Intravenous sugar solution
Intravenous sugar solution, also known as dextrose solution, is a mixture of dextrose (glucose) and water.[1] It is used to treat low blood sugar or water loss without electrolyte loss.[2] Water loss without electrolyte loss may occur in fever, hyperthyroidism, high blood calcium, or diabetes insipidus.[2] It is also used in the treatment of high blood potassium, diabetic ketoacidosis, and as part of parenteral nutrition.[2] It is given by injection into a vein.[2]
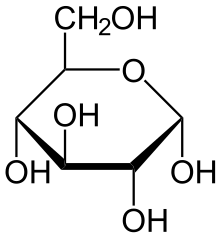 Chemical structure of dextrose | |
| Clinical data | |
|---|---|
| Other names | dextrose solution, glucose solution |
| AHFS/Drugs.com | Monograph |
| License data | |
| Pregnancy category |
|
| Routes of administration | intravenous |
| ATC code | |
| Identifiers | |
| ChemSpider |
|
Side effects may include irritation of the vein in which it is given, high blood sugar, and swelling.[2][3] Excess use may result in low blood sodium and other electrolyte problems.[2] Intravenous sugar solutions are in the crystalloid family of medications.[4] They come in a number of strengths including 5%, 10%, and 50% dextrose.[2] While they may start out hypertonic they become hypotonic solutions as the sugar is metabolised.[5] Versions are also available mixed with saline.[3]
Dextrose solutions for medical use became available in the 1920s and 1930s.[6][7] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[8] The wholesale cost in the developing world is about US$1.00–1.80 per liter of 10% dextrose in water, and it is about US$0.60–2.40 per liter of 5% dextrose in normal saline.[9][10] In the United Kingdom a 50 ml vial of 50% solution costs the NHS 2.01 pounds.[2]
Medical uses
Administering a 5% sugar solution peri- and postoperatively usually achieves a good balance between starvation reactions and hyperglycemia caused by sympathetic activation. A 10% solution may be more appropriate when the stress response from the reaction has decreased, after approximately one day after surgery. After more than approximately 2 days, a more complete regimen of total parenteral nutrition is indicated.
In patients with hypernatremia and euvolemia, free water can be replaced using either 5% D/W or 0.45% saline.
In patients with fatty-acid oxidation disorders (FOD), 10% solution may be appropriate upon arrival to the emergency room.
Side effects
Intravenous glucose is used in some Asian countries as a pick-me-up, for "energy," but is not a part of routine medical care in the United States where a glucose solution is a prescription drug. Asian immigrants to the United States are at risk if they seek intravenous glucose treatment. It may be had at store-front clinics catering to Asian immigrants, but, despite having no more effect than drinking sugared water, poses medical risks such as the possibility of infection. The procedure is commonly called "ringer."[11]
Types
Types of glucose/dextrose include:
- D5W (5% dextrose in water), which consists of 278 mmol/L dextrose
- D5NS (5% dextrose in normal saline), which, in addition, contains normal saline (0.9% w/v of NaCl).
- D5 1/2NS 5% dextrose in half amount of normal saline (0.45% w/v of NaCl).[12]
- D5LR (5% dextrose in lactated Ringer solution)
- D50 - 50% dextrose in water
The percentage is a mass percentage, so a 5% glucose/dextrose solution contains 50 g/L of glucose/dextrose (5g/100ml).
Glucose provides energy 4 kcal/gram, so a 5% glucose solution provides 0.2 kcal/ml. If prepared from dextrose monohydrate, which provides 3.4 kcal/gram, a 5% solution provides 0.17 kcal/ml.[13]
References
- "Dextrose". The American Society of Health-System Pharmacists. Archived from the original on 18 January 2017. Retrieved 8 January 2017.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. pp. 683–684. ISBN 9780857111562.
- WHO Model Formulary 2008 (PDF). World Health Organization. 2009. p. 491. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 January 2017.
- David, Suresh S. (2016). Clinical Pathways in Emergency Medicine. Springer. p. 62. ISBN 9788132227106. Archived from the original on 16 January 2017.
- Waldmann, Carl; Soni, Neil; Rhodes, Andrew (2008). Oxford Desk Reference: Critical Care. OUP Oxford. p. 142. ISBN 9780199229581. Archived from the original on 16 January 2017.
- Skipper, Annalynn (2012). Dietitian's Handbook of Enteral and Parenteral Nutrition. Jones & Bartlett Publishers. p. 283. ISBN 9780763742904. Archived from the original on 16 January 2017.
- Nelms, Marcia; Sucher, Kathryn (2015). Nutrition Therapy and Pathophysiology. Cengage Learning. p. 89. ISBN 9781305446007. Archived from the original on 16 January 2017.
- World Health Organization (2019). "World Health Organization model list of essential medicines: 21st list 2019". World Health Organization (WHO). hdl:10665/325771. Cite journal requires
|journal=(help) - "Dextrose 10% in Water". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- "Dextrose 5% in Sodium Chloride 0.9%". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- Jiha Ham (20 March 2015). "A Life Upended After an IV Glucose Treatment Popular Among Asian Immigrants". The New York Times. Archived from the original on 22 March 2015. Retrieved 21 March 2015.
Although many doctors warn Asian immigrants in New York that the effects of injecting glucose differ little from drinking sugary water, many Asians, especially of older generations, still use the intravenous solution. In their homelands, it is commonly prescribed by doctors as a method to cure colds, fevers and sometimes an upset stomach.
- eMedicine > Hypernatremia: Treatment & Medication Archived 2011-03-02 at the Wayback Machine By Ivo Lukitsch and Trung Q Pham. Updated: Apr 19, 2010
- Calculating Parenteral Feedings Archived 2010-12-03 at the Wayback Machine D. Chen-Maynard at California State University, San Bernardino. Retrieved September 2010. HSCI 368
External links
- "Dextrose". Drug Information Portal. U.S. National Library of Medicine.