Lactic acidosis
Lactic acidosis is a medical condition characterized by the buildup of lactate (especially L-lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates due to a problem with the body's oxidative metabolism.
| Lactic acidosis | |
|---|---|
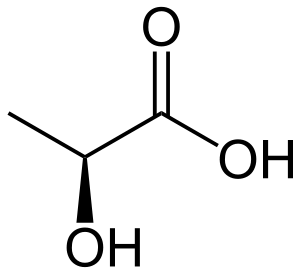 | |
| L-(+)-lactic acid | |
| Specialty | Endocrinology |
Lactic acidosis is typically the result of an underlying acute or chronic medical condition, medication, or poisoning. The symptoms are generally attributable to these underlying causes, but may include nausea, vomiting, Kussmaul breathing (laboured and deep), and generalised weakness.
The diagnosis is made on biochemical analysis of blood (often initially on arterial blood gas samples), and once confirmed, generally prompts an investigation to establish the underlying cause to treat the acidosis. In some situations, hemofiltration (purification of the blood) is temporarily required. In rare chronic forms of lactic acidosis caused by mitochondrial disease, a specific diet or dichloroacetate may be used. The prognosis of lactic acidosis depends largely on the underlying cause; in some situations (such as severe infections), it indicates an increased risk of death.
Classification
The Cohen-Woods classification categorizes causes of lactic acidosis as:[1]
- Type A: Decreased tissue oxygenation (e.g., from decreased blood flow)
- Type B
- B1: Underlying diseases (sometimes causing type A)
- B2: Medication or intoxication
- B3: Inborn error of metabolism
Signs and symptoms
Lactic acidosis is commonly found in people who are unwell, such as those with severe heart and/or lung disease, a severe infection with sepsis, the systemic inflammatory response syndrome due to another cause, severe physical trauma, or severe depletion of body fluids.[2] Symptoms in humans include all those of typical metabolic acidosis (nausea, vomiting, generalized muscle weakness, and laboured and deep breathing).[3]
Causes
The several different causes of lactic acidosis include:
- Genetic conditions
- Biotinidase deficiency, multiple carboxylase deficiency, or nongenetic deficiencies of biotin
- Diabetes mellitus and deafness
- Fructose 1,6-bisphosphatase deficiency
- Glucose-6-phosphatase deficiency
- GRACILE syndrome
- Mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes
- Pyruvate dehydrogenase deficiency
- Pyruvate carboxylase deficiency
- Leigh syndrome
- Drugs
- Linezolid[4]
- Paracetamol/acetaminophen poisoning[5]
- Metformin: this risk is low (less than 10 cases for 100,000 patient years), but the risk of metformin-induced lactic acidosis (MALA) increases in certain situations where both the plasma levels of metformin are increased and lactate clearance is impaired.[6] The older related and now withdrawn drug phenformin carried a much higher risk of lactic acidosis.[7]
- Isoniazid toxicity
- Propofol
- Epinephrine
- Propylene glycol (D-lactic acidosis)
- Nucleoside reverse-transcriptase inhibitors
- Abacavir/dolutegravir/lamivudine[8]
- Emtricitabine/tenofovir[9]
- Potassium cyanide (cyanide poisoning)
- Fialuridine[10]
- Other
- Thiamine deficiency (especially during TPN)
- Impaired delivery of oxygen to cells in the tissues (e.g., from impaired blood flow (hypoperfusion))
- Bleeding
- Polymyositis
- Ethanol toxicity
- Sepsis
- Shock
- Advanced liver disease
- Diabetic ketoacidosis
- Excessive exercise (overtraining)
- Regional hypoperfusion (e.g., bowel ischemia or marked cellulitis)
- Cancers such as Non-Hodgkin's and Burkitt lymphomas
- Pheochromocytoma[2]
- Tumor lysis syndrome[11]
- D-lactic acidosis due to intestinal bacterial flora production in short gut syndrome
Pathophysiology
Most cells in the body normally metabolize glucose to form water and carbon dioxide in a two-step process. First, glucose is broken down to pyruvate through glycolysis. Then, mitochondria oxidize the pyruvate into water and carbon dioxide by means of the Krebs cycle and oxidative phosphorylation. This second step requires oxygen. The net result is ATP, the energy carrier used by the cell for metabolic activities and to perform work, such as muscle contraction. When the energy in ATP is used during cell work via ATP hydrolysis, hydrogen ions, (positively charged protons) are released. The mitochondria normally incorporate these free hydrogen nuclei back into ATP, thus preventing buildup of unbound hydrogen cations, and maintaining neutral pH.
