History of penicillin
The history of penicillin follows a number of observations and discoveries of apparent evidence of antibiotic activity in molds before the modern isolation of the chemical penicillin in 1928. There are anecdotes about ancient societies using molds to treat infections, and in the following centuries many people observed the inhibition of bacterial growth by various molds.[1] However, it is unknown if the species involved were Penicillium species or if the antimicrobial substances produced were penicillin.
The Scottish physician Alexander Fleming was the first to suggest that a Penicillium mold must secrete an antibacterial substance, and the first to concentrate the active substance involved, which he named penicillin, in 1928. Penicillin was the first modern antibiotic. During the next twelve years Fleming grew, distributed, and studied the original mold, which was determined to be a rare variant of Penicillium notatum (now Penicillium chrysogenum).[2][3]
Many later scientists were involved in the stabilization and mass production of penicillin and in the search for more productive strains of Penicillium.[4] Important contributors include Ernst Chain, Howard Florey, Norman Heatley, and Edward Abraham.[2] Shortly after the discovery of penicillin, scientists found that some disease-causing pathogens display antibiotic resistance to penicillin. Research that aims to develop more effective strains and to study the causes and mechanisms of antibiotic resistance continues today.[5][6]
Early history
Many ancient cultures, including those in Egypt, Greece, and India, independently discovered the useful properties of fungi and plants in treating infection.[7] These treatments often worked because many organisms, including many species of mold, naturally produce antibiotic substances. However, ancient practitioners could not precisely identify or isolate the active components in these organisms.
In 17th-century Poland, wet bread was mixed with spider webs (which often contained fungal spores) to treat wounds. The technique was mentioned by Henryk Sienkiewicz in his 1884 book With Fire and Sword. In England in 1640, the idea of using mold as a form of medical treatment was recorded by apothecaries such as John Parkinson, King's Herbarian, who advocated the use of mold in his book on pharmacology. [8]
Early scientific evidence
- NB
- In the early stages of penicillin research, most species of Penicillium were generally referred to as Penicillium glaucum, so we cannot identify the actual strains used. Thus, it is difficult to tell whether it was really penicillin preventing bacterial growth.[9]
The modern history of penicillin research begins in earnest in the 1870s, in the United Kingdom. Sir John Scott Burdon-Sanderson, who started out at St. Mary's Hospital (1852–1858) and later worked there as a lecturer (1854–1862), observed that culture fluid covered with mold would produce no bacterial growth. Burdon-Sanderson's discovery prompted Joseph Lister, an English surgeon and the father of modern antisepsis, to discover in 1871 that urine samples contaminated with mold also did not permit the growth of bacteria. Lister also described the antibacterial action on human tissue of a species of mold he called Penicillium glaucum.[10] A nurse at King's College Hospital whose wounds did not respond to any traditional antiseptic was then given another substance that cured her, and Lister's registrar informed her that it was called Penicillium. In 1874, the Welsh physician William Roberts, who later coined the term "enzyme", observed that bacterial contamination is generally absent in laboratory cultures of Penicillium glaucum. John Tyndall followed up on Burdon-Sanderson's work and demonstrated to the Royal Society in 1875 the antibacterial action of the Penicillium fungus.[11] By this time, Bacillus anthracis had been shown to cause anthrax, the first demonstration that a specific bacterium caused a specific disease.
