Ischemic preconditioning
Ischemic preconditioning (IPC) is an experimental technique[1] for producing resistance to the loss of blood supply, and thus oxygen, to tissues of many types. In the heart, IPC is an intrinsic process whereby repeated short episodes of ischaemia protect the myocardium against a subsequent ischaemic insult. It was first identified in 1986 by Murry et al. This group exposed anesthetised open-chest dogs to four periods of 5 minute coronary artery occlusions followed by a 5-minute period of reperfusion before the onset of a 40-minute sustained occlusion of the coronary artery. The control animals had no such period of “ischaemic preconditioning” and had much larger infarct sizes compared with the dogs that did.[2] The exact molecular pathways behind this phenomenon have yet to be fully understood.
| Ischemic preconditioning | |
|---|---|
| MeSH | D019194 |
Background
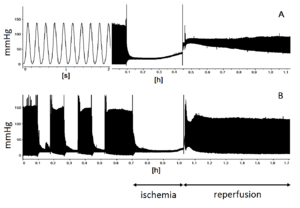
If the blood supply to an organ or a tissue is impaired for a short time (usually less than five minutes) then restored so that blood flow is resumed, and the process repeated two or more times, the cells downstream of the tissue or organ are robustly protected from a final ischemic insult when the blood supply is cut off entirely and permanently.
The protective effect which is imparted by IPC has two windows of protection. The first, lasts between 4–6 hours [3] and has been named classical or early preconditioning. The second window begins at 24 hours lasting up to 72 hours post the ischaemia and reperfusion stimulus.[4]
In an experimental setting if the left anterior descending coronary artery of the animal is ligated the downstream cardiac cellular mass is infarcted and will be injured and then die. If, on the other hand the tissue is subjected to IPC the downstream cellular mass will sustain only minimal to modest damage. IPC protects the tissue by initiating a cascade of biochemical events that allows for an up-regulation of the energetics of the tissue. The locus of this phenomenon is the intracellular organelle, the mitochondrion.
Investigations of various exogenous circulating ligands such as the delta active opiates and opioids simulate the phenomenon of IPC thus protecting the downstream tissues without the IPC intermittent ligating procedure.
Methods to either mimic or elicit IPC have been attempted in clinical practice, in the area of coronary heart disease in an attempt to limit the injury caused to the heart via ischemia and reperfusion injury.[5] Such injury would occur when a patient has an acute myocardial infarct followed by reperfusion by either percutaneous coronary intervention or thrombolysis.
Early Preconditioning
Is thought to be stimulated by local action of adenosine, opiates and bradykinin which are all endogenously released by ischemic cells. The presence of each substance is not required but the protection is more potent if they are. They activate G-protein coupled pathways, which carries a protective signal to an end-effector. There have been many suggestions to what this might be, the sarcolemmal ATP-sensitive potassium channel, the mitochondrial ATP-sensitive potassium channel, the mitochondrial permeability transition pore, reactive oxygen species generation, chloride channels, the inward rectifier potassium ion channel and connexon 43 related channels.
Impairment of Preconditioning
It has also been shown that the protective effect of IPC is suppressed by pathological conditions such as hypercholesterolemia, hyperglycemia, hypertension, cardiac hypertrophy, aging, obesity and hyperhomocysteinemia.
Application
The only group of humans who are chronically exposed to an opioid with delta activity are methadone maintained patients treated for chronic pain or opioid addiction. These patients have a coronary risk profile greater than the general population:
- 90% smoke. In the general population in the USA ~25% smoke.
- Heart Healthy living i.e. attention to lipid control is less frequent than in the general population
- ~25% of the patients in Methadone Maintenance Programs use the highly ischemogenic cocaine one or more times a year. In the general population in the USA less than 1% are reported to do so.
Preliminary and as yet unpublished surveys of the methadone treated population point to a high degree of protection from myocardial ischemic events. The one published study, an autopsy series from the Office of the Chief Medical Examiner of the City of New York demonstrated significantly less evidence for coronary occlusive disease. Simulation of IPC with methadone could not be evaluated in this post mortem investigation.