If oxygen supply is inadequate (hypoxia), the mitochondria are unable to continue creating ATP at a rate sufficient to meet the cell's energy needs. In this situation, glycolysis is increased to provide additional ATP, and the excess pyruvate produced is converted into lactate and released from the cell into the bloodstream, where it accumulates over time. While increased glycolysis helps compensate for less ATP from oxidative phosphorylation, it cannot bind the hydrogen cations that result from ATP hydrolysis. Therefore, hydrogen cation concentration rises and causes acidosis.[12]
The excess hydrogen cations produced during lactic acidosis are widely believed to actually derive from production of lactic acid. This is incorrect, as cells do not produce lactic acid; pyruvate is converted directly into lactate, the anionic form of lactic acid. When excess intracellular lactate is released into the blood, maintenance of electroneutrality of the blood requires that a cation be released into the blood, as well. This can reduce blood pH. Glycolysis coupled with lactate production is neutral in the sense that it does not produce excess hydrogen cations; however, pyruvate production does produce them. Lactate production is buffered intracellularly, e.g. the lactate-producing enzyme, lactate dehydrogenase, binds one hydrogen cation per pyruvate molecule converted. When such buffer systems become saturated, cells will transport lactate into the bloodstream. Hypoxia certainly causes both a buildup of lactate and acidification, and lactate is therefore a good "marker" of hypoxia, but lactate itself is not the cause of low pH.[13] During exercise and some illnesses, lactate production is not generated by lack of oxygen, per se, but by the catecholamine-driven metabolism of glucose (glycolysis) that cells use when they cannot get enough energy from oxygen-based reactions.
Lactate serves as an energy source for other tissues.[14]
Lactic acidosis sometimes occurs without hypoxia, for example, in rare inborn errors of metabolism where mitochondria do not function at full capacity. In such cases, when the body needs more energy than usual, for example during exercise or disease, mitochondria cannot match the cells' demand for ATP, and lactic acidosis results. Also, muscle types that have few mitochondria and preferentially use glycolysis for ATP production (fast-twitch or type II fibers) are naturally prone to lactic acidosis.
Lactic acidosis is also a consequence of the processes causing rigor mortis. In the absence of oxygen, tissue in the muscles of the deceased carry out anaerobic metabolism using muscle glycogen as the energy source, causing acidification. With depletion of muscle glycogen, the loss of ATP causes the muscles to grow stiff, as the actin-myosin bonds cannot be released. (Rigor is later resolved by enzymatic breakdown of the myofibers.)
Diagnosis
Acid-base disturbances such as lactic acidosis are typically first assessed using arterial blood gas tests. Testing of venous blood is also available as an alternative. Normally resulting lactate concentrations are in the range indicated below:[15]
| mg/dL | mM | |
|---|---|---|
| Venous blood | 4.5 – 19.8 | 0.5 – 2.2 |
| Arterial blood | 4.5 – 14.4 | 0.5 – 1.6 |
Treatment
Direct removal of lactate from the body (e.g. with hemofiltration) is difficult, with limited evidence for benefit.[16] In type A lactic acidosis, treatment consists of effective management of the underlying cause, and limited evidence supports the use of sodium bicarbonate solutions to improve the pH (which is associated with increased carbon dioxide generation and may reduce the calcium levels).[17]
In type B lactic acidosis produced by medication, withdrawal of the medication may be necessary to resolve the lactic acidosis.
