Sural nerve
The sural nerve is a sensory nerve in the calf region (sura) of the leg. It is made up of branches of the tibial nerve and common fibular nerve, the medial cutaneous branch from the tibial nerve, and the lateral cutaneous branch from the common fibular nerve. Once formed, the nerves runs down the mid calf to the ankle and along the skin from the mid-posterior popliteal fossa to just behind to the lateral malleolus and then under the malleolus and forward along the lateral aspect of the foot.
| Sural nerve | |
|---|---|
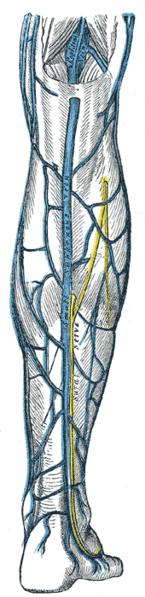 The small saphenous vein (sural nerve visible running vertically) | |
| Details | |
| From | Medial sural cutaneous nerve, communicating branch with the common fibular nerve (S1, S2) |
| Innervates | Supplies sensation to the skin of the lateral foot and lateral lower ankle. |
| Identifiers | |
| Latin | nervus suralis |
| MeSH | D013497 |
| TA | A14.2.07.062 |
| FMA | 44688 |
| Anatomical terms of neuroanatomy | |
The sural nerve supplies sensation to the skin of the lateral foot and lateral lower ankle.[1]
Structure
The sural cutaneous nerve consists of the fusion of the medial sural cutaneous nerve (MSCN) which is a terminal branch of the tibial nerve and the lateral sural cutaneous nerve (LSCN) which is one of the terminal branches of the common fibular nerve. These two branches, MSCN and LSCN, are connected by the sural communicating branch and form the sural nerve. How the two branches fuse, the contribution of the fibular and tibial branch, the location of the connection, and differences between the two lower extremities contribute to variability of this nerve.
The tibial nerve and the common fibular nerve arise as the sciatic nerve divides into two branches in the popliteal fossa. As the tibial nerve travels down the popliteal fossa, and before it goes beneath the gastrocnemius, it gives off a cutaneous branch which is the medial sural cutaneous nerve. This nerve courses laterally over the lateral head of the gastrocnemius. The common fibular nerve also gives off a small cutaneous branch which is the lateral sural cutaneous nerve. When the common fibular nerve is divided from the sciatic nerve, it travels parallel to the distal portion of the biceps femoris muscle and towards the fibular head. The small cutaneous branch arises as the common fibular nerve travels towards the fibular head. The nerve then continues down the leg on the posterior-lateral side, then posterior to the lateral malleolus where it runs deep to the fibularis tendon sheath and reaches the lateral tuberosity of the fifth toe, where it ramifies.[2][3][4]
From the mid calf down to the ankle the nerve courses close to the skin along a line drawn from the mid-posterior popliteal fossa to just posterior to the lateral malleolus and then under the malleolus and forward along the lateral aspect of the foot.
Function
The sural nerve supplies sensation to the skin of the lateral foot and lateral lower ankle.[1]
The nerve transmits sensory signals from the posterior lateral corner of the leg and the lateral foot and 5th toe towards the spinal cord and brain.[2]
Clinical significance
The sural nerve has a purely sensory function, and so its removal results in only a relatively minor deficit. For this reason, it is often used for nerve biopsy, as well as the donor nerve when a nerve graft is performed.
Sural nerve block
A sural nerve block can be used for quick anesthetization to the foot and lower leg. Because this technique requires few injections to reach adequate anesthesia, a smaller volume of anesthetic is needed.[5] The sural nerve is rather superficial, which makes it more accessible to surgeons. Therefore, it is relatively easier than other procedures. Also, due to its superficial properties, the sural nerve is easily blocked at multiple levels at or above the ankle. In one study, regional anesthesia of the foot and ankle, when performed by surgeons, was completely successful 95% of the time.[6] Sural nerve block is not advised if a patient is allergic to the anesthetic solution, has infected tissue at the injection site, has severe bleeding disorder, or has preexisting neurological damage.[7]
Disease
Sural mononeuropathy is uncommon. If affected, it can be due to a mass lesion such as a ganglion or to trauma, which is the most common cause.[8] Sometimes inflammatory or vasculitic diseases will selectively involve the sural nerve. In addition, the sural nerve will be involved in any kind of generalized peripheral sensory or sensorimotor neuropathy. Sensory changes from sural neuropathy are variable but usually occur in the postero-lateral aspect of the leg and the dorso-lateral foot. These can sometimes be painful with paresthesias and dysesthesias.[9] Nerve conduction studies can be used to delineate sural nerve lesions.[10] Treatment will depend on the cause of the neuropathy. Occasionally biopsy of the nerve is performed for diagnostic purposes. For example, ganglions are usually resected. Traumatic neuropathy is usually treated non-surgically.[8] Sural nerve damage is usually part of a more generalised peripheral neuropathy.[11]
Additional images
- Areas of skin sensation supplied by nerves in the leg.
