Butalbital
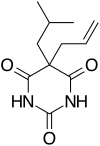
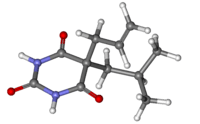
Butalbital is a barbiturate with an intermediate duration of action. Butalbital is often combined with other medications, such as paracetamol (acetaminophen) or aspirin, for the treatment of pain and headache. The various formulations combined with codeine are FDA-approved for the treatment of tension headaches. Butalbital has the same chemical formula as talbutal but a different structure—one that presents as 5-allyl-5-isobutylbarbituric acid.[2] Its use for headaches is discouraged (except as a last resort) due to its toxicity and the availability of safer agents.[3]
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a601009 |
| Pregnancy category |
|
| Routes of administration | oral |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 20-45% |
| Metabolism | hepatic mainly CYP3A4 |
| Elimination half-life | 35 hours [1] |
| Excretion | renal |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.926 |
| Chemical and physical data | |
| Formula | C11H16N2O3 |
| Molar mass | 224.260 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
| (verify) | |
Preparations
Combinations include:
- Butalbital and acetaminophen (paracetamol) (trade names: Axocet, Bucet, Bupap, Cephadyn, Dolgic, Phrenilin,Forte, Sedapap)
- Butalbital, paracetamol (acetaminophen), and caffeine (trade names: Fioricet, Esgic, Esgic-Plus)
- Butalbital and aspirin (trade name: Axotal)
- Butalbital, aspirin, and caffeine (trade names Fiorinal, Fiormor, Fiortal, Fortabs, Laniroif)
- Butalbital, paracetamol (acetaminophen), caffeine, and codeine phosphate (Fioricet#3 with Codeine)
- Butalbital, aspirin, caffeine, and codeine phosphate (trade name: Fiorinal#3 with Codeine)
- Ergotamine tartrate, caffeine, butalbital, belladonna alkaloids (trade name: Cafergot-PB)
Contraindications
Butalbital is not suggested as a first-line treatment for headache because it impairs alertness, brings risk of dependence and addiction, and increases the risk that episodic headaches will become chronic.[3] When all other treatments fail or are unavailable, butalbital (or narcotics) may be appropriate for treating headache if the patient can be monitored to prevent the development of chronic headache.[3]
There are specific treatments which are appropriate for targeting migraines and headaches which are preferable to butalbital when available as an option.[4] It is a least preferable option to be used if other available treatments fail.[4]
Side effects
Side effects for any psychoactive drug are difficult to predict, though butalbital is usually well tolerated. Commonly reported side effects for butalbital, some of which tend to subside with continued use, include:
|
 Fioricet (50/40/325) |
Rare side-effects include Stevens–Johnson syndrome, an adverse reaction to barbiturates, and anaphylaxis.
The risk and severity of all side effects is greatly increased when butalbital (or butalbital-containing medications) are combined with other sedatives (ex. ethanol, opiates, benzodiazepines, antihistamines). In particular, butalibital, especially when combined with other sedatives (e.g. opioids), can cause life-threatening respiratory depression and death. Inhibitors of the hepatic enzyme CYP3A4 may also increase the risk, severity, and duration of side effects, many drugs inhibit this enzyme as do some foods such as grapefruit and the blood orange. Taking butalbital-based medications with some other drugs may also increase the side effects of the other medication.
Dangers and risks
Butalbital can cause dependence and/or addiction. Mixing with alcohol increases the risk of intoxication, increases respiratory depression, and increases liver toxicity when the butalbital is in combination with paracetamol (acetaminophen). Many opioid-dependent persons frequently use barbiturates as a potentiator to their normal dose of opiates in order to increase the effects, or with a less than normal dose as means of conserving their supply. Especially when used with the stronger narcotics, suicide or accidental death occurs much more frequently than first reported with one drug alone. Use of alcohol, benzodiazepines, and other CNS-depressants often also contribute to respiratory depression, coma, and in extreme cases fatality.