Lactic acidosis in the context of mitochondrial disorders (type B3) may be treated with a ketogenic diet and possibly with dichloroacetate (DCA),[18] although this may be complicated by peripheral neuropathy and has a weak evidence base.[19]
Prognosis
The underlying cause determines the prognosis of lactic acidosis. In sepsis, elevated lactate levels correlate with mortality. The mortality of lactic acidosis in people taking metformin was previously reported to be 50%, but in more recent reports this was closer to 25%.[20]
Other animals
Reptiles
Reptiles, which rely primarily on anaerobic energy metabolism (glycolysis) for intense movements, can be particularly susceptible to lactic acidosis. In particular, during the capture of large crocodiles, the animals' use of their glycolytic muscles often alter the blood's pH to a point where they are unable to respond to stimuli or move.[21] Cases are recorded in which particularly large crocodiles which put up extreme resistance to capture later died of the resulting pH imbalance.[22]
Certain turtle species have been found to be capable of tolerating high levels of lactic acid without suffering the effects of lactic acidosis. Painted turtles hibernate buried in mud or underwater and do not resurface for the entire winter. As a result, they rely on anaerobic respiration to provide the majority of their energy needs.[23] Adaptations in particular in the turtle's blood composition and shell allow it to tolerate high levels of lactic acid accumulation. In the anoxic conditions where anaerobic respiration is dominant, calcium levels in the blood plasma increase.[23] This calcium serves as a buffer, reacting with the excess lactate to form the precipitate calcium lactate. This precipitate is suggested to be reabsorbed by the shell and skeleton, thereby removing it from the bloodstream; studies examining turtles that have been subjected to prolonged anoxic conditions have up to 45% of their lactate stored within their skeletal structure.[23]
Ruminants
In ruminant livestock, the cause of clinically serious lactic acidosis is different from the causes described above.
In domesticated ruminants, lactic acidosis may occur as a consequence of ingesting large amounts of grain, especially when the rumen population is poorly adapted to deal with grain.[24][25][26] Activity of various rumen organisms results in accumulation of various volatile fatty acids (normally, mostly acetic, propionic, and butyric acids), which are partially dissociated.[27] Although some lactate is normally produced in the rumen, it is normally metabolized by such organisms as Megasphaera elsdenii and, to a lesser extent, Selenomonas ruminantium and some other organisms. With high grain consumption, the concentration of dissociated organic acids can become quite high, resulting in rumen pH dropping below 6. Within this lower pH range, Lactobacillus spp. (producing lactate and hydrogen ions) are favored, and M. elsdenii and S. ruminantium are inhibited, tending to result in a considerable rise of lactate and hydrogen ion concentrations in the rumen fluid.[28] The pKa of lactic acid is low, about 3.9, versus, for example, 4.8 for acetic acid; this contributes to the considerable drop in rumen pH which can occur.[27]
Because of the high solute concentration of the rumen fluid under such conditions, considerable water is translocated from the blood to the rumen along the osmotic potential gradient, resulting in dehydration which cannot be relieved by drinking, and which can ultimately lead to hypovolemic shock.[24] As more lactate accumulates and rumen pH drops, the ruminal concentration of undissociated lactic acid increases. Undissociated lactic acid can cross the rumen wall to the blood,[29] where it dissociates, lowering blood pH. Both L and D isomers of lactic acid are produced in the rumen;[24] these isomers are metabolized by different metabolic pathways, and activity of the principal enzyme involved in metabolism of the D isomer declines greatly with lower pH, tending to result in an increased ratio of D:L isomers as acidosis progresses.[28]
Measures for preventing lactic acidosis in ruminants include avoidance of excessive amounts of grain in the diet, and gradual introduction of grain over a period of several days, to develop a rumen population capable of safely dealing with a relatively high grain intake.[24][25][26] Administration of lasalocid or monensin in feed can reduce risk of lactic acidosis in ruminants,[30] inhibiting most of the lactate-producing bacterial species without inhibiting the major lactate fermenters.[31] Also, using a higher feeding frequency to provide the daily grain ration can allow higher grain intake without reducing the pH of the rumen fluid.[32]
Treatment of lactic acidosis in ruminants may involve intravenous administration of dilute sodium bicarbonate, oral administration of magnesium hydroxide, and/or repeated removal of rumen fluids and replacement with water (followed by reinoculation with rumen organisms, if necessary).[24][25][26]
References
- Woods, Hubert Frank; Cohen, Robert (1976). Clinical and biochemical aspects of lactic acidosis. Oxford: Blackwell Scientific. ISBN 0-632-09460-5.
