus luteum will continue to produce progesterone (and maintain high basal body temperatures) for eight to twelve weeks, after which the placenta takes over this function.[8]
Luteal phase defect
Luteal phase defect (LPD), or luteal insufficiency, occurs when the luteal phase is shorter than normal, progesterone levels during the luteal phase are below normal, or both. LPD is believed to interfere with the implantation of embryos. The lactational amenorrhea method of birth control works primarily by preventing ovulation, but is also known to cause LPD.[9]
For diagnosis of LPD, the main methods are:
- An endometrial biopsy, preferably on the 12th day when there is an expected 14 day luteal phase.[10]
- Vaginal ultrasonography, to detect abnormalities in folliculogenesis.[10]
The characteristics of the rise in basal body temperature after ovulation is not helpful in the diagnosis of luteal phase defect, but there is a high likelihood of luteal phase defect if it lasts less than 11 days.[11] A single progesterone test is unreliable because of high variability across the day, and multiple tests are expensive and inconvenient.[10]
LPD is a spectrum. There is unruptured luteinized follicle syndrome (ULFS), short luteal phases that are, for example, nine days long, and follicular non-responsiveness to hCG. The second two varieties can be stabilized by taking high-dose progesterone suppositories or injections until one gets a positive pregnancy test, and then continuing for another 8–10 weeks until the placenta is self-sufficient. Some people have seen normalization with a high dose of vitamin B6.
ULFS can be treated by a high dose of hCG at ovulation, or by IVF.
References
- Bagnell, C. 2005. "Animal Reproduction". Rutgers University Department of Animal Sciences.
- Cui N, Wang L, Wang W, Zhang J, Xu Y, Jiang L, Hao G (November 2017). "The correlation of anandamide with gonadotrophin and sex steroid hormones during the menstrual cycle". Iranian Journal of Basic Medical Sciences. 20 (11): 1268–1274. doi:10.22038/IJBMS.2017.9488. PMC 5749362. PMID 29299205.
- Losos JB, Raven PH, Johnson GB, Singer SR (2002). Biology. New York: McGraw-Hill. pp. 1207–09. ISBN 0-07-303120-8.
- Weschler T (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 361–2. ISBN 0-06-093764-5.
- Weschler 2002, pp. 310,326
- Marieb, Elaine (2013). Anatomy & physiology. Benjamin-Cummings. p. 915. ISBN 9780321887603.
- Wilcox AJ, Baird DD, Weinberg CR (June 1999). "Time of implantation of the conceptus and loss of pregnancy". The New England Journal of Medicine. 340 (23): 1796–9. doi:10.1056/NEJM199906103402304. PMID 10362823.
- Glade B. Curtis (1999). "Week 4". Your Pregnancy Week by Week. Element Books. ISBN 1-86204-396-5.
- Díaz S, Cárdenas H, Brandeis A, Miranda P, Salvatierra AM, Croxatto HB (September 1992). "Relative contributions of anovulation and luteal phase defect to the reduced pregnancy rate of breastfeeding women". Fertility and Sterility. 58 (3): 498–503. PMID 1521642.
- Alderson TL (2016-12-09). "Luteal Phase Dysfunction Workup". Medscape.
- Downs KA, Gibson M (October 1983). "Basal body temperature graph and the luteal phase defect". Fertility and Sterility. 40 (4): 466–8. PMID 6617904.