When benzodiazepines are co-administered with barbiturates, the sum effect of the drugs is far greater than would be expected considering the effect of both drugs separately. This is due to complementary mechanisms at the GABAA receptor, where benzodiazepines increase the rate of chloride channel opening while barbiturates increase the duration. A dose of a benzodiazepine causes a channel which normally opens once every 30 seconds to open 3 times faster, while a barbiturate causes the channel to pass three chloride ions per opening instead of the normal one. When combined, the channel is now passing nine ions every 30 seconds instead of one, a 9-fold increase in activity.
As with most barbiturates, butalbital is a general inducer of P450 enzymes in both rodents and humans, particularly CYP3A4 (hence inducing its own metabolism), CYP2D6, and CYP2C9, although its P450 enzyme induction capability is far less than that of equivalent doses of phenobarbital or secobarbital (the most potent known enzyme inducers in the barbiturate molecular family). At very high doses it has also been demonstrated to induce glutathione S-transferase A1/glutathione S-transferase A2 in rats, although the doses required to achieve this effect to a clinically significant degree fall within the range of butalbital's LD50, making its use for this purpose impractical and highly dangerous (this effect has not yet been tested in human models, it is therefore unknown whether or not GS-T induction plays a significant role in butalbital's effects in humans, or even occurs at all).
References
- "Butalbital and Acetaminophen - FDA prescribing information, side effects and uses". drugs.com. Archived from the original on 2018-01-21.
- DE Patent 526854
- American Headache Society (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Headache Society, archived from the original on 3 December 2013, retrieved 10 December 2013, which cites
- Bigal, M. E.; Lipton, R. B. (2009). "Excessive opioid use and the development of chronic migraine". Pain. 142 (3): 179–182. doi:10.1016/j.pain.2009.01.013. PMID 19232469.
- Bigal, M. E.; Serrano, D.; Buse, D.; Scher, A.; Stewart, W. F.; Lipton, R. B. (2008). "Acute Migraine Medications and Evolution from Episodic to Chronic Migraine: A Longitudinal Population-Based Study". Headache: The Journal of Head and Face Pain. 48 (8): 1157–1168. doi:10.1111/j.1526-4610.2008.01217.x. PMID 18808500.
- Scher, A. I.; Stewart, W. F.; Ricci, J. A.; Lipton, R. B. (2003). "Factors associated with the onset and remission of chronic daily headache in a population-based study". Pain. 106 (1–2): 81–89. doi:10.1016/S0304-3959(03)00293-8. PMID 14581114.
- Katsarava, Z.; Schneeweiss, S.; Kurth, T.; Kroener, U.; Fritsche, G.; Eikermann, A.; Diener, H. C.; Limmroth, V. (2004). "Incidence and predictors for chronicity of headache in patients with episodic migraine". Neurology. 62 (5): 788–790. doi:10.1212/01.WNL.0000113747.18760.D2. PMID 15007133.
- American Academy of Neurology (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Academy of Neurology, archived from the original on September 1, 2013, retrieved August 1, 2013, which cites
- Silberstein, S. D. (2000). "Practice parameter: Evidence-based guidelines for migraine headache (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 55 (6): 754–762. doi:10.1212/WNL.55.6.754. PMID 10993991.
- Evers, S.; Afra, J.; Frese, A.; Goadsby, P. J.; Linde, M.; May, A.; Sándor, P. S.; European Federation of Neurological Societies (2009). "EFNS guideline on the drug treatment of migraine - revised report of an EFNS task force". European Journal of Neurology. 16 (9): 968–981. doi:10.1111/j.1468-1331.2009.02748.x. PMID 19708964.
- Institute for Clinical Systems Improvement (2011), Headache, Diagnosis and Treatment of, Institute for Clinical Systems Improvement, archived from the original on 2013-10-29
External links
"Butalbital". On-line Medical Dictionary. Retrieved June 26, 2005. "Butalbital and Acetaminophen (Systemic)". MedicinePlus Drug Information. Archived from the original on December 30, 2006. Retrieved December 31, 2006. "Controlled Substances in Schedule III". Drug Enforcement Administration. 2007. Archived from the original on 2007-02-02. Retrieved 2007-01-13.