- Kraut, Jeffrey A.; Madias, Nicolaos E. (11 December 2014). "Lactic Acidosis". New England Journal of Medicine. 371 (24): 2309–2319. doi:10.1056/NEJMra1309483. PMID 25494270.
- MedlinePlus Encyclopedia Lactic acidosis
- Santini, A; Ronchi, D; Garbellini, M; Piga, D; Protti, A (July 2017). "Linezolid-induced lactic acidosis: the thin line between bacterial and mitochondrial ribosomes". Expert Opinion on Drug Safety. 16 (7): 833–843. doi:10.1080/14740338.2017.1335305. PMID 28538105.
- Shah, AD; Wood, DM; Dargan, PI (January 2011). "Understanding lactic acidosis in paracetamol (acetaminophen) poisoning". British Journal of Clinical Pharmacology. 71 (1): 20–8. doi:10.1111/j.1365-2125.2010.03765.x. PMC 3018022. PMID 21143497.
- DeFronzo, R; Fleming, GA; Chen, K; Bicsak, TA (February 2016). "Metformin-associated lactic acidosis: Current perspectives on causes and risk". Metabolism: Clinical and Experimental. 65 (2): 20–9. doi:10.1016/j.metabol.2015.10.014. PMID 26773926.
- Fimognari, F. L.; Pastorelli, R.; Incalzi, R. A. (2006). "Phenformin-Induced Lactic Acidosis in an Older Diabetic Patient: A recurrent drama (phenformin and lactic acidosis)". Diabetes Care. 29 (4): 950–1. doi:10.2337/diacare.29.04.06.dc06-0012. PMID 16567854.
- "Triumeq (Abacavir, Dolutegravir, and Lamivudine Film-coated Tablets) Drug Information: Description, User Reviews, Drug Side Effects, Interactions – Prescribing Information at RxList". RxList. Retrieved 2016-03-25.
- "Truvada".
- McKenzie, Robin; Fried, Michael W.; Sallie, Richard; Conjeevaram, Hari; Di Bisceglie, Adrian M.; Park, Yoon; Savarese, Barbara; Kleiner, David; Tsokos, Maria; Luciano, Carlos; Pruett, Timothy; Stotka, Jennifer L.; Straus, Stephen E.; Hoofnagle, Jay H. (1995). "Hepatic Failure and Lactic Acidosis Due to Fialuridine (FIAU), an Investigational Nucleoside Analogue for Chronic Hepatitis B". New England Journal of Medicine. 333 (17): 1099–105. doi:10.1056/NEJM199510263331702. PMID 7565947.
- Darmon, Michael; Malak, Sandra; Guichard, Isabelle; Schlemmer, Benoit (July–September 2008). "Acute tumor lysis syndrome: a comprehensive review". Revista Brasileira de Terapia Intensiva. 20 (3): 278–285. doi:10.1590/S0103-507X2008000300011. ISSN 0103-507X.
- Hochachka, P. W.; Mommsen, T. P. (1983). "Protons and anaerobiosis". Science. 219 (4591): 1391–7. Bibcode:1983Sci...219.1391H. doi:10.1126/science.6298937. PMID 6298937.
- Robergs, Robert A.; Ghiasvand, Farzenah; Parker Daryl (2004). "Biochemistry of exercise-induced metabolic acidosis". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 287 (3): R502–16. doi:10.1152/ajpregu.00114.2004. PMID 15308499.
- Gladden, LB (Mar 2008). "Current trends in lactate metabolism: introduction". Medicine & Science in Sports & Exercise. 40 (3): 475–6. doi:10.1249/MSS.0b013e31816154c9. PMID 18379209.
