Injection (medicine)
Injection (often referred to as a "shot" in US English, or a "jab" in UK English) is the act of putting a liquid, especially a drug, into a person's body using a needle (usually a hypodermic needle) and a syringe.[1] Injection is a technique for delivering drugs by parenteral administration, that is, administration via a route other than through the digestive tract. Parenteral injection includes subcutaneous, intramuscular, intravenous, intraperitoneal, intracardiac, intraarticular, and intracavernous injection.
Injection is generally administered as a bolus, but can possibly be used for continuous drug administration as well.[2] The medication may be long-acting even when administered as a bolus and is then called depot injection. Administration by an indwelling catheter is generally preferred instead of injection in case of more long-term or recurrent drug administration.
Injections are among the most common health care procedures, with at least 16 billion administered in developing and transitional countries each year.[3] 95% of injections are administered in curative care, 3% are for immunization, and the rest for other purposes, such as blood transfusions.[3] In some instances the term injection is used synonymously with inoculation even by different workers in the same hospital. This should not cause confusion; the focus is on what is being injected/inoculated, not the terminology of the procedure.
Since the process imparts a small puncture wound to the body (with varying degrees of pain depending on injection type and location, medication type, needle gauge, the skill of the individual administering the injection and the sensitivity of the individual being injected), fear of needles is a common phobia and proper antiseptic measures should be used.
Types of Injections
Intravenous injection
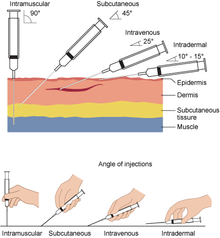
Intravenous injections (IV injections) involve needle insertion directly into the vein and the substance is directly delivered into the bloodstream.[4] In medicine and drug use, this route of administration is the fastest way to get the desired effects since the medication moves immediately into blood circulation and to the rest of the body.[5] This type of injection is the most common and often associated with illicit drug use because of the rapid effects.[6][7]
Intramuscular injection
Intramuscular injections (IM injections) deliver a substance deep into a muscle, where they are quickly absorbed by blood vessels. Common injections sites include the deltoid, vastus lateralis, and ventrogluteal muscles.[8] Most inactivated vaccines, like influenza, are given by IM injection.[9] Some medications are formulated for IM injection, like Epinephrine autoinjectors. Medical professionals are trained to give IM injections, but patients can also be trained to self-administer medications like epinephrine.
Subcutaneous injection
In a subcutaneous injection (SQ injections), the medication is delivered to the tissues between the skin and the muscle.[10] Absorption of the medicine is slower than that of intramuscular injection. Since the needle does not need to reach the muscles, often a bigger gauge and shorter needle is used. Usual site of administration is fat tissues behind the arm. Certain intramuscular injection medicines such as EpiPen® can also be used subcutaneously.[11] Insulin injection is a common type of subcutaneous injection medicine. Certain vaccines including MMR (Measles, Mumps, Rubella), Varicella (Chickenpox), Zoster (Shingles) are given subcutaneously.[12]
Intradermal injection

In an intradermal injection, medication is delivered directly into the dermis, the layer just below the epidermis of the skin. The injection is often given at a 5 to 15 degree angle with the needle placed almost flat against the patient's skin. Absorption takes the longest from this route compared to intravenous, intramuscular, and subcutaneous injections. Because of this, intradermal injection are often used for sensitivity tests, like tuberculin and allergy tests, and local anesthesia tests. The reactions caused by these tests are easily seen due to the location of the injections on the skin.[13]
Common sites of intradermal injections are the forearm and lower back.
Depot injection
A depot injection is an injection, usually subcutaneous, intradermal, or intramuscular, that deposits a drug in a localized mass, called a depot, from which it is gradually absorbed by surrounding tissue. Such injection allows the active compound to be released in a consistent way over a long period. Depot injections are usually either solid or oil-based. Depot injections may be available as certain forms of a drug, such as decanoate salts or esters. Examples of depot injections include Depo Provera and haloperidol decanoate. Prostate cancer patients receiving hormone therapy usually get depot injections as a treatment or therapy. Zoladex is an example of a medication delivered by depot for prostate cancer treatment or therapy. Naltrexone may be administered in a monthly depot injection to control opioid abuse; in this case, the depot injection improves compliance by replacing daily pill administration.
The advantages of using a long-acting depot injection include increased medication compliance due to reduction in the frequency of dosing, as well as more consistent serum concentrations. A significant disadvantage is that the drug is not immediately reversible, since it is slowly released.
