Hyperaldosteronism
Hyperaldosteronism is a medical condition wherein too much aldosterone is produced by the adrenal glands, which can lead to lowered levels of potassium in the blood (hypokalemia) and increased hydrogen ion excretion (alkalosis).
| Hyperaldosteronism | |
|---|---|
| Other names | Aldosteronism[1] |
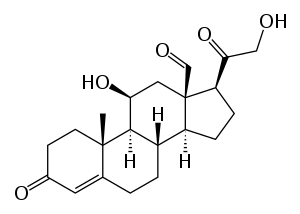 | |
| Aldosterone | |
| Specialty | Endocrinology |
This cause of mineralocorticoid excess is primary hyperaldosteronism reflecting excess production of aldosterone by adrenal zona glomerulosa. Bilateral micronodular hyperplasia is more common than unilateral adrenal adenoma.
Signs and symptoms
It can be asymptomatic, but these symptoms may be present:
- Fatigue
- Headache
- High blood pressure
- Hypokalemia
- Hypernatraemia
- Hypomagnesemia
- Intermittent or temporary paralysis
- Muscle spasms
- Muscle weakness
- Numbness
- Polyuria
- Polydipsia
- Tingling
- Metabolic alkalosis[2]
Cause
The causes of primary hyperaldosteronism are adrenal hyperplasia and adrenal adenoma (Conn's syndrome). These cause hyperplasia of aldosterone-producing cells of the adrenal cortex resulting in primary hyperaldosteronism. The causes of secondary hyperaldosteronism are massive ascites, left ventricular failure, and cor pulmonale. These act either by decreasing circulating fluid volume or by decreasing cardiac output, with resulting increase in renin release leading to secondary hyperaldosteronism. Secondary hyperaldosteronism can also be caused by Proximal renal tubular acidosis
Diagnosis
When taking a blood test, the aldosterone-to-renin ratio is abnormally increased in primary hyperaldosteronism, and decreased or normal but with high renin in secondary hyperaldosteronism.
Types
In endocrinology, the terms 'primary' and 'secondary' are used to describe the abnormality (e.g., elevated aldosterone) in relation to the defect, i.e., the tumor's location. Hyperaldosteronism can also be caused by plant poisoning, where the patient has been exposed to too much licorice. Licorice is a perennial herb that is used in making candies and in cooking other desserts because of its sweet taste. It contains the chemical glycyrrhizin, which has medicinal uses, but at higher levels it can be toxic. Through inhibition of 11-beta-hydroxysteroid dehydrogenase type 2 (11-beta-HSD2), glycyrrhizin allows cortisol to activate mineralocorticoid receptors (MR) in the kidney. This severely potentiates mineralocorticoid receptor mediated renal sodium reabsorbtion, due to much higher circulating concentrations of cortisol compared to aldosterone. This, in turn, expands the extracellular volume, increases total peripheral resistance and increases arterial blood pressure. The condition is termed pseudohyperaldosteronism.
Primary
Primary aldosteronism (hyporeninemic hyperaldosteronism) was previously thought to be most commonly caused by an adrenal adenoma, termed Conn's syndrome. However, recent studies have shown that bilateral idiopathic adrenal hyperplasia is the cause in up to 70% of cases. Differentiating between the two is important, as this determines treatment. Also see congenital adrenal hyperplasia. Adrenal carcinoma is an extremely rare cause of primary hyperaldosteronism. Two familial forms have been identified: type I (dexamethasone suppressible), and type II, which has been linked to the 7p22 gene.[3]
Features
- Hypertension
- Hypokalemia (e.g., may cause muscle weakness)
- Alkalosis
Investigations
- High serum aldosterone
- Low serum renin
- High-resolution CT abdomen
Management
- Adrenal adenoma: surgery
- Bilateral adrenocortical hyperplasia: aldosterone antagonist, e.g., spironolactone
Secondary
- Secondary hyperaldosteronism (also hyperreninism, or hyperreninemic hyperaldosteronism) is due to overactivity of the renin–angiotensin–aldosterone system (RAAS).
Secondary refers to an abnormality that indirectly results in pathology through a predictable physiologic pathway, i.e., a renin-producing tumor leads to increased aldosterone, as the body's aldosterone production is normally regulated by renin levels.
One cause is a juxtaglomerular cell tumor. Another is renal artery stenosis, in which the reduced blood supply across the juxtaglomerular apparatus stimulates the production of renin. Likewise, fibromuscular dysplasia may cause stenosis of the renal artery, and therefore secondary hyperaldosteronism. Other causes can come from the tubules: Hyporeabsorption of sodium (as seen in Bartter and Gitelman syndromes) will lead to hypovolemia/hypotension, which will activate the Renin–angiotensin system (RAAS).
Treatment
Treatment includes spironolactone, a potassium-sparing diuretic that works by acting as an aldosterone antagonist.
References
- "aldosteronism" at Dorland's Medical Dictionary
- "Hyperaldosteronism: eMedicine Pediatrics: General Medicine". Retrieved 2009-06-16.
- Lafferty AR, Torpy DJ, Stowasser M, et al. (November 2000). "A novel genetic locus for low renin hypertension: familial hyperaldosteronism type II maps to chromosome 7 (7p22)". J. Med. Genet. 37 (11): 831–5. doi:10.1136/jmg.37.11.831. PMC 1734468. PMID 11073536.
External links
| Classification | |
|---|---|
| External resources |