Hyperinsulinemia
Hyperinsulinemia, is a condition in which there are excess levels of insulin circulating in the blood relative to the level of glucose. While it is often mistaken for diabetes or hyperglycaemia, hyperinsulinemia can result from a variety of metabolic diseases and conditions. While hyperinsulinemia is often seen in people with early stage type 2 diabetes mellitus, it is not the cause of the condition and is only one symptom of the disease. Type 1 diabetes only occurs when pancreatic beta-cell function is impaired. Hyperinsulinemia can be seen in a variety of conditions including diabetes mellitus type 2, in neonates and in drug induced hyperinsulinemia. It can also occur in congenital hyperinsulism, including nesidioblastosis.
| Hyperinsulinemia | |
|---|---|
| Other names | Hyperinsulinaemia |
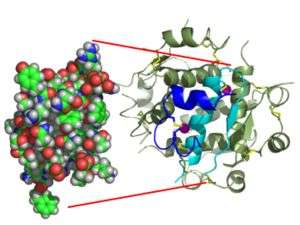 | |
| Insulin binding to its receptor | |
| Specialty | Endocrinology |
Hyperinsulinemia is associated with hypertension, obesity, dyslipidemia, and glucose intolerance.[1] These conditions are collectively known as Metabolic syndrome.[2] This close association between hyperinsulinemia and conditions of metabolic syndrome suggest related or common mechanisms of pathogenicity.[1] Hyperinsulinemia has been shown to "play a role in obese hypertension by increasing renal sodium retention".[1]
In type 2 diabetes, the cells of the body become resistant to the effects of insulin as the receptors which bind to the hormone become less sensitive to insulin concentrations resulting in hyperinsulinemia and disturbances in insulin release.[3] With a reduced response to insulin, the beta cells of the pancreas secrete increasing amounts of insulin in response to the continued high blood glucose levels resulting in hyperinsulinemia. In insulin resistant tissues, a threshold concentration of insulin is reached causing the cells to uptake glucose and therefore decreases blood glucose levels. Studies have shown that the high levels of insulin resulting from insulin resistance might enhance insulin resistance.[3]
Studies on mice with genetically reduced circulating insulin suggest that hyperinsulinemia plays a causal role in high fat diet-induced obesity. In this study, mice with reduced insulin levels expended more energy and had fat cells that were reprogrammed to burn some energy as heat.[4]
Hyperinsulinemia in neonates can be the result of a variety of environmental and genetic factors. If the mother of the infant is a diabetic, and does not properly control her blood glucose levels, the hyperglycemic maternal blood can create a hyperglycemic environment in the fetus. To compensate for the increased blood glucose levels, fetal pancreatic beta cells can undergo hyperplasia. The rapid division of beta cells results in increased levels of insulin being secreted to compensate for the high blood glucose levels. Following birth, the hyperglycemic maternal blood is no longer accessible to the neonate resulting in a rapid drop in the newborn’s blood glucose levels. As insulin levels are still elevated this may result in hypoglycemia. To treat the condition, high concentration doses of glucose are given to the neonate as required maintaining normal blood glucose levels. The hyperinsulinemia condition subsides after one to two days.[5]
Symptoms
There are often no visible symptoms of hyperinsulinemia unless hypoglycaemia (low blood sugar) is present.
Some patients may experience a variety of symptoms when hypoglycaemia is present, including:[6]
- Temporary muscle weakness
- Brain fog
- Fatigue
- Temporary thought disorder, or inability to concentrate
- Visual problems such as blurred vision or double vision
- Headaches
- Shaking/Trembling
- Thirst
If a person experiences any of these symptoms, a visit to a qualified medical practitioner is advised, and diagnostic blood testing may be required.
Causes
Possible causes include:
- Neoplasm
- Pancreatic cancer
- Polycystic ovary syndrome (PCOS)
- Trans fats [7]
Link to obesity
Since hyperinsulinemia and obesity are so closely linked it is hard to determine whether hyperinsulinemia causes obesity or obesity causes hyperinsulinemia, or both.
