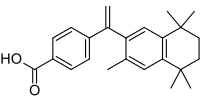
Bexarotene
Bexarotene (brand name: Targretin) is an antineoplastic (anti-cancer) agent approved by the U.S.Food and Drug Administration (FDA) (in late 1999) and the European Medicines Agency (EMA) (early 2001) for use as a treatment for cutaneous T cell lymphoma (CTCL).[1] It is a third-generation retinoid.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Targretin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608006 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral and topical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | >99% |
| Metabolism | Hepatic (CYP3A4-mediated) |
| Elimination half-life | 7 hours |
| Excretion | Parent drug and metabolites are eliminated primarily through the hepatobiliary system. Less than 1% is excreted in the urine unchanged. |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.206.790 |
| Chemical and physical data | |
| Formula | C24H28O2 |
| Molar mass | 348.478 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Medical uses
Bexarotene is indicated for the treatment of cutaneous manifestations of cutaneous T-cell lymphoma in people who are refractory to at least one prior systemic therapy (oral) and for the topical treatment of cutaneous lesions in patients with CTCL who have refractory or persistent disease after other therapies or who have not tolerated other therapies (topical).[2]
It has been used off-label for non-small cell lung cancer[3] and breast cancer.[4]
Contraindications
Known contraindications include:[5]
- Hypersensitivity to the active substance or to any of the excipients in the preparation(s).
- Pregnancy and lactation
- Women of child-bearing potential without effective birth-control measures
- History of pancreatitis
- Uncontrolled hypercholesterolaemia
- Uncontrolled hypertriglyceridaemia
- Hypervitaminosis A
- Uncontrolled thyroid disease
- Hepatic insufficiency
- Ongoing systemic infection
Adverse effects
Overall the most common adverse effects are skin reactions (mostly itchiness and rashes), leucopenia, headache, weakness, thyroid anomalies (which seem to be mediated by RXR-mediated downregulation of thyroid stimulating hormone) and blood lipid anomalies such as hypercholesterolaemia (high blood cholesterol) and hyperlipidaemia, hypothyroidism.[2][5][6][7]
Interactions
Its plasma concentration may be increased by concomitant treatment with CYP3A4 inhibitors such as ketoconazole.[5] It may also induce CYP3A4, and hence CYP3A4 substrates like cyclophosphamide may have their plasma concentrations reduced.[5] Likewise consumption of grapefruit juice might increase bexarotene's plasma concentrations, hence potentially altering its therapeutic effects.[5]
Mechanism
Bexarotene is a retinoid that selectively activates retinoid X receptors (RXRs), as opposed to the retinoic acid receptors, the other major target of retinoic acid (the acid form of vitamin A).[7][8][9] By so doing it induces cell differentiation and apoptosis and prevents the development of drug resistance.[10] It also has anti-angiogenic effects and inhibits cancer metastasis.[10] The retinoic acid receptors (RARs) regulate cell differentiation and proliferation whereas RXRs regulate apoptosis.[6]
Physical properties
Bexarotene is a solid, white powder. It is poorly soluble in water; the solubility is estimated to be about 10-50 μM. It is soluble in DMSO at 65 mg/mL and in ethanol at 10 mg/mL with warming.[11]
History
SRI International and the La Jolla Cancer Research Foundation (now the Sanford-Burnham Medical Research Institute) collaborated on work that resulted in patent filings for the drug.[12]
The developer of bexarotene (brand name Targretin) was Ligand Pharmaceuticals, a San Diego biotech company which received FDA approval for the drug in 1999.[13] The FDA approved bexarotene on 29 December 1999.[14]
Japanese pharmaceutical Eisai bought the rights to Targretin and three other anti-cancer products from Ligand in 2006.[13] In the United States, patents on the drug expired in 2016.[13]
It received EMA approval on 29 March 2001.[15]
Early-stage preclinical studies suggested that bexarotene reduced amyloid plaques and improved mental functioning in a small sample of mice engineered to exhibit Alzheimer's-like symptoms [16][17] although subsequent studies have yielded mixed results.[18][19][20][21][22]
References
- Gniadecki, R; Assaf, C; Bagot, M; Dummer, R; Duvic, M; Knobler, R; Ranki, A; Schwandt, P; Whittaker, S (2007). "The optimal use of bexarotene in cutaneous T-cell lymphoma". British Journal of Dermatology. 157 (3): 433–40. doi:10.1111/j.1365-2133.2007.07975.x. PMID 17553039.
- "TARGRETIN (BEXAROTENE) CAPSULE [CARDINAL HEALTH]". DailyMed. Cardinal Health. March 2006. Retrieved 12 January 2014.
- Dragnev, KH; Petty, WJ; Shah, SJ; Lewis, LD; Black, CC; Memoli, V; Nugent, WC; Hermann, T; Negro-Vilar, A; Rigas, JR; Dmitrovsky, E (2007). "A proof-of-principle clinical trial of bexarotene in patients with non-small cell lung cancer" (PDF). Clinical Cancer Research. 13 (6): 1794–800. doi:10.1158/1078-0432.CCR-06-1836. PMID 17363535.
