Fibrothorax
Fibrothorax is a medical condition characterised by severe scarring (fibrosis) and fusion of the layers of the pleural space surrounding the lungs resulting in decreased movement of the lung and ribcage.[1] The main symptom of fibrothorax is shortness of breath. There also may be recurrent fluid collections surrounding the lungs. Fibrothorax may occur as a complication of many diseases, including infection of the pleural space known as an empyema or bleeding into the pleural space known as a haemothorax.[2]
| Fibrothorax | |
|---|---|
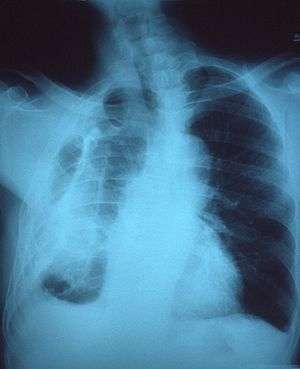 | |
| Fibrothorax on chest x-ray | |
| Specialty | Respiratory medicine |
| Symptoms | Breathlessness |
| Usual onset | Adulthood |
| Duration | Long Term |
| Causes | Haemothorax, empyema, tuberculosis, collagen vascular diseases, uraemia, rheumatoid arthritis, pleurodesis, pleural effusion, certain medications |
| Risk factors | Asbestos exposure |
| Diagnostic method | Chest X-ray, CT scan |
| Treatment | Watchful waiting, decortication |
| Prognosis | Variable |
| Frequency | Rare |
Fibrosis in the pleura may be produced intentionally using a technique called pleurodesis to prevent recurrent punctured lung (pneumothorax), and the usually limited fibrosis that this produces can rarely be extensive enough to lead to fibrothorax.[3] The condition is most often diagnosed using an X-ray or CT scan, the latter more readily detecting mild cases. Fibrothorax is often treated conservatively with watchful waiting but may require surgery. The outlook is usually good as long as there is no underlying pulmonary fibrosis or complications following surgery. The disease is highly uncommon.
Signs and symptoms
Signs
Common signs observed during examination for fibrothorax include reduced movement of the ribcage during breathing, reduced breath sounds on the affected side(s), and a dull feeling when the chest is pressed.[4]
.png)
Symptoms
The condition only causes symptoms if the visceral pleura is affected.[5] Although fibrothorax may not cause any symptoms, the most common symptom associated with this condition is shortness of breath. Persistent, recurrent pleural effusions are a possible symptom, caused by the persistent cavity formed by the hardening pleura around the original fluid collection.[4] Shortness of breath tends to develop gradually and may worsen over time. Less commonly, fibrothorax may cause chest discomfort or a dry cough.[4] As fibrothorax may occur as a complication of other diseases, symptoms are sometimes seen which reflect the underlying problem, for example fever in cases of empyema.
Causes
Fibrothorax is often a complication of other diseases that cause inflammation of the pleura. These include infections such as empyema or tuberculosis, or bleeding within the pleural space known as a haemothorax. It may also be caused by exposure to certain substances such as asbestos which can cause generalised fibrosis of the lungs which may involve the pleura.[6] Less common causes of fibrothorax include collagen vascular diseases such as systemic lupus erythematosus, sarcoidosis, and rheumatoid arthritis; kidney failure leading to uraemia; and side effects of certain medications.[3][7] The medications most commonly associated with pleural fibrosis are the ergot alkaloids bromocriptine, pergolide, and methysergide.[3] Fibrothorax may also occur without a clear underlying cause, in which case it is known as idiopathic fibrothorax.
A technique called pleurodesis can be used to intentionally create scar tissue within the pleural space, usually as a treatment for repeated episodes of a punctured lung, known as a pneumothorax, or for malignant pleural effusions. While this procedure usually generates only limited scar tissue, in rare cases a fibrothorax can develop.[8]
Mechanism
Fibrosis can affect one or both of the two layers of tissue forming the pleura—the visceral pleura adjacent to the lung and the parietal pleura adjacent to the ribcage. The term fibrothorax implies severe fibrosis affecting both the visceral and parietal pleura, fusing the lung to the chest wall.[2] The condition starts as a pleural effusion that has not been drained. Over time, the undrained pleural effusion causes sustained inflammation of the pleura, which can then lead to deposition of fibrin in the pleura and the development of a fibrotic scar. Eventually, a "peel" that is rich in collagen is formed around the fluid collection. From this point, the illness can no longer be treated with thoracentesis, since the fluid will return to the cavity maintained by the peel.[4] Over time, generally over the course of years, the fibrotic scar tissue slowly tightens and thickens, contracting the contents of one or both halves of the chest and reducing the mobility of the ribs. The peel can become deeper than 2 cm.[2] Within the chest, the lung is compressed and unable to expand (trapped lung), making it vulnerable to collapse and causing breathlessness.[6]
Microscopic
At the microscopic level, the scar tissue is composed of collagen fibres deposited in a basket weave pattern.[6] Usually, the underlying condition has to cause intense inflammation of the pleura, though it is unclear exactly how this results in fibrosis. It is suspected that a protein called Transforming Growth Factor beta (TGF-β) plays a key role in producing fibrothorax, as this cellular chemical signal induces pleural fibrosis when given to animals. Furthermore, anti-TGF-β antibodies prevent fibrothorax in empyema.[3]