In 1877, French biologists Louis Pasteur and Jules Francois Joubert observed that cultures of the anthrax bacilli, when contaminated with molds, could be successfully inhibited. Some references say that Pasteur identified the strain as Penicillium notatum.[12] However, Paul de Kruif's 1926 Microbe Hunters describes this incident as contamination by other bacteria rather than by mold.[13] In 1887, Garré found similar results. In 1895, Vincenzo Tiberio, an Italian physician at the University of Naples, published research about molds initially found in a water well in Arzano; in particular, from his observations he concluded that these molds contained soluble substances having antibacterial action.[14][15][16][17]
Two years later, Ernest Duchesne at École du Service de Santé Militaire in Lyon independently discovered the healing properties of a Penicillium glaucum mold, even curing infected guinea pigs of typhoid. He published a dissertation[18][19][20] in 1897 but it was ignored by the Institut Pasteur. Duchesne was himself using a discovery made earlier by Arab stable boys, who used molds to cure sores on horses. He did not claim that the mold contained any antibacterial substance, only that the mold somehow protected the animals. The penicillin isolated by Fleming does not cure typhoid and so it remains unknown which substance might have been responsible for Duchesne's cure.[lower-alpha 1]
In Belgium in 1920, Andre Gratia and Sara Dath observed a fungal contamination in one of their Staphylococcus aureus cultures that was inhibiting the growth of the bacterium. They identified the fungus as a species of Penicillium and presented their observations as a paper, but it received little attention. An Institut Pasteur scientist, Costa Rican Clodomiro Picado Twight, similarly recorded the antibiotic effect of Penicillium in 1923.
Modern breakthroughs
First isolation and successful treatment
In 1928, Scottish biologist Alexander Fleming noticed a halo of inhibition of bacterial growth around a contaminant blue-green mold on a Staphylococcus plate culture. He concluded that the mold was releasing a substance that was inhibiting bacterial growth. He grew a pure culture of the mold and subsequently concentrated what he later named "penicillin". He soon began treating infections in patients with penicillin. One of the first was his assistant Stuart Braddock. Fleming applied penicillin to his Sinus infection. Within three hours, most of the bacteria in the infected area had disappeared.[21] In 1929, he reported his findings in an article for The British Journal of Experimental Pathology.[22] During the next twelve years, Fleming grew and distributed the original mold, which was eventually identified as Penicillium notatum (now known as Penicillium chrysogenum). He was unsuccessful in making a stable form of it for mass production.[23] Although Fleming did some research with penicillin directly on patients and greatly contributed to its medical use, he did not realize its revolutionary potential, due to the impurity of the penicillin he made and the difficulty in mass producing it. Most of his further research with penicillin was focused mostly on the properties of penicillin rather than medical treatment with penicillin.[24]
Cecil George Paine, a pathologist at the Royal Infirmary in Sheffield, attempted to treat sycosis (eruptions in beard follicles) with penicillin but was unsuccessful, probably because the drug did not penetrate deep enough. Moving on to ophthalmia neonatorum, a gonococcal infection in babies, he achieved the first cure on 25 November 1930. He cured four patients (one adult, the others infants) of eye infections, although a fifth patient was not so lucky.[25]
Stabilization and mass production
At Oxford, Howard Walter Florey organized a large biochemical research team, notable among them Ernst Boris Chain and Norman Heatley, to undertake clinical trials and produce a stable penicillin in quantity.[26]
Between 1941 and 1943, Moyer, Coghill and Raper at the USDA Northern Regional Research Laboratory (NRRL) in Peoria, Illinois, United States, developed methods for industrialized penicillin production and isolated higher-yielding strains of the Penicillium fungus.[27] In December 1942, survivors of the Cocoanut Grove fire in Boston were the first burn patients to be successfully treated with penicillin.[28] Simultaneous research by Jasper H. Kane and other Pfizer scientists in Brooklyn developed the practical, deep-tank fermentation method for production of large quantities of pharmaceutical-grade penicillin.[29]
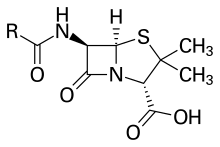