- Esteva, FJ; Glaspy, J; Baidas, S; Laufman, L; Hutchins, L; Dickler, M; Tripathy, D; Cohen, R; DeMichele, A; Yocum, RC; Osborne, CK; Hayes, DF; Hortobagyi, GN; Winer, E; Demetri, GD (March 2003). "Multicenter Phase II Study of Oral Bexarotene for Patients With Metastatic Breast Cancer" (PDF). Journal of Clinical Oncology. 21 (6): 999–1006. doi:10.1200/JCO.2003.05.068. PMID 12637463.
- "Targretin Capsules - Summary of Product Characteristics". electronic Medicines Compendium. Eisai Ltd. 4 April 2013. Retrieved 14 January 2014.
- Brunton, L; Chabner, B; Knollman, B (2010). Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill Professional. ISBN 978-0-07-162442-8.
- "Targretin (bexarotene) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Retrieved 31 January 2014.
- Rowe, A (February 1997). "Retinoid X receptors". The International Journal of Biochemistry & Cell Biology. 29 (2): 275–278. doi:10.1016/S1357-2725(96)00101-X. PMID 9147128.
- Dawson, M. I.; Xia, Z. (2012). "The retinoid X receptors and their ligands". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 1821 (1): 21–56. doi:10.1016/j.bbalip.2011.09.014. PMC 4097889. PMID 22020178.
- Qu, L; Tang, X (January 2010). "Bexarotene: a promising anticancer agent". Cancer Chemotherapy and Pharmacology. 65 (2): 201–205. doi:10.1007/s00280-009-1140-4. PMID 19777233.
- "Bexarotene MSDS". LC Labs. Archived from the original on 9 May 2015.
- "Lymphoma Treatment: Targretin (bexarotene)". Timeline of Innovation. SRI International. Retrieved 20 September 2013.
- Vinluan, Frank (12 October 2011). "Generic cancer drug from Banner aims to take on Eisai's Targretin". MedCity News. Retrieved 11 February 2012.
- "Bexarotene". Drugs.com. Archived from the original on 12 January 2014. Retrieved 12 January 2014.
- "Targretin : EPAR - Product Information" (PDF). European Medicines Agency. Eisai Ltd. 3 April 2013. Retrieved 12 January 2014.
- Cramer, P. E.; Cirrito, J. R.; Wesson, D. W.; Lee, C. Y. D.; Karlo, J. C.; Zinn, A. E.; Casali, B. T.; Restivo, J. L.; et al. (2012). "ApoE-Directed Therapeutics Rapidly Clear β-Amyloid and Reverse Deficits in AD Mouse Models". Science. 335 (6075): 1503–1506. doi:10.1126/science.1217697. PMC 3651582. PMID 22323736.
- MedicalXpress (9 February 2012). "FDA-approved drug rapidly clears amyloid from the brain, reverses Alzheimer's symptoms in mice". MedicalXpress. Retrieved 14 February 2012.
- Fitz, N. F.; Cronican, A. A.; Lefterov, I.; Koldamova, R. (2013). "Comment on "ApoE-Directed Therapeutics Rapidly Clear β-Amyloid and Reverse Deficits in AD Mouse Models"". Science. 340 (6135): 924. doi:10.1126/science.1235809. PMC 4086452.
- Price, A. R.; Xu, G.; Siemienski, Z. B.; Smithson, L. A.; Borchelt, D. R.; Golde, T. E.; Felsenstein, K. M. (2013). "Comment on "ApoE-Directed Therapeutics Rapidly Clear β-Amyloid and Reverse Deficits in AD Mouse Models"". Science. 340 (6135): 924. doi:10.1126/science.1234089. PMC 4086452.
- Tesseur, I.; Lo, A. C.; Roberfroid, A.; Dietvorst, S.; Van Broeck, B.; Borgers, M.; Gijsen, H.; Moechars, D.; et al. (2013). "Comment on "ApoE-Directed Therapeutics Rapidly Clear β-Amyloid and Reverse Deficits in AD Mouse Models"". Science. 340 (6135): 924. doi:10.1126/science.1233937. PMC 4086452.
- Veeraraghavalu, K.; Zhang, C.; Miller, S.; Hefendehl, J. K.; Rajapaksha, T. W.; Ulrich, J.; Jucker, M.; Holtzman, D. M.; et al. (2013). "Comment on "ApoE-Directed Therapeutics Rapidly Clear β-Amyloid and Reverse Deficits in AD Mouse Models"". Science. 340 (6135): 924. doi:10.1126/science.1235505. PMC 4086452.
- "Anti-Cancer Drug Reverses Alzheimer's Disease In Mice". Medical News Today. 25 May 2013.