- Goldman, Lee; Schafer, Andrew (May 11, 2015). Goldman-Cecil Medicine (25 ed.). Elsevier. ISBN 978-1455750177.
- Cerdá, J; Tolwani, AJ; Warnock, DG (Jul 2012). "Critical care nephrology: management of acid-base disorders with CRRT". Kidney International. 82 (1): 9–18. doi:10.1038/ki.2011.243. PMID 21814173.
- Boyd, JH; Walley, KR (Aug 2008). "Is there a role for sodium bicarbonate in treating lactic acidosis from shock?". Current Opinion in Critical Care. 14 (4): 379–83. doi:10.1097/MCC.0b013e3283069d5c. PMID 18614899.
- Stacpoole, PW; Kurtz, TL; Han, Z; Langaee, T (2008). "Role of dichloroacetate in the treatment of genetic mitochondrial diseases". Advanced Drug Delivery Reviews. 60 (13–14): 1478–87. doi:10.1016/j.addr.2008.02.014. PMC 3746325. PMID 18647626.
- Pfeffer, G; Majamaa, K; Turnbull, DM; Thorburn, D; Chinnery, PF (2012). Chinnery, Patrick F (ed.). "Treatment for mitochondrial disorders". The Cochrane Database of Systematic Reviews. 4 (4): CD004426. doi:10.1002/14651858.CD004426.pub3. PMID 22513923.
- Kajbaf, F; Lalau, JD (November 2014). "Mortality rate in so-called "metformin-associated lactic acidosis": a review of the data since the 1960s". Pharmacoepidemiology and Drug Safety. 23 (11): 1123–7. doi:10.1002/pds.3689. PMID 25079826.
- Seymour R. S.; Webb G. J. W.; Bennett A. F.; Bradford D. F. (1987). "Chapter 26. Effect of capture on the physiology of Crocodylus porosus" (PDF). In Webb, G. J. W.; Manolis, S. C.; Whitehead, P. J. (eds.). Wildlife Management: Crocodiles and Alligators. Sydney: Surrey Beatty. pp. 253–257.
- . Accessed 31 January 2009.
- Jackson, Donald C. (2002). "Hibernating without oxygen: physiological adaptations of the painted turtle". The Journal of Physiology. 543 (3): 731–737. doi:10.1113/jphysiol.2002.024729. PMC 2290531. PMID 12231634.
- Kimberling, C. V. 1988. Jensen and Swift's diseases of sheep. 3rd Ed. Lea & Fibiger, Philadelphia. 394 pp.
- Pugh, D. G. 2002. Sheep and goat medicine. Saunders. 468 pp.
- Kahn, C. M. (ed.) 2005. Merck veterinary manual. 9th Ed. Merck & Co., Inc., Whitehouse Station.
- Van Soest, P. J. 1994. Nutritional ecology of the ruminant. 2nd Ed. Cornell Univ. Press, Ithaca. 476 pp.
- Nocek, J. E. 1997. Bovine acidosis: implications on laminitis. J. Dairy Sci. 80: 1005–1028.
- Owens, FN; Secrist, DS; Hill, WJ; Gill, DR (1998). "Acidosis in cattle: a review". Journal of Animal Science. 76 (1): 275–86. doi:10.2527/1998.761275x. PMID 9464909.
- Nagaraja, TG; Avery, TB; Bartley, EE; Galitzer, SJ; Dayton, AD (1981). "Prevention of lactic acidosis in cattle by lasalocid or monensin". Journal of Animal Science. 53 (1): 206–16. doi:10.2527/jas1981.531206x. PMID 7319937.
- Dennis, SM; Nagaraja, TG; Bartley, EE (1981). "Effects of lasalocid or monensin on lactate-producing or -using rumen bacteria". Journal of Animal Science. 52 (2): 418–26. doi:10.2527/jas1981.522418x. PMID 7275867.
- Kaufmann, W. 1976. Influence of the composition of the ration and the feeding frequency on ph-regulation in the rumen and on feed in-take in ruminants. Livestock Prod. Sci. 3: 103–114.
External links
| Classification | |
|---|---|
| External resources |