Obesity is characterized by an excess of adipose tissue – insulin increases the synthesis of fatty acids from glucose, facilitates the entry of glucose into adipocytes and inhibits breakdown of fat in adipocytes.[8]
On the other hand, adipose tissue is known to secrete various metabolites, hormones and cytokines that may play a role in causing hyperinsulinemia.[9] Specifically cytokines secreted by adipose tissue directly affect the insulin signalling cascade, and thus insulin secretion.[10] Adiponectins are cytokines that are inversely related to percent body fat; that is people with a low body fat will have higher concentrations of adiponectins where as people with high body fat will have lower concentrations of adiponectins. Weyer "et al,." (2011) reported that hyperinsulinemia is strongly associated with low adiponectin concentrations in obese people, though whether low adiponectin has a causal role in hyperinsulinemia remains to be established.[10]
- May lead to hypoglycemia or diabetes
- Increased risk of PCOS
- Increased synthesis of VLDL (hypertriglyceridemia)
- Hypertension (insulin increases sodium retention by the renal tubules)
- Coronary Artery Disease (increased insulin damages endothelial cells)
- Increased risk of cardiovascular disease
- Weight gain and lethargy (possibly connected to an underactive thyroid)
- Obesity and hyperinsulinemia have some links with some types of cancer[11][12]
Diagnosis
Diagnosis can be made by checking fasting and post prandial insulin levels either with normal meal or with 100g of oral glucose.
Treatment
Treatment is typically achieved via diet and exercise, although metformin may be used to reduce insulin levels in some patients (typically where obesity is present). A referral to a dietician is beneficial. Another method used to lower excessively high insulin levels is cinnamon as was demonstrated when supplemented in clinical human trials.[13]
A healthy diet that is low in simple sugars and processed carbohydrates, and high in fiber, and vegetable protein is often recommended. This includes replacing white bread with whole-grain bread, reducing intake of foods composed primarily of starch such as potatoes, and increasing intake of legumes and green vegetables, particularly soy.[14]
Regular monitoring of weight, blood sugar, and insulin are advised, as hyperinsulinemia may develop into diabetes mellitus type 2.
It has been shown in many studies that physical exercise improves insulin sensitivity.[15] The mechanism of exercise on improving insulin sensitivity is not well understood however it is thought that exercise causes the glucose receptor GLUT4 to translocate to the membrane.[16] As more GLUT4 receptors are present on the membrane more glucose is taken up into cells decreasing blood glucose levels which then causes decreased insulin secretion and some alleviation of hyperinsulinemia.[15] Another proposed mechanism of improved insulin sensitivity by exercise is through AMPK activity.[15] The beneficial effect of exercise on hyperinsulinemia was shown in a study by Solomon et al. (2009), where they found that improving fitness through exercise significantly decreases blood insulin concentrations.[15]
Common misconceptions
- Hyperinsulinemia is often mistaken for diabetes or hypoglycaemia. These are separate, albeit related, conditions. Treatment may overlap for these conditions, but medical advice should always be sought.
See also
- Metabolic syndrome (Syndrome X)
- Acanthosis nigricans
References
- Modan, Michaela; Halkin H; Almog S; Lusky A; Eshkol A; Shefi M; Shitrit A; Fuchs Z. (March 1985). "Hyperinsulinemia: A link between hypertension obesity and glucose intolerance". J. Clin. Invest. 75 (3): 809–17. doi:10.1172/JCI111776. PMC 423608. PMID 3884667.
- Danker, Rache; Chetrit A; Shanik MH; Raz I; Roth J (August 2009). "Basal-stat hyperinsulinemia in healthy normoglycemic adults is predictive of type 2 diabetes over a 24-year follow-up". Diabetes Care. 32 (8): 1464–66. doi:10.2337/dc09-0153. PMC 2713622. PMID 19435961.
- Shanik, M.H.; Yuping, X.; Skrha, J.; Danker, R.; Zick, Y.; Roth, J. (2008). "Insulin Resistance and Hyperinsulinemia". Diabetes Care. 31 (2): S262–68. doi:10.2337/dc08-s264. PMID 18227495.