Dorothy Hodgkin determined the correct chemical structure of penicillin using X-ray crystallography at Oxford in 1945.[30][31][32][5] In Kundl, Tyrol, Austria, in 1952, Hans Margreiter and Ernst Brandl of Biochemie (now Sandoz) developed the first acid-stable penicillin for oral administration, Penicillin V.[33] American chemist John C. Sheehan of the Massachusetts Institute of Technology (MIT) subsequently completed the first chemical synthesis of penicillin in 1957.[34] The second-generation semi-synthetic β-lactam antibiotic methicillin, designed to counter first-generation-resistant penicillinases, was introduced in the United Kingdom in 1959. Methicillin-resistant forms of Staphylococcus aureus likely already existed at the time.[5][35]
Manufacturing
When production first began one-liter containers would have a yield of less than 1% to a yield of 80–90% in 10,000 gallon containers. This increase in efficiency happened between 1939 and 1945 due to continuous innovation of the process. Orvill May, the Director of the Agricultural Research Service had Robert Coghill, who was the Chief of the Fermentation Division, used his experience with fermentation to increase the efficiency of extracting penicillin from the mold. Shorty after beginning Andrew Moyer replaced sucrose with lactose in the growth media, which resulted in an increased yield. An even larger increase occurred when Moyer added corn steep liquor.[26]
One major issue with the process that British scientists had was the inefficiency of growing the mold on the surface of their nutrient baths, rather than having it submerged. Even though a submerged process of growing the mold would be more efficient, the strain used was not suitable for the conditions it would require. This led to a search for a strain that had already adapted to work. A cantaloupe in a Peoria marketplace ended up being the best they could find.[36] In order to try and improve upon that strain they subjected it with X-rays to facilitate mutations in its genome and managed to increase it production capabilities even more.[37][38]
Now that scientists had a mold that grew well submerged and produced an acceptable amount of penicillin the next problem to tackle was providing the required air to the mold for it to grow. This was solved using an aerator, but that caused severe foaming due to the corn steep which was solved by the introduction of an anti-foaming agent known as glyceryl monoricinoleate.[39]
Penicillin Resistance
In 1940, Ernst Chain and Edward Abraham reported the first indication of antibiotic resistance to penicillin, an E. coli strain that produced the penicillinase enzyme, which was capable of breaking down penicillin and completely negating its antibacterial effect.[5][6][40] In 1942, strains of Staphylococcus aureus had been documented to have developed a strong resistance to penicillin. Most of the strains were resistant to penicillin by the 1960s.[41] In 1967, Streptococcus pneumoniae was also reported to be penicillin resistant. Many strains of bacteria have developed a resistance to penicillin.
Notes
- At the time, the term Penicillium glaucum was used as a catch-all phrase for a variety of different fungi, though not for Penicillium notatum. Duchesne's specific mold was unfortunately not preserved, which makes it impossible to be certain today which fungus might have been responsible for the cure and, consequently, even less certain which specific antibacterial substance was responsible.
References
- "Alexander Fleming". Science History Institute. June 2016. Retrieved 21 August 2018.
- "Discovery and Development of Penicillin". International Historic Chemical Landmarks. American Chemical Society. Retrieved 21 August 2018.
- Macfarlane, Gwyn (1984). Alexander Fleming, the man and the myth. Cambridge, Mass.: Harvard University Press.
- Barreiro, Carlos; Martín, Juan F.; García-Estrada, Carlos (2012). "Proteomics Shows New Faces for the Old Penicillin Producer". Journal of Biomedicine and Biotechnology. 2012: 105109. doi:10.1155/2012/105109. PMC 3270403. PMID 22318718.
- Davies, J.; Davies, D. (30 August 2010). "Origins and Evolution of Antibiotic Resistance". Microbiology and Molecular Biology Reviews. 74 (3): 417–433. doi:10.1128/MMBR.00016-10. PMC 2937522. PMID 20805405.
- Lobanovska, M; Pilla, G (March 2017). "Penicillin's Discovery and Antibiotic Resistance: Lessons for the Future?". The Yale Journal of Biology and Medicine. 90 (1): 135–145. PMC 5369031. PMID 28356901.
- "History of Antibiotics | Steps of the Scientific Method, Research and Experiments". Experiment-Resources.com. Retrieved 13 July 2012.
- Andrzej Nowak; Maciej Nowak; Krystyna Cybulska. "Stories with microorganisms".