In psychiatric nursing, a short acting depot, zuclopenthixol acetate, which lasts in the system from 24–72 hours, is more regularly used for rapid tranquillisation.[14]
Infiltration injection
The pharmaceutical injection type of infiltration involves loading a volume of tissue with the drug, filling the interstitial space. Local anesthetics are often infiltrated into the dermis and hypodermis.
Injection pain
The pain of an injection may be lessened by prior application of ice or topical anesthetic, or simultaneous pinching of the skin. Recent studies suggest that forced coughing during an injection stimulates a transient rise in blood pressure which inhibits the perception of pain.[15] Sometimes, as with an amniocentesis, a local anesthetic is given.[16] The most common technique to reduce the pain of an injection is simply to distract the patient.
Babies can be distracted by giving them a small amount of sweet liquid, such as sugar solution [17], or comforted by breastfeeding [18] during the injection, which reduces crying.
Injection hygiene
Proper needle technique and hygiene is important to perform injections safely for patients and healthcare personnel.[19] A new, sterile needle should be used each time, as needles get duller and more damaged with each use and reusing needles increases risk of infection. Needles should not be shared between people, as this increases risk of transmitting blood-borne pathogens. This can lead to infections and even lifelong disease.
In addition, multi-use medication bags, bottles, syringes, and ampules should not be entered with used needles. This practice also increases the risk of disease transmission between people sharing the same medication.[19]
Aseptic technique should always be practiced when administering injections. Aseptic practices and procedures include barriers such as gloves, gowns and masks for health care providers, sterile instruments (needles, syringes, etc.) and equipment, contact guidelines to avoid touching non-sterile surfaces with sterile items, and environmental controls.[20]
Needles should be disposed of in sharps containers. This reduces the risk of accidental needle sticks and exposure to other people.[21] Sharps containers should be closed once they are 3/4 full and seal with duct tape.[22] In the United States, there are 39 states that participate in programs to provide needle or syringe exchange programs.[23] If living in a state with a sharps take back program, the sharps container may be taken to the take back center for disposal. Otherwise, it should be placed in the center of a full trash bag. In the state of Ohio, sharps are allowed to be put in the regular trash. Some medicine companies provide mail-back sharps programs.[22]
Injection safety
Risks of Unsafe Injections
Unsafe injection practices can be attributed to at least 49 disease outbreaks since 2001. Contamination of needles at the point of administration can lead to transmission of Hepatitis B and C, HIV, and bloodstream infections.[24] Drug users have high rates of unsafe needle use including sharing needles between people.[25] The reuse of needles puts people at risk for disease.[26][27] The spread of HIV, Hepatitis B, and Hepatitis C from injection drug use is a worldwide issue.[28] In North America in 1994, over half of HIV cases were the result of drug use and unsafe iunjection practices.[6]
Another risk is poor collection and disposal of dirty injection equipment, which exposes healthcare workers and the community to the risk of needle stick injuries. In some countries, unsafe disposal can lead to re-sale of used equipment on the black market. Many countries have legislation or policies that mandate that healthcare professionals use a safety syringe (safety engineered needle) or alternative methods of administering medicines whenever possible.
Open burning of syringes, which is considered unsafe by the World Health Organization, is reported by half of the non-industrialized countries.[3]
According to one study, unsafe injections cause an estimated 1.3 million early deaths each year.[29]
To improve injection safety, the WHO recommends:[30]
- Changing the behavior of health care workers and patients
- Ensuring the availability of equipment and supplies
- Managing waste safely and appropriately
A needle tract infection is an infection that occurs when pathogenic micro-organisms are seeded into the tissues of the body during an injection.[31] Such infections are also referred to as needlestick infections.