- Mehran, Arya E.; Nicole M. Templeman; G. Stefano Brigidi; Gareth E. Lim; Kwan-Yi Chu; Xiaoke Hu; Jose Diego Botezelli; Ali Asadi; Bradford G. Hoffman; Timothy J. Kieffer; Shernaz X. Bamji; Susanne M. Clee; James D. Johnson (6 Dec 2012). "Hyperinsulinemia Drives Diet-Induced Obesity Independently of Brain Insulin Production". Cell Metabolism. 16 (5): 723–37. doi:10.1016/j.cmet.2012.10.019. PMID 23217255.
- Ferry, R.J. (2010). Hyperinsulinism "Medscape".
- Hyperinsulinemia
- Clément L, Poirier H, Niot I, Bocher V, Guerre-Millo M, Krief S, Staels B, Besnard P (2002). "mice fed a diet enriched in t10,c12-CLA (0.4% w/w) for 4 weeks developed lipoatrophy, hyperinsulinemia, and fatty liver, whereas diets enriched in c9,t11-CLA and LA had no significant effect ; from google (hyperinsulinemia trans fat) result 2". J Lipid Res. 43 (9): 1400–09. doi:10.1194/jlr.M20008-JLR200. PMID 12235171.
- Physiologic Effects of Insulin
- Matsuzawa, Y; Fanahashi T; Nakamura T (1999). "Moleculare mechanism of metabolic syndrome X: contribution of adiposcyte-derived bioactive substances". Annals of the New York Academy of Sciences. 892 (1): 146–54. Bibcode:1999NYASA.892..146M. doi:10.1111/j.1749-6632.1999.tb07793.x. PMID 10842660.
- Weyer, C; Funahachi T; Tanaka S; Hotta K; Matsuzawa Y; Pratley RE; Tataranni PA (2011). "Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia". The Journal of Clinical Endocrinology & Metabolism. 86 (5): 1930–35. doi:10.1210/jcem.86.5.7463. PMID 11344187.
- Poloz, Y.; Stambolic, V. (2015). "Obesity and cancer, a case for insulin signaling". Cell Death and Disease. 6 (12): e2037. doi:10.1038/cddis.2015.381. PMC 4720912. PMID 26720346.
- Vigneri, R.; Goldfine, I. D.; Frittitta, L. (2016). "Insulin, insulin receptors, and cancer". Journal of Endocrinological Investigation. 39 (12): 1365–1376. doi:10.1007/s40618-016-0508-7. PMID 27368923.
- Solomon, TP; Blannin, AK (November 2007). "Effects of short-term cinnamon ingestion on in vivo glucose tolerance". Diabetes, Obesity & Metabolism. 9 (6): 895–901. doi:10.1111/j.1463-1326.2006.00694.x. PMID 17924872.
- Villegas, R; Gao, YT; Yang, G; Li, HL; Elasy, TA; Zheng, W; Shu, XO (January 2008). "Legume and soy food intake and the incidence of type 2 diabetes in the Shanghai Women's Health Study". The American Journal of Clinical Nutrition. 87 (1): 162–7. doi:10.1093/ajcn/87.1.162. PMC 2361384. PMID 18175751.
- Solomon, Thomas P; Haus JM; Kelly KR; Cook MD; Riccardi M; Rocco M; Kashyap SR; Barkowkis H; Kirwan JP (2009). "Randomized trial on the effects of a 7-d low-glycemic diet and exercise intervention on insulin resistance in older obese humans". Am J Clin Nutr. 90 (5): 1222–29. doi:10.3945/ajcn.2009.28293. PMC 2762157. PMID 19793849.
- Lund, S; Holman GD; Schmitz O; Pedersen O (1995). "Contraction stimulates translocation of glucose transporter GLUT4 in skeletal muscle through a mechanism distinct from that of insulin". Proc. Natl. Acad. Sci. U.S.A. 92 (13): 5817–5821. Bibcode:1995PNAS...92.5817L. doi:10.1073/pnas.92.13.5817. PMC 41592. PMID 7597034.