- Shama, Gilbert (September 2016). "La Moisissure et la Bacterie: Deconstructing the fable of the discovery of penicillin by Ernest Duchesne". Endeavour. 40 (3): 193. doi:10.1016/j.endeavour.2016.07.005. PMID 27496372.
- MacFarlane, Gwyn (1979). Howard Florey : the making of a great scientist. Oxford: Oxford Univ. Pr. pp. 14–15. ISBN 978-0198581611.
- Douglas Allchin. "Penicillin & Chance". SHiPS Resource Center. Archived from the original on 28 May 2009. Retrieved 9 February 2010.
- "penicillin". New age Encyclopedia. Retrieved 8 March 2019.
- 'At once Pasteur jumped to a fine idea: “If the harmless bugs from the air choke out the anthrax bacilli in the bottle, they will do it in the body too! It is a kind of dog-eat-dog!” shouted Pasteur, (...) Pasteur gravely announced: “That there were high hopes for the cure of disease from this experiment,” but that is the last you hear of it, for Pasteur was never a man to give the world of science the benefit of studying his failures.'
- Tiberio, Vincenzo (1895) "Sugli estratti di alcune muffe" [On the extracts of certain moulds], Annali d'Igiene Sperimentale (Annals of Experimental Hygiene), 2nd series, 5 : 91–103. From p. 95: "Risulta chiaro da queste osservazioni che nella sostanza cellulare delle muffe esaminate son contenuti dei principi solubili in acqua, forniti di azione battericida: sotto questo riguardo sono più attivi o in maggior copia quelli dell' Asp. flavescens, meno quelli del Mu. mucedo e del Penn. glaucum." (It follows clearly from these observations that in the cellular substance of the moulds examined are contained some water-soluble substances, provided with bactericidal action: in this respect are more active or in greater abundance those of Aspergillus flavescens; less, those of Mucor mucedo and Penicillium glaucum.)
- Bucci R., Galli P. (2011) "Vincenzo Tiberio: a misunderstood researcher," Italian Journal of Public Health, 8 (4) : 404–406. (Accessed 1 May 2015)
- "Almanacco della Scienza CNR". Almanacco.rm.cnr.it. 2 March 2011. Retrieved 13 July 2012.
- Salvatore De Rosa, Introduttore: Fabio Pagan. "Vincenzo Tiberio, vero scopritore degli antibiotici – Festival della Scienza" (in Italian). Festival2011.festivalscienza.it. Retrieved 13 July 2012.
- Duchesne 1897, Antagonism between moulds and bacteria. An English translation by Michael Witty. Fort Myers, 2013. ASIN B00E0KRZ0E and B00DZVXPIK.
- Ernest Duchesne, Contribution à l'étude de la concurrence vitale chez les micro-organismes : antagonisme entre les moisissures et les microbes [Contribution to the study of the vital competition in microorganisms: antagonism between moulds and microbes], (Lyon, France: Alexandre Rey, 1897).
- Une découverte oubliée : la thèse de médecine du docteur Ernest Duchesne (1874–1912)
- Arseculeratne, S. N.; Arseculeratne, G. (May 2017). "A re-appraisal of the conventional history of antibiosis and Penicillin". Mycoses. 60 (5): 343–347. doi:10.1111/myc.12599. PMID 28144986.
- Lobanovska, Mariya; Pilla, Giulia (March 2017). "Penicillin's Discovery and Antibiotic Resistance: Lessons for the Future?". Yale Journal of Biology and Medicine. 90 (1): 135–145. PMC 5369031. PMID 28356901.
- Bowden, Mary Ellen (2018). "Old Brew, New Brew". Distillations. 4 (2): 8–11. Retrieved 21 August 2018.
- Arseculeratne, S. N.; Arseculeratne, G. (May 2017). "A re-appraisal of the conventional history of antibiosis and Penicillin". Mycoses. 60 (5): 343–347. doi:10.1111/myc.12599. PMID 28144986.