Diagnosis
Fibrothorax can be detected on a plain chest X-ray.[6] Thickening of the pleura that surround the lungs can be seen which, if severe, may also restrict the lung on the affected side causing a loss of lung volume.[6] A CT scan or chest X-ray may also detect calcification of the thickened pleura.[6] There may be signs of the causative disease, such as upper lobe consolidation in cases of tuberculosis.[9] Features similar to those seen on a plain X-ray can also be found on a CT scan.[6]
 Extensive left-sided fibrothorax
Extensive left-sided fibrothorax Chest radiograph displaying inhomogeneous opacification of the left half of the chest that is fibrothorax
Chest radiograph displaying inhomogeneous opacification of the left half of the chest that is fibrothorax
 Autopsy specimen showing extensive pleural fibrosis
Autopsy specimen showing extensive pleural fibrosis
Treatment
Conservative
Conservative treatment of fibrothorax is generally done by treating its underlying cause and is reserved for milder cases. In cases of fibrothorax caused by medication, it is recommended that the offending medications be stopped. Some cases of fibrothorax can then be treated conservatively by watchful waiting, as fibrothorax caused by tuberculosis, empyema, or haemothorax often improves spontaneously 3–6 months after the precipitating illness. During this time, medications that might cause fibrosis to worsen such as ergot alkaloids should be avoided.[3] Tobacco smoking cessation is strongly recommended, since tobacco smoke exposure can worsen fibrosis.[10]
Surgical
In severe cases of fibrothorax that are compromising a person's ability to breathe, the scar tissue causing fibrothorax can be surgically removed using a technique called decortication.[1][6] However, surgical decortication is an invasive procedure which carries the risk of complications including a small risk of death,[6] and is therefore generally only considered if severe symptoms are present and have been for many months.[3] The relative effectiveness of conservative treatment versus surgical decortication is unclear.[9] A pleurectomy can be done in a progressive case that fails to resolve, as often happens when asbestosis is the cause.[11]
Prognosis
Fibrothorax complicating another condition, such as tuberculous pleuritis, empyema, or acute haemothorax often spontaneously resolves in 3-6 months.[3]
The prognosis of decortication is typically good if the affected person is otherwise healthy. The mortality of surgery is less than 1% overall, but rises to 4-6% in the elderly. Other factors predicting poorer surgical outcomes include intraoperative complications, incomplete surgery, lung disease beyond the fibrothorax being treated, and specific causes of fibrothorax such as asbestosis.[11]
Epidemiology
Though sporadic cases have been reported in the medical literature, for example due to iatrogenic or postoperative complications, fibrothorax is rare in developed countries, mainly due a lower incidence of tuberculosis. The condition is far more common in workers exposed to asbestos, with 5–13.5% of those exposed subsequently developing some degree of pleural fibrosis, sometimes not diagnosed until decades after the initial exposure.[10]
References
- Jantz, MA; Antony, VB (June 2006). "Pleural fibrosis". Clinics in Chest Medicine. 27 (2): 181–91. doi:10.1016/j.ccm.2005.12.003. PMID 16716812.
- Huggins JT, Sahn SA (2004). "Causes and management of pleural fibrosis". Respirology. 9 (4): 441–7. doi:10.1111/j.1440-1843.2004.00630.x. PMID 15612954.
- Broaddus, CV; Mason, RC; Ernst, JD; King, TE; Lazarus, SC; Murray, JF; Nadel, JA; Slutsky, A; Gotway, M (2015-03-17). Murray & Nadel's Textbook of Respiratory Medicine E-Book (5 ed.). Elsevier Health Sciences. pp. 1785–6. ISBN 978-0-323-26193-7.
- Birdas, Thomas J.; Keenan, Robert J. (2009). Sugarbaker, David J.; Bueno, Raphael; Krasna, Mark J.; Mentzer, Steven J.; Zellos, Lambros (eds.). Adult Chest Surgery. New York, NY: The McGraw-Hill Companies.
- Huggins, John T.; Sahn, Steven A. (2004). "Causes and management of pleural fibrosis". Respirology. 9 (4): 441–447. doi:10.1111/j.1440-1843.2004.00630.x. ISSN 1440-1843. PMID 15612954.
- Donath, Joseph; Miller, Albert (2009). "Restrictive Chest Wall Disorders". Seminars in Respiratory and Critical Care Medicine. 30 (3): 275–292. doi:10.1055/s-0029-1222441. ISSN 1069-3424. PMID 19452388.
- Alhassan, Sulaiman; Fasanya, Adebayo; Thirumala, Raghu (2017-02-15). "Extensive Calcified Fibrothorax". American Journal of Respiratory and Critical Care Medicine. 195 (4): e25–e26. doi:10.1164/rccm.201606-1265im. PMID 27854506.
- "Clinical Respiratory Medicine | ScienceDirect". www.sciencedirect.com. Retrieved 2019-12-02.
- "Fibrothorax – an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2018-03-29.
- "Pleural Thickening of Lungs: Causes, Symptoms & Treatment". Mesothelioma Center – Vital Services for Cancer Patients & Families. Retrieved 2018-05-28.
- Moore, Jason (2015). "Fibrothorax". Encyclopedia of Trauma Care. Springer, Berlin, Heidelberg. pp. 616–618. doi:10.1007/978-3-642-29613-0_130. ISBN 978-3-642-29611-6.