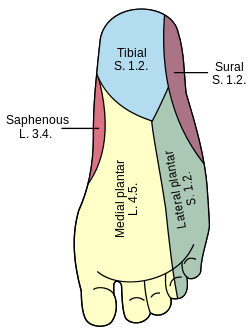 Areas of skin supplied by nerves of the leg - the sural nerve supplies the lateral ankle.
Areas of skin supplied by nerves of the leg - the sural nerve supplies the lateral ankle.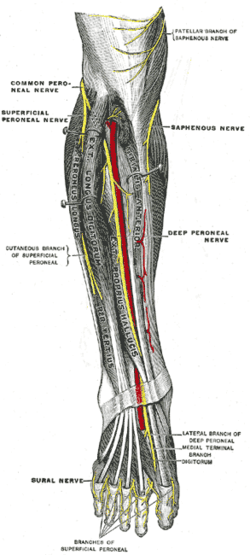 Deep nerves of the front of the leg.
Deep nerves of the front of the leg.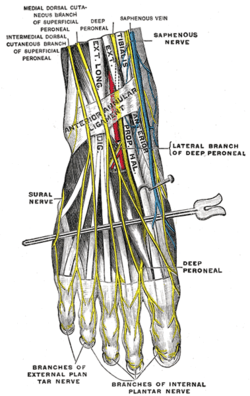 Course of nerves at the bottom of the foot.
Course of nerves at the bottom of the foot.
References
This article incorporates text in the public domain from page 963 of the 20th edition of Gray's Anatomy (1918)
- Medical Research Council Memorandum 45. Aids to the examination of the peripheral nervous system. 1975 London: Her Majesty's Stationery Office. p 54.
- "The Sural Nerve, Anatomy and entrapment". Functional Anatomy. November 26, 2009.
- Lawrence SJ1, Botte MJ. (1994). The sural nerve in the foot and ankle: an anatomic study with clinical and surgical implications. Foot Ankle International. Sep;15(9):490-4.
- Mestdagh H1, Drizenko A, Maynou C, Demondion X, Monier R. (2001). Origin and make up of the human sural nerve. Surg Radiol Anat. Sep;23(5):307-12.
- Crystal, Chad S.; Blankenship, Robert B. (2005). "Local Anesthetics and Peripheral Nerve Blocks in the Emergency Department". Emergency Medicine Clinics of North America. 23 (2): 477–502. doi:10.1016/j.emc.2004.12.012. PMID 15829393.
- Myerson, M. S.; Ruland, C. M.; Allon, S. M. (1992). "Regional Anesthesia for Foot and Ankle Surgery". Foot & Ankle International. 13 (5): 282–8. doi:10.1177/107110079201300510. PMID 1624194.
- Sural Nerve Block at eMedicine
- Stickler DE, Morley KN, Massey EW. Sural neuropathy: etiologies and predisposing factors. Muscle Nerve. 4:482-484, 2006.
- Yuebing L, Lederman RJ. Sural mononeuropathy: A report of 36 cases. Muscle Nerve 49:443-445, 2014.
- Kimura J. Electrodiagnosis in Diseases of Nerve and Muscle: Principles and Practice. 1983 Philadelphia, FA Davis, p 502.
- "Sural Nerve Pain - Causes, Symptoms & Treatment of Neuritis". Pain Care - Comprehensive Guide For Treatment Of Pain. Retrieved 1 October 2016.
External links
- Anatomy photo:11:07-0202 at the SUNY Downstate Medical Center
- Sural_nerve at the Duke University Health System's Orthopedics program
- Cutaneous field