Hypertriglyceridemia
Hypertriglyceridemia denotes high (hyper-) blood levels (-emia) of triglycerides, the most abundant fatty molecule in most organisms. Elevated levels of triglycerides are associated with atherosclerosis, even in the absence of hypercholesterolemia (high cholesterol levels), and predispose to cardiovascular disease. Very high triglyceride levels also increase the risk of acute pancreatitis. Hypertriglyceridemia itself is usually symptomless, although high levels may be associated with skin lesions known as xanthomas.[1]
| Hypertriglyceridemia | |
|---|---|
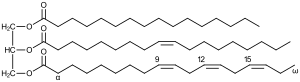 | |
| Triglyceride, which cause hypertriglyceridemia at high level | |
| Specialty | Endocrinology |
Signs and symptoms

Most people with elevated triglycerides experience no symptoms. Some forms of primary hypertriglyceridemia can lead to specific symptoms: both familial chylomicronemia and primary mixed hyperlipidemia include skin symptoms (eruptive xanthoma), eye abnormalities (lipemia retinalis), hepatosplenomegaly (enlargement of the liver and spleen), and neurological symptoms. Some experience attacks of abdominal pain that may be mild episodes of pancreatitis. Eruptive xanthomas are 2–5 mm papules, often with a red ring around them, that occur in clusters on the skin of the trunk, buttocks and extremities.[2] Familial dysbetalipoproteinemia causes larger, tuberous xanthomas; these are red or orange and occur on the elbows and knees. Palmar crease xanthomas may also occur.[1][2]
The diagnosis is made on blood tests, often performed as part of screening. Once diagnosed, other blood tests are usually required to determine whether the raised triglyceride level is caused by other underlying disorders ("secondary hypertriglyceridemia") or whether no such underlying cause exists ("primary hypertriglyceridaemia"). There is a hereditary predisposition to both primary and secondary hypertriglyceridemia.[1]
Acute pancreatitis may occur in people whose triglyceride levels are above 1000 mg/dL (11.3 mmol/L).[1][2][3] Hypertriglyceridemia is associated with 1–4% of all cases of pancreatitis. The symptoms are similar to pancreatitis secondary to other causes, although the presence of xanthomas or risk factors for hypertriglyceridemia may offer clues.[3]
Causes
- Overeating[4][5]
- Obesity
- Diabetes mellitus and insulin resistance - it is one of the defined components of metabolic syndrome (along with central obesity, hypertension, and hyperglycemia)
- Excess alcohol consumption
- Kidney failure, nephrotic syndrome
- Genetic predisposition; some forms of familial hyperlipidemia such as familial combined hyperlipidemia i.e. Type II hyperlipidemia
- Lipoprotein lipase deficiency - Deficiency of this water-soluble enzyme, that hydrolyzes triglycerides in lipoproteins, leads to elevated levels of triglycerides in the blood.
- Lysosomal acid lipase deficiency or Cholesteryl ester storage disease
- Certain medications e.g. isotretinoin, hydrochlorothiazide diuretics, beta blockers, protease inhibitors
- Hypothyroidism (underactive thyroid)
- Systemic Lupus Erythematosus and associated autoimmune responses [6]
- Glycogen storage disease type 1.
- Propofol
- HIV medications
Diagnosis
The diagnosis is made on blood tests, often performed as part of screening. The normal triglyceride level is less than 150 mg/dL (1.7 mmol/L).[1][5] Once diagnosed, other blood tests are usually required to determine whether the raised triglyceride level is caused by other underlying disorders ("secondary hypertriglyceridemia") or whether no such underlying cause exists ("primary hypertriglyceridaemia"). There is a hereditary predisposition to both primary and secondary hypertriglyceridemia.[1]
Screening
In 2016 the United States Preventive Services Task Force concluded that testing the general population under the age of 40 without symptoms is of unclear benefit.[7][8]
Treatment
Lifestyle changes including weight loss and dietary modification may improve hypertriglyceridemia. The decision to treat hypertriglyceridemia with medication depends on the levels and on the presence of other risk factors for cardiovascular disease. Very high levels that would increase the risk of pancreatitis is treated with a drug from the fibrate class. Niacin and omega-3 fatty acids as well as drugs from the statin class may be used in conjunction, with statins being the main drug treatment for moderate hypertriglyceridemia where reduction of cardiovascular risk is required.[1]
Lifestyle changes
Weight loss and dietary modification are effective first-line lifestyle modification treatments for hypertriglyceridemia.[9] For people with mildly or moderately high levels of triglycerides lifestyle changes including weight loss, moderate exercise,[10] and dietary modification are recommended.[1] This may include restriction of carbohydrates (specifically fructose)[9] and fat in the diet and the consumption of omega-3 fatty acids from algae, nuts, and seeds.[11][12]
Medications
Medications are recommended in those with high levels of triglycerides that are not corrected with lifestyle modifications, with fibrates being recommended first.[1][13][14] Epanova (omega-3-carboxylic acids) is another prescription drug used to treat very high levels of blood triglycerides.[15]
The decision to treat hypertriglyceridemia with medication depends on the levels and on the presence of other risk factors for cardiovascular disease. Very high levels that would increase the risk of pancreatitis is treated with a drug from the fibrate class. Niacin and omega-3 fatty acids as well as drugs from the statin class may be used in conjunction, with statins being the main medication for moderate hypertriglyceridemia when reduction of cardiovascular risk is required.[1]
Epidemiology
As of 2006, the prevalence of hypertriglyceridemia in the United States was 30%.[5]
See also
- Remnant cholesterol
References
- Berglund L, Brunzell JD, Goldberg AC, et al. (September 2012). "Evaluation and treatment of hypertriglyceridemia: an endocrine society clinical practice guideline". J. Clin. Endocrinol. Metab. 97 (9): 2969–89. doi:10.1210/jc.2011-3213. PMC 3431581. PMID 22962670.