Remote pre- and post-conditioning
Rather than blocking a coronary artery, similar results have been seen by blocking the brachial artery using a blood pressure cuff prior to surgery.[6] Some research also suggests that ischemic conditioning is also beneficial following a stroke [7][8] or chronic cerebral hypoperfusion [9] or heart attack.[10]
References
- Citations
- Murry, C. E.; Jennings, R. B.; Reimer, K. A. (1986-11-01). "Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium". Circulation. 74 (5): 1124–1136. doi:10.1161/01.CIR.74.5.1124. ISSN 0009-7322. PMID 3769170.
- Murry, CE; Jennings, RB; Reimer, KA (November 1986). "Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium". Circulation. 74 (5): 1124–36. doi:10.1161/01.cir.74.5.1124. PMID 3769170.
- Rodrigo, GC; Samani, NJ (January 2008). "Ischemic preconditioning of the whole heart confers protection on subsequently isolated ventricular myocytes". American Journal of Physiology. Heart and Circulatory Physiology. 294 (1): H524–31. doi:10.1152/ajpheart.00980.2007. PMID 17965281.
- Das, Manika; Das, Dipak K. (31 March 2008). "Molecular mechanism of preconditioning". IUBMB Life. 60 (4): 199–203. doi:10.1002/iub.31. PMID 18344203.
- Johnson, Peter Anto (2019-05-02). "Cardioprotective actions of opioids in the ischemic heart: bypassing occlusions in our current knowledge". University of Toronto Medical Journal. 96 (2): 33 – 37–33 – 37. ISSN 1913-5440.
- Thielmann, Matthias; Kottenberg, Eva; Kleinbongard, Petra; Wendt, Daniel (17 August 2013). "Cardioprotective and prognostic effects of remote ischaemic preconditioning in patients undergoing coronary artery bypass surgery: a single-centre randomised, double-blind, controlled trial". The Lancet. 382 (9892): 597–604. doi:10.1016/S0140-6736(13)61450-6. PMID 23953384.
- Zhao, Heng (25 February 2009). "Ischemic postconditioning as a novel avenue to protect against brain injury after stroke". Journal of Cerebral Blood Flow & Metabolism. 29 (5): 873–885. doi:10.1038/jcbfm.2009.13. PMC 2736291. PMID 19240739.
- Pan LN, Zhu W, Li Y, Xu XL, Guo LJ, Lu Q, Wang J (2014). "Astrocytic Toll-like receptor 3 is associated with ischemic preconditioning-induced protection against brain ischemia in rodents". PLOS ONE. 9 (6): e99526. doi:10.1371/journal.pone.0099526. PMC 4051824. PMID 24914679.
- Wang J, Fu X, Yu L, Li N, Wang M, Liu X, Zhang D, Han W, Zhou C, Wang J (2015). "Preconditioning with VEGF enhances angiogenic and neuroprotective effects of bone marrow mononuclear cell transplantation in a rat model of chronic cerebral hypoperfusion". Mol. Neurobiol. 53 (9): 6057–6068. doi:10.1007/s12035-015-9512-8. PMC 4854818. PMID 26530694.
- ZQ, Zhao (August 2003). "Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning". Am J Physiol Heart Circ Physiol. 285 (2): H579–H588. doi:10.1152/ajpheart.01064.2002. PMID 12860564.
- Bibliography
- Gross GJ (2003). "Role of opioids in acute and delayed preconditioning". J. Mol. Cell. Cardiol. 35 (7): 709–18. doi:10.1016/S0022-2828(03)00135-4. PMID 12818560.
- Marmor M, Penn A, Widmer K, Levin RI, Maslansky R (2004). "Coronary artery disease and opioid use". Am. J. Cardiol. 93 (10): 1295–7. doi:10.1016/j.amjcard.2004.01.072. PMID 15135709.