Improvements to Injection Safety
An important movement in injection safety is the rising prevalence of supervised injection sites. These sites not only provide clean needles to mitigate infection risk, they also provide a safe space with clinicians and life saving support if needed. In an event of an overdose a clinician would be able to administer life saving support including medications such as naloxone, an opioid antagonist, used as an antidote in opioid overdose situations. Safe injection site are associated with lower overdose mortality, ambulance calls, and HIV infections.[32]
Ten countries around the world currently use safe injection sites, also called supervised consumption services. These include Australia, Canada, Denmark, France, Germany, Luxembourg, The Netherlands, Norway, Spain and Switzerland. In total, there are about 120 sites operating.[33] Although the United States does not currently have any safe injection sites, some cities such San Francisco, Philadelphia, and Denver are considering opening them.[23] In 2018, the California State Assembly attempted to pass Assembly Bill 186 to launch a three year pilot program in San Francisco for California's first safe injection sites.[34] Colorado and Pennsylvania are not too far behind, expressing their interests in launching safe injection sites. Recent rulings in Pennsylvania have determined that safe injection sites are not unlawful under the federal law.[35]
In nature
Many species of animals, and some stinging plants, have developed poison-injecting devices for self-defence or catching prey, for example:
- Venomous snakes
- Stinging insects
- Weevers (a fish)
- Sting rays
- Bloodsucking insects: some of them first inject an anticoagulant to make feeding easier
- Cnidocyte cells in the animals called cnidaria
- Stinging nettles
See also
- Dart injection
- Jet injector
- Injection port
- Lethal injection
- Needlestick injury
- Needle remover
- Safety syringe
References
- "injection". Cambridge dictionary. Retrieved 2017-07-30.
- St Charles M, Lynch P, Graham C, Minshall ME (2009). "A cost-effectiveness analysis of continuous subcutaneous insulin injection versus multiple daily injections in type 1 diabetes patients: a third-party US payer perspective". Value in Health. 12 (5): 674–86. doi:10.1111/j.1524-4733.2008.00478.x. PMID 19171006.
- "Injection safety". Health Topics A to Z. World Health Organization. Retrieved 2011-05-09.
- "Handbook of Basic Pharmacokinetics … Including Clinical Applications, Seventh Edition", Handbook of Basic Pharmacokinetics? Including Clinical Applications, 7th Edition, The American Pharmacists Association, 2009-01-01, doi:10.21019/9781582121260.ch6, ISBN 978-1-58212-126-0
|chapter=ignored (help) - Fan, Jianghong; de Lannoy, Inés A. M. (2014-01-01). "Pharmacokinetics". Biochemical Pharmacology. Special Issue: Pharmacology in 21st Century Biomedical Research. 87 (1): 93–120. doi:10.1016/j.bcp.2013.09.007. ISSN 0006-2952. PMID 24055064.
- Schoener, Eugene P; Hopper, John A; Pierre, James D (2002-09-01). "Injection drug use in North America". Infectious Disease Clinics of North America. 16 (3): 535–551. doi:10.1016/S0891-5520(02)00010-7. ISSN 0891-5520. PMID 12371114.
- Pieper, Barbara; Kirsner, Robert S.; Templin, Thomas N.; Birk, Thomas J. (2007-10-01). "Injection Drug Use: An Understudied Cause of Venous Disease". Archives of Dermatology. 143 (10): 1305–9. doi:10.1001/archderm.143.10.1305. ISSN 0003-987X. PMID 17938345.
- Mann E (2016). Injection (Intramuscular): Clinician Information. The Joanna Briggs Institute.
- Wolicki E, Weinbaum C, Weaver D (2017-10-04). "Pinkbook: Vaccine Administration: Epidemiology of VPDs". Centers for Disease Control and Prevention (CDC). Retrieved 2017-10-30.
- "What Is a Subcutaneous Injection?". Healthline. Retrieved 2017-11-15.
- EpiPen/EpiPen Jr (epinephrine) [prescribing information]. Morgantown, WV: Mylan Specialty LP; August 2018.
- "Administer the Vaccine(s)". Centers for Disease Control and Prevention (CDC). 2017-09-01. Retrieved 2017-11-15.
- Taylor CR, Lillis C, LeMone P, Lynn P (2011). Fundamentals of nursing: The art and science of nursing care. Philadelphia: Lippincott Williams & Wilkins. pp. 749, 788.
- Healy D (2016). Psychiatric Drugs Explained. Churchill Livingstone. p. 19. ISBN 978-0-7020-4688-9.
- Usichenko TI, Pavlovic D, Foellner S, Wendt M (February 2004). "Reducing venipuncture pain by a cough trick: a randomized crossover volunteer study". Anesthesia and Analgesia. 98 (2): 343–5, table of contents. doi:10.1213/01.ANE.0000094983.16741.AF. PMID 14742367.
- Usichenko TI, Pavlovic D, Foellner S, Wendt M (February 2004). "Reducing venipuncture pain by a cough trick: a randomized crossover volunteer study". Anesthesia and Analgesia. 98 (2): 343–5, table of contents. doi:10.1213/01.ane.0000094983.16741.af. PMID 14742367.
- Harrison D, Stevens B, Bueno M, Yamada J, Adams-Webber T, Beyene J, Ohlsson A (June 2010). "Efficacy of sweet solutions for analgesia in infants between 1 and 12 months of age: a systematic review". Archives of Disease in Childhood. 95 (6): 406–13. doi:10.1136/adc.2009.174227. PMID 20463370.
