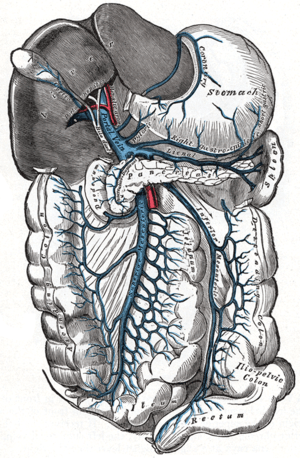
Hepatic portal system
In human anatomy, the hepatic portal system is the system of veins comprising the hepatic portal vein and its tributaries. It is also called the portal venous system (although it is not the only example of a portal venous system) and splanchnic veins, which is not synonymous with hepatic portal system and is imprecise (as it means visceral veins and not necessarily the veins of the abdominal viscera).[1]
| Hepatic portal system | |
|---|---|
 The hepatic portal vein and its territory | |
| Details | |
| Location | Abdomen |
| Anatomical terminology | |
Structure
Large veins that are considered part of the portal venous system are the:
The superior mesenteric vein and the splenic vein come together to form the actual hepatic portal vein. The inferior mesenteric vein connects in the majority of people on the splenic vein, but in some people, it is known to connect on the portal vein or the superior mesenteric vein.
Roughly, the portal venous system corresponds to areas supplied by the celiac trunk, the superior mesenteric artery, and the inferior mesenteric artery.
Function
The portal venous system is responsible for directing blood from parts of the gastrointestinal tract to the liver. Substances absorbed in the small intestine travel first to the liver for processing before continuing to the heart. Not all of the gastrointestinal tract is part of this system. The system extends from about the lower portion of the esophagus to the upper part of the anal canal. It also includes venous drainage from the spleen and pancreas.
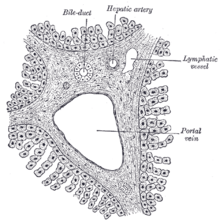
Blood flow to the liver is unique in that it receives both oxygenated and (partially) deoxygenated blood. As a result, the partial gas pressure of oxygen (pO2) and perfusion pressure of portal blood are lower than in other organs of the body. Blood passes from branches of the portal vein through cavities between "plates" of hepatocytes called sinusoids. Blood also flows from branches of the hepatic artery and mixes in the sinusoids to supply the hepatocytes with oxygen. This mixture percolates through the sinusoids and collects in a central vein which drains into the hepatic vein. The hepatic vein subsequently drains into the inferior vena cava.
The hepatic artery provides 30 to 40% of the oxygen to the liver, while only accounting for 25% of the total liver blood flow. The rest comes from the partially deoxygenated blood from the portal vein. The liver consumes about 20% of the total body oxygen when at rest. That is why the total liver blood flow is quite high, at about 1 litre a minute and up to two litres a minute. That is on average one fourth of the average cardiac output at rest.
Clinical significance
Portal hypertension is a condition in which the blood pressure of the portal venous system is too high. It is often the result of cirrhosis of the liver.
Drug metabolism
Many drugs that are absorbed through the GI tract are substantially metabolized by the liver before reaching general circulation. This is known as the first pass effect. As a consequence, certain drugs can only be taken via certain routes. For example, nitroglycerin cannot be swallowed because the liver would deactivate the medication, but it can be taken under the tongue or transdermally (through the skin) and thus is absorbed in a way that bypasses the portal venous system. Inversely, dextromethorphan, a cough suppressor, is best taken orally because it needs to be metabolised by the liver into dextrorphan in order to be effective. This latter principle is that of most prodrugs.
The use of suppositories is a way to bypass partially the portal vein: the upper 1/3 of the rectum is drained into the portal vein while the lower 2/3 are drained into the internal iliac vein that goes directly in the inferior vena cava (thus bypassing the liver).
References
- Splanchnic circulation. Online Medical Dictionary. URL: http://cancerweb.ncl.ac.uk/cgi-bin/omd?splanchnic+circulation. Accessed on: October 22, 2008.