- Yuan G, Al-Shali KZ, Hegele RA (April 2007). "Hypertriglyceridemia: its etiology, effects and treatment". CMAJ. 176 (8): 1113–20. doi:10.1503/cmaj.060963. PMC 1839776. PMID 17420495.
- Tsuang W, Navaneethan U, Ruiz L, Palascak JB, Gelrud A (April 2009). "Hypertriglyceridemic pancreatitis: presentation and management". Am. J. Gastroenterol. 104 (4): 984–91. doi:10.1038/ajg.2009.27. PMID 19293788.
- Garg, A; Grundy, SM; Unger, RH (Oct 1992). "Comparison of effects of high and low carbohydrate diets on plasma lipoproteins and insulin sensitivity in patients with mild NIDDM". Diabetes. 41 (10): 1278–85. doi:10.2337/diabetes.41.10.1278. PMID 1397701.
- Pejic RN, Lee DT (May–Jun 2006). "Hypertriglyceridemia". J Am Board Fam Med. 19 (3): 310–6. doi:10.3122/jabfm.19.3.310. PMID 16672684.
- Beigneux, Anne P.; Miyashita, Kazuya; Ploug, Michael; Blom, Dirk J.; Ai, Masumi; Linton, Macrae F.; Khovidhunkit, Weerapan; Dufour, Robert; Garg, Abhimanyu; McMahon, Maureen A.; Pullinger, Clive R.; Sandoval, Norma P.; Hu, Xuchen; Allan, Christopher M.; Larsson, Mikael; Machida, Tetsuo; Murakami, Masami; Reue, Karen; Tontonoz, Peter; Goldberg, Ira J.; Moulin, Philippe; Charrière, Sybil; Fong, Loren G.; Nakajima, Katsuyuki; Young, Stephen G. (August 27, 2017). "Autoantibodies against GPIHBP1 as a Cause of Hypertriglyceridemia". NEJM. 376 (17): 1647–1658. doi:10.1056/NEJMoa1611930. PMC 5555413. PMID 28402248.
- Chou, Roger; Dana, Tracy; Blazina, Ian; Daeges, Monica; Bougatsos, Christina; Jeanne, Thomas L. (9 August 2016). "Screening for Dyslipidemia in Younger Adults: A Systematic Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 165 (8): 560–564. doi:10.7326/M16-0946. PMID 27538032.
- Bibbins-Domingo, Kirsten; Grossman, David C.; Curry, Susan J.; Davidson, Karina W.; Epling, John W.; García, Francisco A. R.; Gillman, Matthew W.; Kemper, Alex R.; Krist, Alex H.; Kurth, Ann E.; Landefeld, C. Seth; Lefevre, Michael; Mangione, Carol M.; Owens, Douglas K.; Phillips, William R.; Phipps, Maureen G.; Pignone, Michael P.; Siu, Albert L. (August 9, 2016). "Screening for Lipid Disorders in Children and Adolescents". JAMA. 316 (6): 625. doi:10.1001/jama.2016.9852. PMID 27532917.
- Nordestgaard, BG; Varbo, A (August 2014). "Triglycerides and cardiovascular disease". The Lancet. 384 (9943): 626–635. doi:10.1016/S0140-6736(14)61177-6. PMID 25131982.
- GILL, Jason; Sara HERD; Natassa TSETSONIS; Adrianne HARDMAN (Feb 2002). "Are the reductions in triacylglycerol and insulin levels after exercise related?". Clinical Science. 102 (2): 223–231. doi:10.1042/cs20010204. PMID 11834142.
- Davidson, Michael H. (28 January 2008). "Pharmacological Therapy for Cardiovascular Disease". In Davidson, Michael H.; Toth, Peter P.; Maki, Kevin C. (eds.). Therapeutic Lipidology. Contemporary Cardiology. Cannon, Christopher P.; Armani, Annemarie M. Totowa, New Jersey: Humana Press, Inc. pp. 141–142. ISBN 978-1-58829-551-4.
- Anagnostis, P; Paschou, SA; Goulis, DG; Athyros, VG; Karagiannis, A (February 2018). "Dietary management of dyslipidaemias. Is there any evidence for cardiovascular benefit?". Maturitas. 108: 45–52. doi:10.1016/j.maturitas.2017.11.011. PMID 29290214.
- Abourbih S, Filion KB, Joseph L, Schiffrin EL, Rinfret S, Poirier P, Pilote L, Genest J, Eisenberg MJ (2009). "Effect of fibrates on lipid profiles and cardiovascular outcomes: a systematic review". Am J Med. 122 (10): 962.e1–962.e8. doi:10.1016/j.amjmed.2009.03.030. PMID 19698935.
- Jun M, Foote C, Lv J, et al. (2010). "Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis". Lancet. 375 (9729): 1875–1884. doi:10.1016/S0140-6736(10)60656-3. PMID 20462635.
- Blair HA, Dhillon S. Omega-3 carboxylic acids (Epanova): a review of its use in patients with severe hypertriglyceridemia. Am J Cardiovasc Drugs. 2014 Oct;14(5):393-400. PMID 25234378
External links
| Classification | |
|---|---|
| External resources |