- Harrison, Denise; Reszel, Jessica; Bueno, Mariana; Sampson, Margaret; Shah, Vibhuti S; Taddio, Anna; Larocque, Catherine; Turner, Lucy (2016-10-28). "Breastfeeding for procedural pain in infants beyond the neonatal period". Cochrane Database of Systematic Reviews. 10: CD011248. doi:10.1002/14651858.cd011248.pub2. ISSN 1465-1858. PMC 6461192. PMID 27792244.
- "Background | Injection Safety | CDC". www.cdc.gov. 2019-06-20. Retrieved 2019-11-02.
- "Aseptic Technique: Uses, Benefits, and Complications". Healthline. Retrieved 2019-11-02.
- Grimmond T, Naisoro W (September 2014). "Sharps injury reduction: a six-year, three-phase study comparing use of a small patient-room sharps disposal container with a larger engineered container". Journal of Infection Prevention. 15 (5): 170–174. doi:10.1177/1757177414543088. PMC 5074232. PMID 28989381.
- "Sharps Containers at Home". www.nationwidechildrens.org. Retrieved 2019-11-21.
- "Supervised injection sites are coming to the United States. Here's what you should know". nursing.usc.edu. 2019-05-02. Retrieved 2019-11-14.
- "CDC Grand Rounds: Preventing Unsafe Injection Practices in the U.S. Health-Care System". www.cdc.gov. Retrieved 2019-10-22.
- Des Jarlais, D. C.; Friedman, S. R.; Stoneburner, R. L. (January 1988). "HIV infection and intravenous drug use: critical issues in transmission dynamics, infection outcomes, and prevention". Reviews of Infectious Diseases. 10 (1): 151–158. doi:10.1093/clinids/10.1.151. ISSN 0162-0886. PMID 3281219.
- "A Patient Safety Threat – Syringe Reuse: Injection Safety". Centers for Disease Control and Prevention (CDC). 2019-04-26. Retrieved 2019-10-23.
- Fischer, Benedikt; Murphy, Yoko; Rudzinski, Katherine; MacPherson, Donald (2016-01-01). "Illicit drug use and harms, and related interventions and policy in Canada: A narrative review of select key indicators and developments since 2000". International Journal of Drug Policy. 27: 23–35. doi:10.1016/j.drugpo.2015.08.007. ISSN 0955-3959. PMID 26359046.
- Degenhardt, Louisa; Whiteford, Harvey A.; Ferrari, Alize J.; Baxter, Amanda J.; Charlson, Fiona J.; Hall, Wayne D.; Freedman, Greg; Burstein, Roy; Johns, Nicole; Engell, Rebecca E.; Flaxman, Abraham (2013-11-09). "Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010". The Lancet. 382 (9904): 1564–1574. doi:10.1016/S0140-6736(13)61530-5. ISSN 0140-6736. PMID 23993281.
- Miller MA, Pisani E (1999). "The cost of unsafe injections". Bulletin of the World Health Organization. 77 (10): 808–11. PMC 2557745. PMID 10593028.
- "Injection Safety, First do no harm" (PDF). Advocacy brochure. World Health Organization. Retrieved 2011-05-09.
- Connor JP, Edelson JG (April 1988). "Needle tract infection. A case report". Oral Surgery, Oral Medicine, and Oral Pathology. 65 (4): 401–3. doi:10.1016/0030-4220(88)90351-9. PMID 3163131.
- Ng J, Sutherland C, Kolber MR (November 2017). "Does evidence support supervised injection sites?". Canadian Family Physician. 63 (11): 866. PMC 5685449. PMID 29138158.
- "Supervised Consumption Services". Drug Policy Alliance. Retrieved 2019-11-21.
- "Supervised injection sites are coming to the United States. Here's what you should know". nursing.usc.edu. 2019-05-02. Retrieved 2019-10-23.
- Allyn B. "Judge McHugh's Federal Ruling on Safehouse". www.documentcloud.org. Retrieved 2019-10-23.
External links
| Wikimedia Commons has media related to Injections (medicine). |
- Information about injections from the Merck Manual
- Information about intradermal injections
- FDA Center for Drug Evaluation and Research Data Standards Manual: Route of Administration
- Revolutions Medical Corp Retractable Syringe
- Revolutions Medical Corp RevVac™ Retracting Safety Syringe Demonstration
-solution.jpg)

