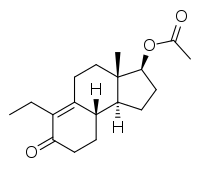
Inocoterone acetate
Inocoterone acetate (USAN) (developmental code names RU-38882, RU-882) is a steroid-like nonsteroidal antiandrogen (NSAA) that was developed for topical administration to treat acne but was never marketed.[1][2] It is the acetate ester of inocoterone, which is less potent in comparison.[3] Inocoterone acetate is actually not a silent antagonist of the androgen receptor but rather a weak partial agonist, similarly to steroidal antiandrogens like cyproterone acetate.[4]
 | |
| Clinical data | |
|---|---|
| Other names | RU-38882; RU-882; 2,5-Seco-A-dinorestr-9-en-17β-ol-5-one 17β-acetate |
| Drug class | Nonsteroidal antiandrogen |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C18H26O3 |
| Molar mass | 290.403 g/mol g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Inocoterone acetate was investigated for the treatment of acne but showed only modest (albeit statistically significant) efficacy in clinical trials.[2][5][6] A reduction of 26% of lesions was observed in males treated with the drug after 16 weeks (~3.7 months).[6][1] However, this is notably far less than that achieved with other agents such as benzoyl peroxide or antibiotics, which produce 50–75% reductions within 2 months.[1] Similar poor results with the topical route have disappointingly been found for other antiandrogens such as cyproterone acetate and spironolactone.[1] Similarly to rosterolone, inocoterone acetate has no systemic antiandrogenic activity when applied systemically.[7]
| Antiandrogen | AR | PR | ER | GR | MR |
|---|---|---|---|---|---|
| Cyproterone acetate | 8–10 | 60 | <0.1 | 5 | 1 |
| Chlormadinone acetate | 5 | 175 | <0.1 | 38 | 1 |
| Megestrol acetate | 5 | 152 | <0.1 | 50 | 3 |
| Spironolactone | 7 | 0.4a | <0.1 | 2a | 182 |
| Trimethyltrienolone | 3.6 | <1 | <1 | <1 | <1 |
| Inocoterone | 0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Inocoterone acetate | <0.1 | <0.1 | <0.1 | <0.1 | <0.1 |
| Flutamide | <0.1 | <0.1 | <0.1 | <0.1 | <0.1 |
| Hydroxyflutamide | 0.5–0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Nilutamide | 0.5–0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Bicalutamide | 1.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Notes: (1): Reference ligands (100%) were testosterone for the AR, progesterone for the PR, estradiol for the ER, dexamethasone for the GR, and aldosterone for the MR. (2): Tissues were rat prostate (AR), rabbit uterus (PR), mouse uterus (ER), rat thymus (GR), and rat kidney (MR). (3): Incubation times (0°C) were 24 hours (AR, a), 2 hours (PR, ER), 4 hours (GR), and 1 hour (MR). (4): Assay methods were different for bicalutamide for receptors besides the AR. Sources: See template. | |||||
References
- Richard A. Helms; David J. Quan (2006). Textbook of Therapeutics: Drug and Disease Management. Lippincott Williams & Wilkins. pp. 211–. ISBN 978-0-7817-5734-8.
- Bentham Science Publishers (September 1999). Current Pharmaceutical Design. Bentham Science Publishers. pp. 717–.
- Annual Reports in Medicinal Chemistry. Academic Press. 2 September 1987. pp. 203–. ISBN 978-0-08-058366-2.
- Térouanne B, Tahiri B, Georget V, Belon C, Poujol N, Avances C, Orio F, Balaguer P, Sultan C (2000). "A stable prostatic bioluminescent cell line to investigate androgen and antiandrogen effects". Mol. Cell. Endocrinol. 160 (1–2): 39–49. doi:10.1016/s0303-7207(99)00251-8. PMID 10715537.
- Leo Plouffe, Jr; Botros R. M. B. Rizk (25 June 2015). Androgens in Gynecological Practice. Cambridge University Press. pp. 84–. ISBN 978-1-316-29887-9.
- Lookingbill, D. P. (1992). "Inocoterone and acne. The effect of a topical antiandrogen: results of a multicenter clinical trial". Archives of Dermatology. 128 (9): 1197–1200. doi:10.1001/archderm.128.9.1197. ISSN 0003-987X.
- Neumann, F.; Töpert, M. (1990). "Antiandrogens and Hair Growth: Basic Concepts and Experimental Research": 791–826. doi:10.1007/978-3-642-74612-3_34. Cite journal requires
|journal=(help)