- Wainwright M, Swan HT (January 1986). "C.G. Paine and the earliest surviving clinical records of penicillin therapy". Med Hist. 30 (1): 42–56. doi:10.1017/S0025727300045026. PMC 1139580. PMID 3511336.
- "Discovery and Development of Penicillin: International Historic Chemical Landmark". Washington, D.C.: American Chemical Society. Archived from the original on 28 June 2019. Retrieved 15 July 2019.
- (1) "Penicillium chrysogenum (aka P. notatum), the natural source for the wonder drug penicillin, the first antibiotic". Tom Volk's Fungus of the Month for November 2003.
(2) "Historic Peoria, Illinois". Northern Regional Research Lab. - Stuart B. Levy, The Antibiotic Paradox: How the Misuse of Antibiotics Destroys Their Curative Powers, Da Capo Press, 2002: pp. 5–7. ISBN 0-7382-0440-4
- "1900–1950". Exploring Our History. Pfizer Inc. 2009. Retrieved 2 August 2009.
- "Penicillin X-ray data showed that proposed β-lactam structure was right". C&EN. Retrieved 21 August 2018.
- HODGKIN, D. C. (July 1949). "The X-ray analysis of the structure of penicillin". Advancement of Science. 6 (22): 85–89. PMID 18134678.
- Curtis, Rachel; Jones, John (2007). "Robert Robinson and penicillin: an unnoticed document in the saga of its structure". Journal of Peptide Science. 13 (12): 769–775. doi:10.1002/psc.888. PMID 17890642.
- "Serie Forschung und Industrie: Sandoz". Medical Tribune (in German) (45/2005). Retrieved 2 August 2009.
- E. J. Corey; John D. Roberts. "Biographical Memoirs: John Clark Sheehan". The National Academy Press. Retrieved 28 January 2013.
- Harkins, Catriona P.; Pichon, Bruno; Doumith, Michel; Parkhill, Julian; Westh, Henrik; Tomasz, Alexander; de Lencastre, Herminia; Bentley, Stephen D.; Kearns, Angela M.; Holden, Matthew T. G. (20 July 2017). "Methicillin-resistant Staphylococcus aureus emerged long before the introduction of methicillin into clinical practice". Genome Biology. 18 (1): 130. doi:10.1186/s13059-017-1252-9. PMC 5517843. PMID 28724393.
- Mestrovic, Tomislav. "Penicillin Produciton". Retrieved 2 May 2019.
- "Alexander Fleming Discovery and Development of Penicillin – Landmark". American Chemical Society. Retrieved 18 March 2019.
- Mestrovic, Tomislav. "Penicillin Produciton". Retrieved 2 May 2019.
- "Alexander Fleming Discovery and Development of Penicillin – Landmark". American Chemical Society. Retrieved 18 March 2019.
- Abraham, EP; Chain, E (1940). "An enzyme from bacteria able to destroy penicillin". Reviews of Infectious Diseases. 10 (4): 677–678. Bibcode:1940Natur.146..837A. doi:10.1038/146837a0. PMID 3055168.
- Lowy, Franklin (1 May 2013). "Antimicrobial resistance: the example of Staphylococcus aureus". The Journal of Clinical Investigation. 111 (9): 1265–1273. doi:10.1172/JCI18535. PMC 154455. PMID 12727914.
Further reading
- Bud, Robert (2007). Penicillin: Triumph and Tragedy. Oxford: Oxford University Press. ISBN 9780199254064.
- Brown, Kevin W. (St Mary's Trust Archivist and Alexander Fleming Laboratory Museum Curator) (2004). Penicillin man: Alexander Fleming and the antibiotic revolution. Scarborough, Ont: Sutton Pub. ISBN 978-0-7509-3152-6.
External links
- History of Antibiotics, archived from the original on 14 May 2002, retrieved 6 August 2013, from a course offered at Princeton University
- Debate in the House of Commons on the history and the future of the discovery